joint commission int.presentation
advertisement

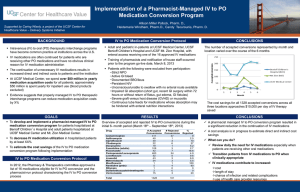
Dr.Ihab Nada,M.D Director of education MSKMC MISSION The mission of Joint Commission International (JCI) is to improve the safety and quality of care in the international community JCI was created in 1998 as the international arm of The Joint Commission (United States) The process of developing standards is , actively overseen by an expert international task force, whose members are drawn from each of the world’s populated continents .JCI standards are the basis for accreditation and certification of individual health care facilities and programs around the world. What is accreditation? Accreditation is a process in which an entity, usually nongovernmental, assesses the health care organization to determine if it meets a set of requirements (standards) designed to improve the safety and quality of care. What are the benefits of accreditation? Accreditation has gained worldwide attention as an effective quality evaluation and management tool. improve public trust that the organization is concerned for patient safety and the quality of care; provide a safe and efficient work environment that contributes to worker satisfaction; negotiate with sources of payment for care with data on the quality of care; How frequently will the standards be updated? the standards will be revised and published at least every three years. Accreditation Surveys • interview with staff and patients and other verbal information; • on-site observations of patient care processes by surveyors; • policies, procedures, clinical practice guidelines, and other documents provided by the organization Section I : International Patient Safety Goals (IPSG) Goal 1: Identify Patients Correctly using two patient identifiers, before administering medications, blood, before taking blood and other specimens or providing treatments Goal 2: Improve Effective Communication The complete verbal and telephone order or test result is written down , and is read back by the receiver of the order then it is confirmed by the individual who gave the order or test result. Goal 3: Improve the Safety of High-Alert Medications High-alert medications are those medications involved in a high percentage of errors medications that carry a higher risk for adverse outcomes, look-alike/sound-alike medications example, concentrated electrolytes as potassium chloride 2 mEq/ml concentrated How to improve safety removing the concentrated electrolytes from the patient care unit to the pharmacy. clearly labeled and stored in a manner that restricts access. Goal 4: Ensure Correct-Site, Correct-Procedure, Correct-Patient Surgery mark for surgical-site identification and involves the patient in the marking process The organization uses a checklist to verify preoperatively the correct site, correct procedure, and correct patient and that all documents and equipment needed are on hand, correct, and functional. The full surgical team conducts and documents a time-out procedure just before starting a surgical procedure. Goal 5: Reduce the Risk of Health Care–Associated Infections include catheter-associated urinary tract infections, blood stream infections, and pneumonia(often associated with mechanical ventilation). Via effective hand-hygiene program. Goal 6: Reduce the Risk of Patient Harm Resulting from Falls initial assessment of patients for fall risk Measures are implemented to reduce fall risk for those assessed to be at risk. Access to Care and Continuity of Care (ACC) 1-Admission to the Organization To have a process for admitting inpatients and for registering outpatients. Patients with emergent, urgent, or immediate needs are given priority The organization considers the clinical needs of patients when there are waiting periods or delays for diagnostic and/or treatment services. At admission as an inpatient, patients and families receive information on the proposed care, the expected outcomes of that care, and any expected cost to the patient for the care. Admission or transfer to or from units providing intensive or specialized services is determined by established criteria. 2-Continuity of Care During all phases of inpatient care, there is a qualified individual identified as responsible for the patient’s care. 3- Discharge, Referral, and Follow-Up The organization cooperates with health care practitioners and outside agencies to ensure timely and appropriate referrals. The clinical records of inpatients contain a copy of the discharge summary. The clinical records of outpatients receiving continuing care contain a summary of all known diagnoses, drug allergies, current medications, and any past surgical procedures and hospitalizations. Patients and, their families are given understandable follow-up instructions. The organization has a process for the management and follow-up of patients who leave against medical advice. 4-Transfer of Patients The transfer process addresses who is responsible during transfer and what supplies and equipment are required during transport. The referring organization determines that the receiving organization can meet the needs of the patient to be transferred. Patient clinical information or a clinical summary is transferred with the patient. During direct transfer, a qualified staff member monitors the patient’s condition. The transfer process is documented in the patient’s record. 5-Transportation The transportation provided or arranged is appropriate to the needs and condition of the patient. There is a process in place to monitor the quality and safety of transportation provided or arranged by the hospital, including a complaint process. Patient and Family Rights Respond to the patient’s requests related to religious beliefs Care is respectful of the patient’s need for privacy. Patients are protected from physical assault. Patient information is confidential. MSKMC will inform pts & family with diagnosis ,ttt plan , complications and consequences of refusing or discontinuing ttt The organization supports the patient’s right to respectful and compassionate care at the end of life. Patient informed consent is obtained The organization informs patients and families about how to gain access to clinical research, clinical investigation, or clinical trials involving human subjects. Informed consent is obtained before a patient participates in clinical research, clinical investigation, and clinical trials. Assessment of Patients (AOP) Each patient’s initial assessment(s) includes an evaluation of physical, psychological, social, and economic factors, including a physical examination and health history. Assessment findings are documented in the patient’s record and readily available to those responsible for the patient’s care. All patients are reassessed at intervals based on their condition and treatment to determine their response to treatment and to plan for continued