Screening for Endometrial Cancer
advertisement

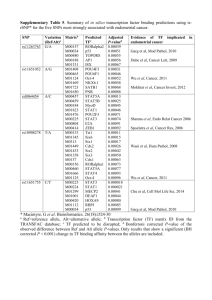
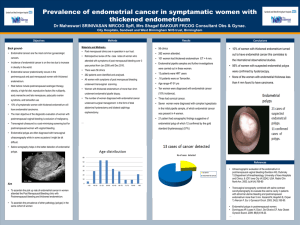
Screening for Cancer in Women Endometrial Cancer Screening…? Organized identification High coverage of a target population Continuous quality assessment. Feasibility of treatment & follow up Of a pre - clinical disease state By a test that is repeated at a given interval OR… Screening can be defined as The application of diagnostic tests or procedures To asymptomatic people For the purpose of dividing them into two groups: • those who have a condition that would benefit from early intervention • and those who do not. Early diagnosis alone does not justify a screening program. The only justification is early diagnosis that leads to a measurable improvement in outcome. The Number Needed to Screen(NNS) is the number of asymptomatic women who must be enrolled in a screening program over a given period of time to prevent one death from the disease in question. The NNS reflects both the prevalence of the disease and the effectiveness of therapy, and has the advantage of being easy to calculate and intuitively useful to clinicians and patients. An Ideal Screening Program… Features of the disease Significant impact on public health Asymptomatic period during which detection is possible Outcomes improved by treatment during asymptomatic period Features of the test Sufficiently sensitive to detect disease during asymptomatic period Sufficiently specific to minimize false-positive test results Acceptable to patients Features of the screened population Sufficiently high prevalence of the disease to justify screening Relevant medical care is accessible Patients willing to comply with further work-up and treatment To screen or To screen not ? Recommended Screening Cervical Carcinoma Not yet , for… Ovarian Cancer Bronchogenic Carcinoma Breast Carcinoma Skin cancer Oral Cancer Colorectal Carcinoma Endometrial Cancer Effective Screening Program Should be tailored to suit the principles for national cancer control programs. We Should NOT copy other’s programs... Otherwise… Too much money & effort will be spent with minimal impact on the incidence & mortality from the disease. Endometrial Cancer Adenocarcinoma is the most common cancer of the female reproductive tract. 2-3% of women will develop it in a lifetime. 75% occur in postmenopausal women. Associated with the best overall survival of all gynecologic malignancies. Usually diagnosed as early stage disease. Endometrial Hyperplasia (EMHP) The majority of the simple and complex EMHPs will regress spontaneously. Atypical HP has a much greater tendency to persist or progress if not specifically treated. Lesions are classified as invasive or pre-invasive according to the presence or absence of stromal invasion. EMHP - Tendency for Progression Hyperplasia Regression Progression Yrs. Simple HP 80% 1% Complex HP 78% 3% 8.3 Atypical HP * 58% 29% 4.1 * true cancer precursor Risk Factors for Endometrial Cancer •Unopposed estrogen exposure •Median age at diagnosis: 59 years •Menstrual cycle irregularities, specifically menorrhagia and menometrorrhagia •Postmenopausal bleeding •Chronic anovulation •Nulliparity •Early menarche (before 12 years) / Late menopause (after 52 years) •Infertility •Tamoxifen (Nolvadex) use •Granulosa and thecal cell tumors •Ovarian dysfunction •Obesity •Diabetes mellitus •Arterial hypertension with or without atherosclerotic heart disease •History of breast or colon cancer Risk factors: Unopposed Estrogen May accelerate the progression from Simple Atypical Cancer Simple or atypical HP will regress if unopposed estrogen is stopped. Users of unopposed estrogen for at least 2 years develop endometrial cancer 2 - 20 times more frequently than nonusers. Risk increases with higher doses and longer use. Risk factors: Unopposed Estrogen After 10 years of use, the risk of developing endometrial cancer = 10 per 1000 postmenopausal women. There is a residual risk that may persist for up to 15 years even after estrogen is stopped. Tamoxifen use??? Risk factors: Prolonged Endogenous Estrogen Primarily due to chronic anovulation. Obesity. Polycystic ovarian disease. Infertility. Late menopause. Explains why smokers have a decreased risk of endometrial cancer. Endometrial Cancer Vaginal bleeding is the most common presenting symptom. Gross and microscopic hemorrhage. Most common histologic types are endometrial and mucinous. Most common prognostic factors: Degree of histologic differentiation. Depth of stromal invasion. Methods of Detection:Endometrial Cancer Endometrial cells on the Pap Smear Endometrial cells HP Adenocarcinoma Normal 13% 11% Atypical 11% 20% Of women with Malignant endometrial cells on a Pap smear, 70% have deep myometrial invasion. Do not ignore endometrial cells on a Pap smear ! Methods of Detection:Endometrial Cancer Endometrial Aspiration Office endometrial samplers are highly sensitive ( 97.5 % or more ) for detection of endometrial cancer. • misses polyps and submucous fibroids. May fail to adequately sample the atrophic endometrium. • insufficiency rate = 15 %. • samples by “shear” rather than curettage. Methods of Detection:Endometrial Cancer Ultrasonography The thicker the endometrial lining of postmenopausal women on TVUS, the greater the risk of endometrial disease. The negative predictive value for the diagnosis of cancer or HP is 100 % when the lining measures < 5 mm in thickness. • Does not apply if EMBx has been previously performed. Saline Contrast Sonography Allows a better evaluation of the endometrium specially in case of TAM therapy or if there is a ? Endometrial polyp or Fibroid Methods of Detection:Endometrial Cancer Hysteroscopy The combination of Hysteroscopy and Guided Biopsy can approach 100 % accuracy in the diagnosis of endometrial cancer and HP. Used to stage the tumor. • Confined to uterine corpus ? • Cervical involvement ? – Errors in staging can occur 10-15% of the time with blind D&C . Four Major Types of Pathologic Findings on Endometrial Biopsy •Proliferative, secretory, benign or atrophic endometrium •Simple or complex (adenomatous) hyperplasia without atypia •Simple or complex (adenomatous) hyperplasia with atypia •Endometrial adenocarcinoma Regardless of histologic type, the presence of atypia is the major determinant of risk for endometrial cancer. Management of Hyperplasia Without Atypia 6mm. POLYP from the fundus 3-D ultrasound-Endometrial polyp Screening…To whom it should be directed All women with postmenopausal bleeding (except in the first 6 months of HRT). Perimenopausal women at high risk or with persistent AUB despite hormonal therapy. Women at any age at high risk for EMHP. Obese women with AUB. Women with DUB not responding to hormonal therapy. Women on tamoxifen therapy.