Exercise and Heart Failure
advertisement

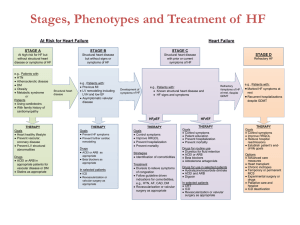
Exercise and Heart Failure Tami Ward MS, APRN, NP-C, CHFN October 10, 2013 I have no conflict of interest Discuss reduced ejection fraction(HFrEF) and preserved ejection fraction (HFpEF) heart failure Examine the role and recommendations of exercise training in heart failure (HF) Identify barriers and strategies to overcome these barriers in the HF population Objectives The definition of HF has now expanded to: a. HF with reduced ejection fraction (HFrEF, EF≤40%) b. HF failure with preserved ejection fraction (HFpEF EF ≥50%) c. HFpEF, borderline (EF 41-49%) d. HFpEF, improved (EF >40%) Two Types of HF Definition of Heart Failure Classification I. Heart Failure with Reduced Ejection Fraction (HFrEF) Ejection Fraction ≤40% Description Also referred to as systolic HF. Randomized clinical trials have mainly enrolled patients with HFrEF and it is only in these patients that efficacious therapies have been demonstrated to date. ≥50% Also referred to as diastolic HF. Several different criteria have been used to further define HFpEF. The diagnosis of HFpEF is challenging because it is largely one of excluding other potential noncardiac causes of symptoms suggestive of HF. To date, efficacious therapies have not been identified. a. HFpEF, Borderline 41% to 49% These patients fall into a borderline or intermediate group. Their characteristics, treatment patterns, and outcomes appear similar to those of patient with HFpEF. b. HFpEF, Improved >40% It has been recognized that a subset of patients with HFpEF previously had HFrEF. These patients with improvement or recovery in EF may be clinically distinct from those with persistently preserved or reduced EF. Further research is needed to better characterize these patients. II. Heart Failure with Preserved Ejection Fraction (HFpEF) ACCF/AHA 2013 HF Guidelines JAC 2013 5 June (E-Pub online) The number of patients with HF, as well as the cost to treat patients with HF, is expected to increase in the future. All causes of HF must be evaluated, with consideration of multigenerational family histories and genetic testing. Risk factors need to be continually addressed when managing a patient with HF: hypertension, lipid disorders, obesity, diabetes mellitus, tobacco use, and known cardiotoxic agents. There is a clear mortality benefit from using guidelinedirected medical therapy. Important points regarding HF management Anticoagulation should not be used in patients with chronic HFrEF with no risk factors (atrial fibrillation, thromboembolic event, or cardioembolic source). Aim for control of systolic and diastolic blood pressures, as well as volume status, to treat HFpEF. Re-evaluate patients with left ventricular EF ≤35%, New York Heart Association class II-IV, left bundle branch block, and a QRS ≥150 ms for cardiac resynchronization therapy. HF education, dietary restrictions, and exercise training should be provided for all patients to enhance self-care. A HF multidisciplinary team, including a palliative care team, should be involved when treating patients with advanced HF. Important points regarding HF management Classification of Heart Failure A B C ACCF/AHA Stages of HF At high risk for HF but without structural heart disease or symptoms of HF. Structural heart disease but without signs or symptoms of HF. Structural heart disease with prior or current symptoms of HF. NYHA Functional Classification None I I II III IV D Refractory HF requiring specialized interventions. No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF. No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF. Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in symptoms of HF. Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes symptoms of HF. Unable to carry on any physical activity without symptoms of HF, or symptoms of HF at rest. ACCF/AHA 2013 HF Guidelines JAC 2013 5 June (E-Pub online) ACCF/AHA 2013 HF Guidelines JAC 2013 5 June (E-Pub online) At Risk for Heart Failure Heart Failure STAGE A STAGE B STAGE C At high risk for HF but without structural heart disease or symptoms of HF Structural heart disease but without signs or symptoms of HF Structural heart disease with prior or current symptoms of HF e.g., Patients with: · HTN · Atherosclerotic disease · DM · Obesity · Metabolic syndrome or Patients · Using cardiotoxins · With family history of cardiomyopathy Structural heart disease e.g., Patients with: · Previous MI · LV remodeling including LVH and low EF · Asymptomatic valvular disease Development of symptoms of HF e.g., Patients with: · Known structural heart disease and · HF signs and symptoms HFpEF THERAPY Goals · Heart healthy lifestyle · Prevent vascular, coronary disease · Prevent LV structural abnormalities Drugs · ACEI or ARB in appropriate patients for vascular disease or DM · Statins as appropriate THERAPY Goals · Prevent HF symptoms · Prevent further cardiac remodeling Drugs · ACEI or ARB as appropriate · Beta blockers as appropriate In selected patients · ICD · Revascularization or valvular surgery as appropriate STAGE D Refractory HF THERAPY Goals · Control symptoms · Improve HRQOL · Prevent hospitalization · Prevent mortality Strategies · Identification of comorbidities Treatment · Diuresis to relieve symptoms of congestion · Follow guideline driven indications for comorbidities, e.g., HTN, AF, CAD, DM · Revascularization or valvular surgery as appropriate Refractory symptoms of HF at rest, despite GDMT e.g., Patients with: · Marked HF symptoms at rest · Recurrent hospitalizations despite GDMT HFrEF THERAPY Goals · Control symptoms · Patient education · Prevent hospitalization · Prevent mortality Drugs for routine use · Diuretics for fluid retention · ACEI or ARB · Beta