Awake Craniotomy: Role in
Neurosurgical Management
Christine Stewart
University of Minnesota, MS4
Outline
• Case R.P.
• Classic indications and exclusion criteria
• Factors to consider when defining eloquent
areas
• Recommendations
R.P.
• 42 RHM w/ long history of seizures recently changed in character,
worsening H/A over past several months. Wife notes increasing apathy,
slow processing
• Difficulty with word-finding, long-term memory, mood-swings
• Other PMHx:
– Cyclist v. car 1983: LOC 1-2 minutes, right frontal frx w/ CSF leak meningitis
– 1st seizure 1985 GTC w/ auras
– Another episode of meningitis 1985 intracranial abscess R. frontal lobe
R. frontal craniotomy
– Imaging from 2002-2008 show a hypodensity in the left frontal lobe which was
interpreted as encephalomalcia given hx
– Hypothyroidism
• Medications:
– Lamictal 400 mg
– Vimpat 200 mg BID
– Levothyroxine
Imaging
Classic Indications for Awake
Craniotomy1
• Surgery in ‘eloquent’ brain
– Near motor strip
– Speech/language centers
– Thalamus
• Removal of brainstem tumors
• Search for a focus of seizure activity
Exclusion Criteria2,3, 4
• Inability to cooperate: dysphasia, language
barrier, emotional labiality, cognitive
impairment
• Low occipital tumors
• Tumors with significant dural attachment
• Patients < 11 years old5
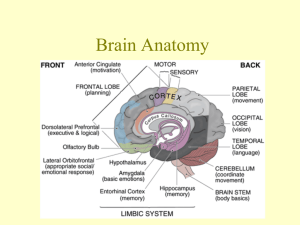
Eloquent areas and factors to consider:
Anatomical variability6
– ICBM 452 atlas
• “Average” brain
– Factors: sex, age,
handedness,
neurological and
psychiatric disease
Eloquent areas and factors to consider:
Functional variability6,7,8
– Even areas with the same anatomical landmarks
may not harbor the same underlying function
• Motor cortex variability:
– “Hand knob” of pre-central gyrus can represent primary
motor cortex or premotor cortex
– Stimulation in pre-central cortex can result in sensory and
motor responses or motor responses in > 1 motor group
– Primary motor area may extend > 20 mm anterior to the
central sulcus
Eloquent areas and factors to consider:
Functional variability
• Variability in language cortices6
– > 4cm of variability in intraoperative speech arrest
J Neurosurg 71:316–326, 1989.
Eloquent areas and factors to consider:
Effect of space-occupying lesions
– Unusual functional acquisition: congenital lesions
(AVMs) higher incidence right v. left sided
language6
– Reorganization: LGG (low grade gliomas)/other
adult neurological injury reorganization of
speech center s.t more frontal speech centers in
pt vs. controls10
– Extent likely depends on time-course of injury9
– Illustratively, these patients rarely present with
neurodeficits9
Variability in Mapping Functional
Localization2,6
• Either measuring electrophysiological signals or
perfusion
• Electrocortical stimulation mapping (ESM)
identifies essential and involved areas
– Other methods seem to be more sensitive to map all
involved areas, but do not identify which are essential
• If essential area is identified:
– Appropriate resection margins have not been
recommended
Effects of Mapping4
% of all patients
% w/ post-op
neurodeficits
% w/ deficits who
were previously
intact
+ Mapping
22.5%
20.9%
4.4%
- Mapping
77.5%
13.5%
1.8%
When considering awake craniotomy:
• Outcomes
– No prospective randomized control trial has been done directly comparing
awake v. GA3
• Patient experience
– Awake procedures are well-tolerated11
• Overall satisfaction rated: 71-93%
• Significant pain identified: 8-29%
• All of this literature asks post-op and relies on recall
– Non-language deficits are noted after surgeries done under GA2
• Visual, spatial perceptions, cognitive and behavioral disorders noted as more individuals
do neuropsychological testing.
• Cost4
– Reduces operating time
• Dependent on experience level
– Reduces post-op ICU stay
– Reduces total hospital stay
• Median LOS: 1 day
Recommendations
• No ‘gold standards’ for pre-operative mapping
b/c no outcomes-correlated evidence
– fMRI at minimum
– DTI may help define white matter tracts in and
around the lesion
– Others: MEG, PET
• Intra-operative monitoring should be
mandatory
– only technique with validated outcomes measures
References
1 Greenberg, M. Handbook of Neurosurgery. 7th edition.
2 Duffau, H. Awake surgery for non-language mapping. Neurosurgery. 66:523-529, 2010.
3 Kirsch, B. and Bernstein, M. Ethical challenges with awake craniotomy for tumor. Can. J. Neurol Sci 39:
78-82, 2012.
4 Serletis, D. and Bernstein, M. Prospective study of awake craniotomy used routinely and nonselectively for supratentorial tumors. J Neurosurgery. 107:1-6, 2007.
5 Berger, MS. The impact of technical adjuncts in surgical management of cerebral low grade gliomas of
childhood. J. of neuro-oncology. 1996; 28:129-155.
6 Pourtrain, N. and Bookheimer, S. Reliability of anatomy as a predictor of eloquence: a review.
Neurosurg Focus 28:E3, 2010.
7 Shinoura N, Suzuki Y, Yamada R, Tabei Y, Saito K, Yagi K:Precentral knob corresponds to the primary
motor and premotor area. Can J Neurol Sci 36:227–233, 2009
8 Uematsu S, Lesser R, Fisher RS, et al: Motor and sensory cortex in humans: topography studied with
chronic subdural stimulation. Neurosurgery 31:59–72, 1992
9 Desmurget M, Bonnetblanc F, Duffau H: Contrasting acute and slow-growing lesions: a new door to
brain plasticity. Brain 130:898–914, 2007
10 Lucas TH II, Drane DL, Dodrill CB, Ojemann GA: Language reorganization in aphasics: an electrical
stimulation mapping investigation. Neurosurgery 63:487–497, 2008
11 Manchella, S. et al. The experience of patients undergoing awake craniotomy for excision of
intracranial masses: expectations, recall, satisfaction and functional outcome. British Journal of
Neurosurgery. June 2011. 25(3): 391-400.