Document
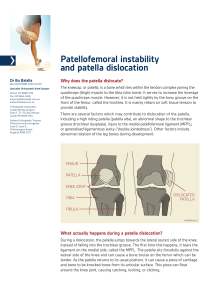
advertisement

Knee Pain What is in common? Observe what? One of the Most Running Injuries Patellofemoral Pain Syndrome ("Runner's Knee") Anatomy Patellofemoral Pain • A common misconception is that the patella only moves in an up-and-down direction. In fact, it also tilts and rotates, so there are various points of contact between the undersurface of the patella and the femur.2,3 • Repetitive contact at any of these areas, sometimes combined with maltracking of the patella that is often not detectable by the naked eye, is the likely mechanism of patellofemoral pain syndrome. • The result is the classic presentation of retropatellar and peripatellar pain. Causes • • • • • • • patellofemoral pain syndrome (PFPS), or simply "runner's knee," is the most common overuse injury among runners. It occurs when a mistracking kneecap (patella) irritates the femoral groove in which it rests on the thighbone. It could be a biomechanical problem—the patella may be larger on the outside than it is on the inside, it may sit too high in the femoral groove, or it may dislocate easily. Also, worn cartilage in the knee joint reduces shock absorption, high-arched feet provide less cushioning, and flat feet or knees that turn in or out excessively can pull the patella sideways. There are also muscular causes. Tight hamstring and calf muscles put pressure on the knee, and weak quadriceps muscles can cause the patella to track out of alignment. Just the repetitive force of a normal running stride alone can be enough to provoke an attack. Causes • Several anatomic and congenital factors may lead to a predisposition towards patellofemoral pain and/or instability. • Tightness of the quadriceps muscles, hamstrings and iliotibial band, and relative weakness of the quadriceps muscle are probably the most common causes. • Other factors that can contribute to this problem include femoral anteversion (excessive rotation of the hips), tibial torsion (excessive rotation of the shin bone), genu valgum (knock knees), genu recurvatum (hyperextended knee) and excessive pronation (flat feet). Etiology • Weakness of the quadriceps • Weakness of the medial quadiceps, specifically VMO dysplasia • Tight iliotibial bands • Tight hamstring muscles • Weakness or tightness of the hip muscles (adductors, abductors, external rotators) • Tight calf muscles scular Etiologies of Patellofemoral Pain Syndrome and Their Pathophysiology Etiology Pathophysiology Weakness of the quadriceps The "quads" include the vastus medialis, vastus medialis obliquus (VMO), vastus intermedius, vastus lateralis and rectus femoris. Weakness may adversely affect the patellofemoral mechanism. Quad-muscle strengthening is often recommended.3,4,7,9,10,14-17 Weakness of the medial quadiceps, specifically VMO dysplasia Weakness of the VMO allows the patella to track too far laterally. Although the role of the VMO is controversial,18-20 VMO strengthening is often recommended.6,7,11,15,16 However, the VMO is a difficult muscle to isolate,21 and most patients find general quadriceps strengthening easier to accomplish. Tight iliotibial bands A tight iliotibial band places excessive lateral force on the patella and can also externally rotate the tibia, upsetting the balance of the patellofemoral mechanism. 22,23 This problem can lead to excessive lateral tracking of the patella. Tight hamstring muscles The hamstring muscles flex the knee. Tight hamstrings place more posterior force on the knee, causing pressure between the patella and femur to increase.7,15,16 Weakness or tightness of the hip muscles (adductors, abductors, external rotators) The VMO originates on the adductor magnus tendon. This is the anatomic basis for recommending adductor strengthening.11,14,16Abductor (gluteus medius) strengthening helps to stabilize the pelvis. Dysfunction of the hip external rotators results in compensatory foot pronation; a simple stretch can improve muscular efficiency. 4 Tight calf muscles Tight calves can lead to compensatory foot pronation and, like tight hamstrings, can increase the posterior force on the knee.11,15,16 NOTE: Exercises to treat the various muscular causes are illustrated in thepatient information handout that follows this article. Information from references 3, 4, 6, 7, 9 through 11, and 14 through 23. Malalignment Q angle • Angle. Although some investigators believe that a "large" Q angle (Figure 3) is a predisposing factor for patellofemoral pain, others question this claim. • One study12 found similar Q angles in symptomatic and nonsymptomatic patients. • • Another study6 compared the symptomatic and asymptomatic legs in 40 patients with unilateral symptoms and found similar Q angles in each leg. • Furthermore, "normal" Q angles vary from 10 to 22 degrees,3depending on the study, and measurements of the Q angle in the same patient vary from physician to physician.13 Foot Overpronation chondromalacia patella Normally, the hyaline cartilage on the back surface of the patella is thicker than anywhere else in the body. Problems with the cartilage on the back of the patella include softening, blistering, fissuring, erosion, and thinning. These problems are collectively called chondromalacia patella. • The top view is called a "Merchant's view" and is obtained with the knee bent 45-degrees, with the beam of the X-ray photograph directed through the knee from head to toe. It shows how well the patella is aligned within the groove on the femur, called the trochlear groove • A high-riding patella is called patella alta, and can be associated with instability of the patella, as it is not well-engaged in the trochlear sulcus with the knee near full extension (straight). A • low-riding patella is called patella baja. Treatment • Many cases of mild to moderate chondromalacia patella can be treated with just oral anti-inflammatory medication, weight loss and the proper type of therapeutic exercise. • While nutritional supplements such as glucosamine and chondroitin have been shown to ease arthritic joint discomfort and slow down articular cartilage breakdown in some patients, there is no convincing proof yet that they totally halt or reverse chondromalacia. • Viscosupplementation(Synvisc, Hyalgan, etc.) injection treatment does not seem to work as well on patellar arthritis pain as it does on symptoms caused by arthritic joint surfaces elsewhere in the knee. Core Strengthening • An 8-week rehabilitation program focusing on strengthening and improving neuromuscular control of the hip and core musculature produces positive patient outcomes, improves hip and core muscle strength, and reduces the knee abduction moment, which is associated with developing PFPS. Knee Flexion • Previous research has been done to indicate that in a closed chain setting, knee flexion beyond 60 degrees leads to increased patellofemoral joint compression and this may be contraindicated for those with PFJ pain or chondromalacia. • Also keep in mind that most people with PFJ complain of more pain descending stairs than ascending stairs. Knee Flexion VMO • The VM has an important role as a medial stabilizer of the patella and aids in the normal functioning of the PFJ. • The VM is phylogenetically the weakest of the quadriceps group and appears to be the first muscle to atrophy and the last to rehabilitate • Quadriceps strengthening exercises, emphasizing the VM, have been suggested as the primary initial management of patellofemoral disorders VMO Exercises Rehabilitation • Rest • Ice • Stretching (quads, hamstrings, IT band and hip musculature) • Straight leg raises • Short arc quads (mini-knee extensions from 30-0 degrees if you will on a bolster) although I am not a huge fan of these • Mini-squats • Calf raises Surgery