Diseases of the Esophagus
advertisement

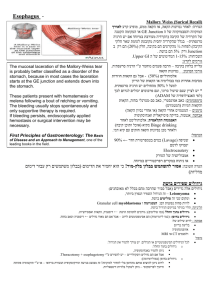
כירורגית חזה מ.ר קפלן צינור שרירי באורך 25ס"מ מחולק ל :3-צוארי ,חזי ,בטני בתמט במנוחה נמתח עד 2-3ס"מ בבליעה שטוח ב 2/3-העליונים ומעוגל ב 1/3-התחתון מתחיל מגובה C6ועד כ- 3ס"מ מתחת לסרעפת – T11 האיבר הצר ביותר במערכת העיכול למעט התוספתן 1/3עליון הוא שריר מפוספס 1/3תחתון הוא שריר חלק 1/3אמצעי הוא שילוב של השניים מכיל שני ספינקטרים מכוסה באפיתל קשקשי שכבות4 לושט Mucosa Submucosa Muscularis propria Adventitia אין- בניגוד לשאר מע' העיכול סרוזה אזורים פונקציונליים ולא אנטומיים ניתן לזהות ע"י מדידות לחץ :UES אזור לחץ גבוה באורך 2-3ממ בין הפארינקס לושט סמוך לcricopharyngeal muscle - :LES אזור לחץ גבוה באזור ה- GEJ בד"כ כ 3-ס"מ מתחת להיאטוס השכבות השריריות אחראיות לפריסטלטיקה של הושט שתי שכבות – פנימית צירקולרית וחיצונית אורכית מע' אנסטומוזות נרחבת מע' ניקוז תת רירית הכרחי להתפשטות מהירה של גידולים שליחת גרורות לפני חסימה של החלל שיעור הישנות גבוה 1. Hiatal Hernia 2. Reflux esophagitis 3. Esophageal motility disorders 4. Cancer Sliding hiatal hernias are more common – 95% The lower esophageal sphincter mechanism becomes incompetent Reflux of acid gastric juice produces a chemical burn Degree of mucosal injury is a function of the duration of acid contact Continued inflammation of the distal esophagus may lead to mucosal erosion Ulceration eventually scarring and stricture Intestinal metaplasia (Barrett`s esophagus) Hiatal hernia with reflux is frequently found in patients who are overweight. Many patients with hiatal hernia have no symptoms. A burning epigastric or substernal pain or tightness Usually the pain does not radiate May be described as a tightness in the chest and can be confused with the pain of myocardial ischemia Aggravate Allevaite supine or leaning over, alcohol, aspirin, tobacco, and caffeine Antacid therapy Late symptoms of dysphagia and vomiting usually suggest stricture formation Anamnesis Weight loss is a feature due to distal esophageal stricture Manometry - loss of the lower esophageal highpressure area 24-h pH-monitoring – gold standard for GERD Upper-GI series Esophagogastric endoscopy - Bx Medical Therapy Avoidance of gastric stimulants (coffee, tobacco, and alcohol) Weight loss Avoid eating several hour before bedtime PPI Failure of PPI treatment Correct the anatomic defect Prevent the reflux of gastric Complications post surgery 3-10% inability to belch or vomit- the "gas-bloat" syndrome Vagal injury The wrap itself Dysphagia Disruption of the repair with recurrent symptoms – 5% esophageal perforation Splenic injury Penumothorax Failure of the high-pressure zone sphincter to relax Not due to spasm Painless dysphagia Progressive dilation of the proximal esophagus Dysphagia Regurgitation of undigested food Weight loss Pain is uncommon Aspiration pneumonia is common Complain of spitting up foul-smelling secretions when simply leaning forward Generally first confirmed by contrast studies of the esophagus Dilation of the proximal esophagus is classic Esophageal diverticula may be present at any level Esophageal manometry – gold standard Medical treatment has generally not been helpful Invasive endoscopic procedure forceful dilation – effective - 60%. 