blockers · Aldosterone antagonists Drugs for use in selected patients · Hydralazine/isosorbide dinitrate · ACEI and ARB · Digoxin In selected patients · CRT · ICD · Revascularization or valvular surgery as appropriate THERAPY Goals · Control symptoms · Improve HRQOL · Reduce hospital readmissions · Establish patient’s endof-life goals Options · Advanced care measures · Heart transplant · Chronic inotropes · Temporary or permanent MCS · Experimental surgery or drugs · Palliative care and hospice · ICD deactivation Exercise intolerance due to fatigue and dyspnea most prominent Other S & S: ◦ ◦ ◦ ◦ ◦ ◦ Paroxysmal nocturnal dyspnea Orthopnea, Edema Worsening dyspnea with exertion or at rest Tachycardia Change in weight Signs and Symptoms in HF patients Current Guidelines 2013: ◦ Class I Exercise training (or regular physical activity) is recommended as safe and effective for patients with HF who are able to participate to improve functional status (Level of Evidence: A) ◦ Class IIa Cardiac rehabilitation can be useful in clinically stable patients with HF to improve functional capacity, exercise duration, HRQOL, and mortality. (Level of Evidence: B) Role of Exercise Training in HF Improvement in exercise capacity after exercise training due to peripheral adaptations (increased oxygen extraction) Improvement in quality of life Reduced hospitalizations and mortality Improved endothelial function Reduction in catecholamine levels Benefits with exercise and cardiac rehabilitation Three major risk factors: age, presence of heart disease and intensity of exercise ◦ Lowest incidence: walking, cycling and treadmill walking ◦ Least active patients are higher risk ◦ In HF patients, most common events include: post-exercise hypotension, atrial and ventricular arrhythmias and worsening HF symptoms Risks to exercise Weight gain > 3 lb in 1-3 days Drop in systolic BP with exercise (marked/symptomatic) NYHA IV (can exercise selective patients) Complex ventricular arrhythmias Resting heart rate ≥ 100 bpm Pre-existing unstable co-morbidities Relative Contraindications to Exercise in Stable HF Patients Progressive worsening of exercise intolerance (dyspnea at rest) Ischemia is suspected Severe AS or severe regurgitant valvular disease Acute systemic illness New onset afib Acute pericarditis/myocarditis/embolism Absolute Contraindications to Exercise with Stable HF Patients Aerobic activity such as walking or cycling Frequency – 3-5 days a week or most days Intensity – 55-80% heart rate reserve with perceived exertion (1114) Duration of each session – start at 5 minutes if needed and progress to 30-60 minutes Exercise Recommendations Cycling ◦ Allows low level workloads ◦ Easily reproducible ◦ May be safer with orthopedic or balance problems Walking Swimming yoga Interval training Flexibility and resistance training Exercise Recommendations Patient related Social and economic Healthcare team/system Condition and Therapy related Barriers and possible solutions Older age Low level of education Low socio-economic status Minority status Anxiety and depression Logistical problems Lack of motivation, lack of insight into benefits and lack of time Patient related Barriers European Journal of Heart Failure (2012) 14, 451-458 Lack or resources and support Lack of reimbursement Transportation concerns Social and Economic Barriers European Journal of Heart Failure (2012) 14, 451-458 Lack of expertise with heart failure Lack of capacity Lack of referral Lack of education on the importance of exercise Healthcare team/system barriers European Journal of Heart Failure (2012) 14, 451-458 Severity of symptoms Level of disability Rate of disease progression Impact of co-morbidities Condition and Therapy Related Barriers European Journal of Heart Failure (2012) 14, 451-458 Patient related ◦ Optimize heart failure management; manage co-morbid conditions ◦ Discuss activity at each visit to rehab ◦ Assess preferred mode of exercise ◦ Education; engage patient as partner in exercise ◦ Screen for depression Recommendations to overcome barriers System and therapy related ◦ Have referral system in place ◦ Educate providers Recommendations to overcome barriers 74 year-old male with history of coronary artery disease; inferior STEMI 2010 (unsuccessful PCI)complicated with cardiogenic shock and VT; initial EF 25%; received single chamber ICD ◦ ◦ ◦ ◦ ◦ Hypertension Hyperlipidemia Osteoarthritis Ischemic cardiomyopathy insomnia Case study Social History ◦ Never used tobacco products ◦ No alcohol and substance abuse ◦ Retired lawyer Family History ◦ Father died of sudden death – age 60 Surgical History ◦ Cataracts; ICD implant Case Study Medications ◦ Aspirin 81mg daily ◦ Carvedilol 12.5mg twice daily ◦ Lisinopril 20mg daily (now on study drug – NEP inhibitor) ◦ Furosemide 40mg twice daily ◦ Potassium 20mEq daily ◦ Simvastatin 40mg daily ◦ Meloxicam as needed ◦ Trazadone 25mg at bedtime ◦ Nitroglycerine 0.4mg as needed Case study Case Study Exercise history ◦ Swimmer in high school ◦ Lifeguard at the Officers Club Pool in the Army Medical Core ◦ Cardiac rehab after STEMI ◦ Resumed swimming after MI U.S. Master’s Senior Olympics 9 Gold medals in Kansas Senior Meet September ‘13 “My Doctor said if I hadn’t been in such good physical shape from swimming it very likely would have been a fatal heart attack. Swimming or any kind of exercise saves lives”. Find strategies to get patients referred and enrolled in your cardiac rehabilitation program Use this opportunity to give disease specific education to the HF patients Prescribing exercise for HF patients is similar to patients without HF Partner with your providers to help keep these patients out of the hospital with close surveillance of their symptoms. In Summary Thank You! Tamra.Ward@Alegent.org