treatment or discharge. Qualified individuals conduct the assessments and reassessments. Laboratory Services All equipment used for laboratory testing is regularly inspected, maintained, and calibrated, and appropriate records are maintained for these activities. Procedures for collecting, identifying, handling, safely transporting, and disposing of specimens are followed. A laboratory safety program is in place, followed, and documented. Radiology and Diagnostic Imaging Services Radiology and diagnostic imaging services are provided by the organization or are readily available through arrangements with outside sources. Individuals with proper qualifications and experience perform diagnostic imaging studies, interpret the results, and report the results. Care of Patients (COP) Food and Nutrition Therapy A variety of food choices, appropriate for the patient’s nutritional status and consistent with his or her clinical care, is regularly available. Pain Management Patients are supported in managing pain effectively. End-of-Life Care Care of the dying patient optimizes his or her comfort and dignity. Care Delivery for All Patients Patients with the same health problems and care needs have a right to receive the same quality of care throughout the organization. Anesthesia and Surgical Care Anesthesia services (including moderate and deep sedation) are available to meet patient needs, A qualified individual(s) is responsible for managing the anesthesia services Each patient’s surgical care is planned and documented based on the results of the assessment. Anesthesia & surgical care are documented in pts records Medication Management and Use An appropriately licensed pharmacist, technician, or other trained professional supervises the pharmacy or pharmaceutical service. An appropriate selection of medications for prescribing or ordering is stocked or readily available. Medications are properly and safely stored. Prescribing, ordering, and transcribing are guided by policies and procedures. The organization identifies those qualified individuals permitted to prescribe or to order medications. A system is used to dispense medications in the right dose to the right patient at the right time. The organization identifies those qualified individuals permitted to administer medications. Medication effects on patients are monitored. Patient and Family Education (PFE) The organization provides education that supports patient and family participation in care decisions and care processes. Education and training help meet patients’ ongoing health needs. Health professionals caring for the patient collaborate to provide education. Section II: Health Care Organization Management Standards Quality Improvement and Patient Safety Those responsible for governing and managing the organization participate in planning and measuring a quality improvement and patient safety program. Design of Clinical and Managerial Processes Data Collection for Quality Measurement Analysis of Measurement Data Improvement Prevention and Control of Infections One or more individuals oversee all infection prevention and control activities. This individual(s) is qualified in infection prevention and control practices through education, training, experience, or certification. The organization designs and implements a comprehensive program to reduce the risks of health care–associated infections in patients and health care workers. The organization provides barrier precautions and isolation procedures that protect patients, visitors, and staff from communicable diseases and protects immunosuppressed patients from acquiring infections to which they are uniquely prone. Gloves, masks, eye protection, other protective equipment, soap, and disinfectants are available and used correctly when required. The organization provides education on infection prevention and control practices to staff, physicians, patients, families, and other caregivers when indicated by their involvement in care. Governance, Leadership, and Direction Governance responsibilities and accountabilities are described in bylaws, policies and procedures, or similar documents that guide how they are to be carried out. A senior manager or director is responsible for operating the organization One or more qualified individuals provide direction for each department or service in the organization. Facility Management and Safety The organization complies with relevant laws, regulations, and facility inspection requirements. The organization plans and implements a program to provide a safe and secure physical environment. The organization has a plan for the inventory, handling, storage, and use of hazardous materials and the control and disposal of hazardous materials and waste. The organization develops and maintains an emergency management plan and program to respond to likely community emergencies, epidemics, and natural or other disasters. The organization plans and implements a program to ensure that all occupants are safe from fire, smoke, or other emergencies in the facility. The organization plans and implements a program for inspecting, testing, and maintaining medical equipment and documenting the results. Potable water and electrical power are available 24 hours a day, seven days a week, The organization educates and trains all staff members about their roles in providing a safe and effective patient care facility. Staff Qualifications and Education Organization leaders define the desired education, skills, knowledge, and other requirements of all staff members. Organization leaders develop and implement processes for recruiting, evaluating, and appointing staff as well as other related procedures identified by the organization. The organization uses a defined process to ensure that nonclinical staff knowledge and skills are consistent with organization needs and the requirements of the position. All clinical and nonclinical staff members are oriented to the organization, the department, or unit to which they are assigned and to their specific job responsibilities at appointment to the staff. The organization uses an ongoing standardized process to evaluate the quality and safety of the patient services provided by each medical staff member. The organization has an effective process to gather, to verify, and to evaluate the nursing staff ’s credentials (license, education, training, and experience). The organization has a standardized procedure to gather, to verify, and to evaluate other health professional staff members’ credentials (license, education, training, and experience). Management of Communication and Information Communication with the Community Communication with Patients and Families Communication Between Practitioners Within and Outside of the Organization Patient Clinical Record The organization initiates and maintains a clinical record for every patient assessed or treated. Thank you ………………..