Assessing Chronic Illness Care in Prison

Assessing Chronic Illness Care in Prison
(ACIC-P): A Tool for Tracking Chronic
Illness Care in Prison
Emily Wang, M.D., MAS
Yale University School of Medicine
Background
• Healthcare is constitutionally guaranteed in
US prison
• 80% of patients have a chronic illness; 40% are diagnosed with chronic illness in prison
• Some prison healthcare systems are embarking on quality improvement programs from chronic illness care
Aim
• To identify a tool to evaluate and direct primary care quality improvement efforts in prison healthcare settings
Assessment of Chronic Illness Care
(ACIC)
• Survey designed to help community primary care organizations assess chronic illness care within the 6 components of the Chronic Care
Model:
– Self-management support
– Linkages to community resources
– Decision support
– Delivery system design
– Clinical information systems
– Organization of the health system
Methods
• Qualitative study using cognitive interviews to better understand the appropriateness of using the ACIC for the prison setting
• Content analysis of interviews were based on the four problem types in cognitive processing
(comprehension, recall, response, and bias)
• Participants included 12 prison health providers and administrators (mean time working 10.25 yrs (0.5-17 yrs))
Study Procedure
Original ACIC Instrument
Reviewed by research team with input from senior leaders of prison systems, and ACIC author
Defined problematic components
Designed Interview probes to assess correctional health providers and administrators interpretation of the ACIC instrument
Training of interviewers and pilot interview Initial modifications to ACIC instrument
ACIC-Prison (ACIC-P)
Cognitive interviews with 12 participants
Iterative process of identifying problematic components at post interview debriefing sessions with modification or inclusion of new verbal probes.
Transcribed interview audio records and performed content analysis, with identification of themes and problematic components
Results: Cognitive Processing
Comprehension e.g. “senior leaders” was interpreted as “... our administrative leadership” and “... my doctor at my medical center”
Response: e.g. “addressing concerns of patients and families.”
Participants indicated they “don’t deal with families”
Results: New Domains for ACIC-P
Role of the Department of Corrections e.g. , “… if you have a guy with chest pain, ..., but you’re also working with the correctional officer to make sure there is security ...”.
Question 1.6. Custody is [intermittently focuses on chronic illness care, has developed a vision for chronic illness care, but no consistent process for getting there, is committed to chronic illness care, and sometimes engage teams in problem solving and implementation, and consistently engages clinical teams improving patient experiences of care and clinical outcomes.]
Results: New Domain for ACIC-P
Discharge planning
“a unique component of chronic illness care in correctional health”
Question 2.4. Linking patients to medical resources after discharge from prison [is not systematically done, is limited to providing a list of resources, is accomplished by a designated person, and is accomplished by coordination between the two healthcare systems.
]
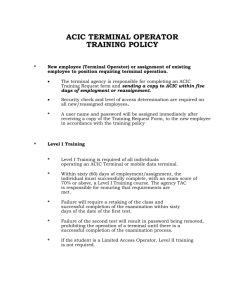
Description
Modifications to ACIC
Number of items Percentage of original ACIC items
Unchanged items from original ACIC
Minor modifications of original ACIC items
Completely changed original ACIC items
New items not in the original ACIC
15
13
6
2
44%
38%
18%
--
Summary
• ACIC is applicable for use in the prison healthcare setting with modifications that reflect the unique nature of practicing primary care in the prison setting
Next Steps
• Administer ACIC-P in two northeastern prison systems to test the psychometric properties of the instrument
*among 55 participants
Acknowledgements
Mentors and Collaborators:
Jenerius Aminawung, MD, MPH
Ed Wagner, MD, MPH
Robert Trestman, PhD, MD
Warren Ferguson, MD
Carol Bova, PhD
Funding:
NHLBI Career Development Award (K23 HL103720)
NIDA R03 (1R03DA031592 )
CMMI (1C1CMS331071-01-00)
Yale Center for Clinical Investigation