The Knee - WordPress.com
advertisement

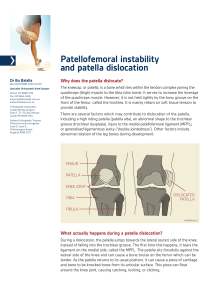
The Knee MSC MANUAL THERAPY SEPT 2011 JANE ASHBROOK Msc Manual Therapy The Knee FUNCTIONAL ANATOMY AND CLINICAL PRESENTATIONS Anterior Cruiate Ligament ACL Normal Partial tear Treatment Conservative Management ACL Reconstruction Indications for ACL reconstruction Professional athletes must have surgery. Prevents meniscal tears and OA. Recreational athletes will benefit, especially activities involving twisting and turning eg. Skiing, tennis, squash. 90% of patients achieved normal or nearly normal function following ACLR (Ardern et al, 2011). Medial Collateral Ligament MCL •Indications Valgus stress test less give in ext suggests ACL/PCL/POL/PMC intact. DMCL tighten with ER. SMCL primary valgus restraint throughout flex. PMC/POL controls valgus, IR and post drawer in ext. (Coen et al, 2010) Total ruptures usually occur with associated injury, including ACL, med or lat meniscus (Nakamyra et al, 2003). Management Conservative: Grade 1,2 and acute 3. Protected weight bearing Early active movement Hinge brace (gr 3) Progressive strength Functional rehab Good outcomes (Cohen et al, 2010) Surgical: Combined SMCL +/- DMCL and POL injuries causing severe instability. Anatomic recontruction of SMCL and POL. Concurrently with coexisting ACLR. May require arthroscopy before or after if chondral defect or meniscal tear present. Posterior Cruciate Ligament PCL Indications Accounts for only 0.65% of all knee injuries (Majewski et al, 2006) 50% MVA (Dandy and Pusey, 1982). Rupture well tolerated ?meniscofemoral ligaments resist post drawer up to 40% (Malone et al, 2006). Management Conservative: ?Immobilised in ext brace 6 weeks. Functional rehab. V little evidence. Surgical: Avulsion # can be repaired. Little evidence for PCLR. No evidence regarding long term OA. If instability present then likely to be other ligaments involved and multiple repair required. Lateral Collateral Ligament LCL 1.1 % of athletic knee injuries (Majewski et al, 2006) Common peroneal nerve injured in conjunction in 15% of cases- meta analysis of 139 patients (Malone et al,2006) If LCL sectioned then small increase in varus is seen on testing. If large movement detected on varus testing then multiple ligament injury should be suspected. Postero-Lateral Corner PLC Indications Rarely injured in isolation (Malone et al, 2006). May present with +ve Dial, +ve postlat drawer and varus opening at 0-30˚ flex. Unstable knee, ?failed ACLR. Post and lat thrust on stance phase of gait. Management Conservative: Knee very unstable. Chronic instability or failed ACL reconstruction. Surgical: Early repair best: 48hrs7 days (La Prade et al, 1997). Larson (sling ITB) or LaPrade (TA allograft) technique. Correction of lat thrust. Can’t replace normal PLC function. Meniscal Injuries Meniscal tears Tear posterior horn medial meniscus with meniscal cyst Radial tear lat meniscus Indications Twisting, change of direction on loaded knee. Acceleration/deceleration. Degen tears spontaneous/minor incident. Composite testing most effective. Accuracy difficult in degen tears and associated lig injuries. Torn discoid lat meniscus: children. Post horn lat meniscus: instability and detachment, PLC. (McDermott, 2011.) Tears Management Conservative: Can be asymptomatic. Less mechanical symptoms in degen tears. Rehab AROM and functional strength. (McDermott, 2011) Surgical: Arthoscopy. Repair: vertical, some horiz, 25% under 40. Sutures. Rehab: PWB, 90* brace 6 weeks. Start impact 3 months. Resect: flap, ragged, complex. Rehab: very quick. New tech: replacement. Chondral Surface Injury Indications Rotational forces cause stress fracture in subchondral bone, fails to heal, necrosis. Common in adolescents, usually stable. Unstable in adults, can cause loose body. Classified dependent on extent and depth. Need WB x-ray and MRI. (Cole and Cohen, 2011) Management Conservative: NSAIDs Corticosteroids Chondroprotective agents. Activity