4% perforations Botoxtm – 50% recurrence within 6 months Surgical Transaction of muscle - Heller myotomy Esophagectomy – sigmoid esophagus, failure of more than one myotomy, or an undilatable stricture The second most common manifestation of esophageal motility disorders Pulsion or Traction, depending on the mechanism that leads to their development Upper third cervical esophageal diverticula usually pulsion Cervical diverticula, or Zenker's pulsion related to dysfunction of the cricopharyngeal muscle complain of regurgitation of recently swallowed food putrid breath odor Treat the underlying condition! • Excision of the diverticula • Myotomy of the cricopharyngeal muscle Middle-third esophageal diverticula Traction Not related to esophageal dysmotility Result of mediastinal inflammation Usually asymptomatic and do not warrant treatment. Diverticula of the distal third of the esophagus Dysfunction of the esophagogastric junction Stricture antireflux surgical procedures Achalasia Excision of the diverticula Always - correction of the underlying pathologic process Exceedingly rare – in middle and distal 1/3 Leiomyomas are the most common intramural tumors 1) potential for malignant degeneration appears to be quite low 2) indent the lumen of the esophagus on contrast radiography 3) tend to grow progressively and cause dysphagia 3) Excised for possible dysphagia and malignancy GERD - Chronic acid reflux Columnar intestinal metaplasia 40 times risk for AdenoCA May progress to Low grade dysplasia High grade dysplasia (stage 0 carcinoma) Invasive AdenoCA 30% are squamous cell carcinomas 70% are Adenocarcinomas < 1% are malignant melanoma Adenoid cystic tumors Sarcomas Origin SCC – squamous epithelium AdenoCA – Barrett`s esophagus Commonly occurs in association with alcohol and/or tobacco abuse Etiology has been related to diet, vitamin deficiency, poor oral hygiene, surgical procedures, and a number of premalignant conditions, (caustic burns, Barrett's esophagus, radiation, esophageal diverticula). Vague symptoms at early stages Weight loss and pain may be present Dysphagia – obstruction of >30% Odynophagia Iron deficiency anemia Endoscopy and biopsy of the lesion Endoscopic US – T & N staging Chest & Abdominal CT – M staging PET CT T1 lamina propria or submucosa T1a muscularis mucosae T1b submucosa T2 - muscularis propria T3 - adventitia T4 - adjacent structures • N0 - No regional lymph node metastasis • N1 - 1 to 2 regional lymph nodes • N2 - 3 to 6 • N3 - >6 Early disease – stage I,(IIa ?) Surgery Locally advanced disease – stage IIb, III Neoadjuvant therapy Surgery Surgical techniques Transhiatal esophagectomy Transthoracic esophagectomy En-block esophagectomy טיפול כירורגי למטרת ריפוי טיפול כירורגי כפליאציה? כירורגיהGold standard - three field esophagectomy - ושט צווארי jejunal flap/ stomach ) כירורגיה+ חזה+ג.א.) א three field esophagectomy - ושט חזי Ivor Lewis/ lt thoracotomy Trans Hiatal אוIvor Lewis - ושט תחתון lt thoracotomy אוIvor Lewis - " "צומת ושט קיבה במשלב עם כריתת קיבה טכניקה כירורגית כניסה? כמה ושט לכרות? כמה בלוטות להסיר? "תחליף ושט"? טכניקת השקה? מאפייני מטופל מיקום השאת? מאפייני מטופל? ניסיון כירורגי? גישה נפוצה 2חתכים OPEN/ LAP יתרונות השקה בצוואר תחלואה חסרונות אונקולוגיה יתרונות אונקולוגיה תחליף ושט חסרונות תחלואה ,תמותה. Rt Thoracotomy Laparotomy Cervical Esophagectomy Combined thoracoscopic / laparotomy Combined thoracoscopic / laparoscopic Laparoscopic transhiatal קיבה מעי גס מעי דק Major complications Perioperative Mortality – 4-7% Anastomotic leak – 5-15% Vocal cord paralysis Chylothorax Empyema Long term Stricture