13. Community Pain Clinic
advertisement

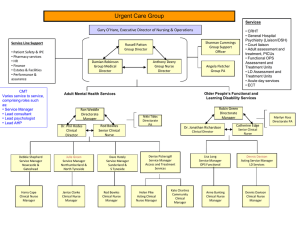
September 5th – 8th 2013 Nottingham Conference Centre, United Kingdom www.nspine.co.uk NWH Community Pain Clinic How can we support people with spinal pain? Mags Wigram, ESP, Pain Management 6th September 2013, N Spine, Nottingham The Clinical Team Pain Consultant Dr Greg Hobbs Advanced Physiotherapy Practitioner Mags Wigram Nursing Team: Advanced Nurse Practitioner Paula Banbury Advanced Nurse Practitioner and Cognitive Behavioural Psychotherapist Kate Feenan Clinical Nurse Specialist Julie Conners The Admin Team Heidi Lewis NWH Primary Care Patient Services Co-ordinator Jo Faulkner and Alicia Shaw NWH Administrators David Hale NWH Information and Governance Co-ordinator Face to face triage • Pain Consultant or Advanced Physiotherapist Practitioner, • 30 or 40 minute assessments, • History taking and physical examination, • Triage decision in agreement with patient. Face to face triage options • Urgent imaging or urgent referral direct to appropriate specialist, • Routine imaging (MRI, nerve conduction studies, x-ray), • Physiotherapy (Community or NUH), • Nottingham Back and Pain Team (via Advanced Nurse Practitioners), • Analgesia review, recommendations to GP, • Spinal injections (Dr Greg Hobbs), • Acupuncture (direct referral) or TENS (clinical nurse specialist), • Non urgent referrals to Spinal Surgeons, • Other e.g. Orthotics, NUH falls team. Recommendations for GP to instigate • from analgesia review, • regarding blood screening, • regarding urgent or routine referrals on to other specialists (non-spinal) e.g. rheumatology, orthopaedics, vascular or medical specialties, oncology, mental health team, • Any other recommendations e.g. referral to dietician/nutritionist, local exercise schemes, community falls team. Two stories of low back pain and right leg pain Neil - History • • • • • • • 47 year old police officer. 6/12 history of LBP with right buttock to calf pain. GP ordered bloods (NAD) and x-ray (L5/S1 changes). Able to remain at work but duties limited. Avoids prolonged sitting and driving due to pain. Affecting sleep, although amitriptyline helps. Paracetamol ineffective, previous gastric ulcer (avoids NSAIDs), and didn’t like side effects of codeine. • Temporary relief only with chiropractor (massage) and physiotherapy (exercise advice). Neil - Physical examination • Lumbar flexion increases buttock and leg pain. • Unable to fully straighten right hip/knee in standing or lying due to buttock and leg pain. • Slight reduction in right calf bulk. • Right hamstrings relatively weaker. • Right achilles reflex slightly dull, but present. • Reduced sensation great toe and sole of foot. Neil - Triage discussion • Lumbar MRI: Possible L5/S1 disc bulge with right S1 nerve root impingement. • Neil would consider nerve root block, but wants to avoid surgery and prefers not to use strong medication because he needs to concentrate at work. • Discussed possible diagnosis and prognosis, and agreed following MRI, options could be nerve root block if indicated and/or further physiotherapy. • For telephone review with results of MRI scan. Neil - Key considerations • Relatively acute – manage fears and expectations, explain diagnosis and reassure re prognosis. • Keep him out of secondary care, whilst this can still be managed conservatively. • Acknowledge and discuss concerns • Work demands and worries • Issues re analgesia use, side effects and work demands. • Support with advice, physiotherapy and nerve root block if indicated. • Longer term telephone follow-up via Clinical Nurse Specialist if required. Kathryn - History • 62 year old lady with long history of low back and right leg pain. • 2004 L4/5 discectomy. • 2008 developed right foot drop. • MRI showed L3/4 disc impinging right L4 nerve root. • Nerve conduction studies showed degeneration in the right peroneal nerve suggestive of proximal (spinal roots or plexus) lesion. • Under spinal clinic, had injections and eventually an L3/4 microdiscectomy 2010, with no improvement. Kathryn - Symptoms • No new symptoms since discharge from the spinal clinic in 2011. • Describes aching LBP radiating to thighs and knees in a generalised distribution. • Also has constant right dorsal ankle/foot pain, with episodes of numb spasm. • Pain worse with walking and walking distance limited to ¼ mile. • Owns a foot drop splint but never wears it because it is very uncomfortable with a poor fit. • Sleep disturbed by back, leg and foot pains. Kathryn – Treatment • Physiotherapy: Since discharge from the spinal clinic two full courses, including manual therapy, exercises, TENS and acupuncture. At the end of her last course 10 months ago, was told there wasn’t any more that physiotherapy could offer. • Analgesia: • Codeine based medication caused constipation. • Still takes paracetamol and ibuprofen prn, but doesn’t think it helps. • Currently weaning off gabapentin to change to pregabalin. She has had previous M.I. so has not been prescribed amitriptyline. Kathryn – Social and emotional impact • Kathryn owned a greengrocers, but had to give this up due to her back pain, and has not worked since. • She lives alone and her social contacts have reduced considerably in the last few years. • She keeps occupied by visiting her elderly father, and manages small spurts of housework resting between activities. She enjoys reading. • Her levels of pain concern her, because of how they limit her mobility and activity levels and her ability to care for her father. • She feels lonely and has been feeling very low recently. Kathryn – Physical examination • Limited lumbar range of movement all directions. • 0/5 power in right EHL and dorsiflexors. • All other right lower limb muscle groups 4/5. • Right achilles reflex dull but present. • Reduced sensation in her right great toe and lateral calf. • Loss of passive dorsiflexion in her right ankle. • Borderline allodynia dorsal right foot. Kathryn - Triage discussion • Discussion of mood, and whether she would like to access counselling or antidepressants via her GP. • Referral to Advanced Pain Nurse Specialist for assessment for CBT or ACT input including possible attendance at Nottingham Pain Management Programme. • Discussion with Pain Consultant regarding any further changes to analgesia, to be recommended to her GP. • Referral to Orthotics, NUH, for refitting of foot drop splint. Advice today re dorsiflexion stretches. • TENS was previously helpful but lost it. Book with Clinical Nurse Specialist for TENS issue and advice. Kathryn – Key considerations • Is just about coping but mood deteriorating. • Is despondent because thinks all treatment options have been exhausted, and because she feels people have given up on her. • Recognises there is no cure, but is hoping for improvements in her pain. • Has not fully explored CBT/ACT approaches. • Via community pain clinic, can access a wide range of services tailored to her particular needs. Questions?