modification/avoidance. Brace. Strength and flexibility. Ineffective. Surgical: Palliative: debridement and lavage. Reparative: marrow stimulating technique. Restorative: ACI, osteochondral grafting. Patello femoral Pain Syndrome Forces Patellofemoral Joint Reaction Force Patellofemoral Joint Stress= PJRF ÷ PF contact area. Unreliable clinical measurement. Increase in angle will increase Lateral patella displacement. Biomechanics Angle of knee flexion Event 0-10* No patella contact with femur 10-30* Patella aligns and enters intercondylar notch 0-50* Tension in patella tendon greater than tension in quads 0-90* Contact zone moves proximally >50* Tension in patella tendon lower than tension in quads 0-60* PJRF and PJS increase 60 ±5* Peak PJS, quads neutral, critical angle 85-90* Quads wrap (Selfe, 2004) Indications Controversy in literature: overloaded with theories. Subchondral bone deformation(Goodfellow et al, 1998, Naslund et al, 2005) Intermedullary pressure changes (Arnoldi, 1991) Lateral retinacular neuroma formation (Sanchis-Alfonso et al, 1998) Vascular dysfunction (Sanchis-Alfonso et al, 2007, Selfe – work ongoing) The tissue homeostasis theory/the biological inflammatory cascade (Dye et al, 1999 Risk Factors Lower limb malalignment (Shelton, 1991). VMO:VL muscle imbalance (McConnel, 1986). VM considered single anatomical unit (Hubbard, 1998). Conflicting evidence of delayed onset VMO (Selfe, 2004). VMO onset delay in runners with PFPS (Ng et al, 2011). VMO-VL timing rations vary between healthy subjects and patients (Selfe, 2004). Effusion inhibits quads: VM (Torry, 2000). Risk Factors Reduced quads flexibility, VM reflex response time, explosive strength and vertical jump ability (Witrouw, 2000). Weakness of hip lateral rotators and abductors (Robinson, 2007 and Ireland, 2003). PFPS subjects sig difference in ITB length in symptomatic and asymptomatic sides(Hudson and Darthuy, In Press) ITB tightness increases pressure on lateral patella facet (Merican et al, 2009) PFPS subjects had significantly shorter hamstrings than asymptomatic controls (White et al, In Press) Treatment Poor prediction of recovery if pain persists for 2 years (Price, 2000). Combination of CKC and OKC exercises required. OKC avoided in 1st 30* flex (Doucette, 1996). Exercises can be performed in controlled pain. Proprioception (Callaghan, 2008, 2010, 2011). Mobilisation and manipulation. Acupuncture. Taping/bracing . Combined (Mason, 2010). Orthotics (Vincenzino, 2010 and Barton, 2009). Patella Instability Indications Functional valgus: if lat force of eccentric quads overcomes VMO and MPFL, patella can dislocate (Greiwe, 2009). Articular geometry: patella alta-increased translation prior to trochlear engagement (Greiwe, 2009). Dynamic limb alignment: femoral anteversion, decreased hip abd and IR strength (Ireland, 2003). Dynamic stability: VMO injury in acute dislocation. Static stability: MPFL fails at low load, 50% increase lat displacement patella (Greiwe, 2009). Management Conservative: Dynamic neuromuscular control: hip, knee, core. Proprioception. Orhtotics. Rehab remains reduced in a proportion of patients (Smith, 2010). VMO activity and onset timing uncertain (Smith, 2010). Surgical: Tibial tubercle osteotomy: alter Q-angle. Distal tubercle osteotomy: decrease patella alta. Trochleoplasty: Increase trochlear groove. Quadsplasty: suture VMO to add magnus. MPFL recon: gracilis aotgraft. Osteoarthritis Risk factors Post menisectomy: Younger patients. Decrease contact surface area 75% and increase contact pressures 235% (McDermott, 2010) 1400% increased prevalence 21 years after menisectomy (Roos, 1998). Degenerative: Older patients. Obesity. Repetitive strain, wear and tear. Genetic predisposition. Management Conservative: Decrease effusion. Increase AROM and flerxibility. Increase muscle strength and propriocetion. Activity modification. NSAIDs. Surgical: Corticosteroid injections. Hyaluronic acid injections. Wash out and debridement. TKR.