PPT檔下載
advertisement
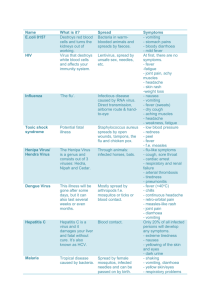
伊波拉病毒感染 診治與感染控制 2014.08.30 疾病管制署 蘇家彬醫師 大綱 伊波拉病毒感染的診斷 伊波拉病毒感染的治療與預防 感染控制措施簡介 結論 伊波拉病毒感染 的診斷 1.Tissue damage 2.SIRS 3.Coagulopathy 4.Immunity impairment Feldman, Lancet, 2010 臨床症狀 潛伏期 : 2-21 天 ( 平均 4-10 天) 症狀為突然發生 – 高燒、頭痛、冷顫、倦怠、肌肉痛 – 常見腸胃道症狀:嘔吐、腹瀉、腹痛 – 出血症狀(約45%) 輕微:點狀出血、流鼻血、瘀血、瘀傷 嚴重:腸胃道出血、休克、DIC – 較少見的症狀:出疹(軀幹、肩膀)、結膜炎、 咽喉炎、咳嗽、打嗝 Anthony S. Fauci, M.D. published on August 13, 2014, at NEJM.org 可能的病程發展 Day 0 – Nonspecific symptom/sign Day 5 – Skin rash – GI symptoms – Hemorrhagic symptoms Day 6 – 16 – Multiple organ failure – Septic shock – Mortality (55% in West Africa, 75% in Guinea) 可能的鑑別診斷 寄生蟲 – Malaria 細菌、立克次體 – typhoid fever, shigellosis, meningococcal disease , plague, leptospirosis, anthrax, relapsing fever, typhus, murine typhus… 病毒 – yellow fever, dengue fever, chikungunya fever, fulminant viral hepatitis… 病毒出血熱 Arenaviridae Bunyaviridae Filoviridae Flaviviridae Junin CrimeanCongo H.F. Ebola (Argentine) Paramyxoviridae Kyasanur Hendra virus Forest Disease (India) Machupo Hantavirus (Bolivia) Sabia (Brazil) Guanarito (Venezuela) Lassa (West Africa) Marburg Omsk H.F. (Russia ) Rift Valley fever Yellow Fever Dengue Nipah virus 實驗室檢驗發現 Leukopenia – lymphopenia followed by elevated neutrophils and a left shift Thrombocytopenia – 50,000 to 100,000 range Liver function elevation – multifocal hepatic necrosis Coagulation abnormalities – DIC Total plasma protein decrease – capillary leak syndrome 診斷方式 Viral isolation* – only in BSL4 laboratory Molecular detection – RT-PCR and Real-time RT-PCR (detects virus) Antigen ELISA (detects virus) IgM ELISA (detects early antibody) IgG ELISA (detects late antibody) IFA (Indirect Fluorescent Antibody) IHC (Immunohistochemistry) 實驗室診斷 Critical information: Date of onset of fever/symptoms IgM IgG viremia days post onset of symptoms 0 3 10 Fever RT-PCR IgM: up to 3 – 6 months ELISA IgM ELISA IgG IgG: up to 3 – 5 years (life-long persistance?) 採檢注意事項 The timing of specimen collection – It may take up to 3 days post-onset of symptoms for the virus to reach detectable levels Blood and sera are best specimens for testing in live patients Tissues (spleen, liver, others) may be tested if patient is deceased Oral swabs can also be used but not routine – not as sensitive, shorter window for positives, etc 伊波拉病毒感染的治療與預防 Dr. Kent Brantly 病患治療方式 以支持性治療為主 – – – – Fluids/electrolytes Oxygenation/Blood pressure Nutritional support Antibiotics to reduce secondary infection risk 研發中的治療方式 – Monoclonal antibodies – Antiviral treatment – Convalescent serum ZMappTM Mapp Biopharmaceutical Inc. A combination of three different monoclonal Nicotiana antibodies that bind to the protein of the Ebola virus Nonhuman primates study – Survival benefit : 24-48 hrs after infection – Still beneficial : fever and positive PCR Not yet in phase I clinical trials http://www.utsandiego.com/news/2014/aug /07/zmapp_drug_graphic/ 18 monkeys, 3 doses of the drug, 3, 4, and 5 days after Ebola virus infection All monkeys received the drug lived, and all three that didn't get the drug died TKM-Ebola An anti-Ebola RNA interference (RNAi) therapeutics Targeting the RNA polymerase L protein in virus Treat previously infected non-human primates – 100 percent protection from an otherwise lethal dose of Zaire Ebola virus Prepare for Phase I clinical study Geisbert et al., The Lancet, Vol 375, May 29, 2010 Other experimental treatments/vaccines Favipiravir (T-705) – suppressed replication of Zaire EBOV in cell culture – good response in animal model – novel broad-spectrum inhibitors of RNA viral infections (influenza……) BCX4430 – a viral RNA-dependent RNA polymerase (RdRp) inhibitor – treat a broad spectrum of viruses including Ebola – Postexposure prophylaxis ? Vaccines – adenovirus-based vaccines, VSIV(vesicular stomatitis virus)based vaccines, filovirus-like particles (VLPs)…… Antiviral Research Vol. 82, Issue 3, June 2009 Antiviral Research Vol. 105, May 2014 Samaritan's Purse AUGUST 21, 2014 Kent Brantly, MD, thanked people for their prayers and praised the staff and other groups for the care he received. Words from Bruce Ribner M.D. Emory's medical team learned a lot about treating the disease during Brantly and Writebol's hospitalizations, especially the importance of fluid and electrolyte replacement and insights on clotting problems It's not clear if the treatments helped or what the long-term sequelae will be in the wake of the measures. Lisa Schnirring | Staff Writer | CIDRAP News | Aug 21, 2014 感染控制措施 簡介 WHO statement In the outbreak, more than 225 health workers infected, nearly 130 dead The factors for health worker infection – Shortages and improper use of personal protective equipment (PPE) – Too few medical staff to respond to the outbreak – Compassion that prompts health workers to work beyond the number of hours recommended for safety reasons. http://www.who.int/mediacentre/news/statements/2014/health-worker-ebola/en/ 原則 接觸感染 經由破損的皮膚或黏膜 病患之血液、分泌物、體液(包含嘔吐物、 尿液、糞便、精液等)、器官等具有傳染性 疾病後期體內病毒量最高,傳染力最高 理論上病原體可能藉由空氣微粒(aerosols)傳 播,但尚未有相關案例報告 防護措施 醫療照護工作人員平時執行所有照護工作時, 都應確實遵從標準防護措施,落實手部衛生、 呼吸道衛生與咳嗽禮節 在照護伊波拉病毒感染的疑似和確定病例時, 則除了標準防護措施外,還應依據接觸傳染 防護及飛沫傳染防護原則,採行適當的防護 措施 如病患有嚴重肺炎症狀時,則建議採取空氣 傳染防護措施 通報個案處置 經醫師評估為伊波拉病毒感染通報病例或經 檢驗證實為確定病例時,應優先安置於負壓 隔離病房進行治療 若負壓隔離病室不敷使用,應安置於有衛浴 設備的單人病室 由於醫護人員照護疑似或確診病人被感染的 風險高過其他族群,因此除了配戴個人防護 配備,亦應嚴格地執行感染控制措施 個人防護裝備: 著裝 個人防護裝備: 卸裝 Boot remover 防護衣之分級 分級 裝備 防護 A級 (Level A) 防滲透之全身包覆式防護衣, 最高等級的呼吸系統保護及 配戴空氣呼吸器 皮膚保護 B級 (Level B) 防潑濺之化學防護衣,配戴 空氣呼吸器 提供對潑灑的防護,無法提 供對蒸氣的防護 C級 (Level C) 防潑濺之化學防護衣,配戴 全面式或半面式口罩 使用於已確認,可能隨空氣 散播的毒化物 D級 (Level D) 連身式防護衣,不須配戴呼 吸防護裝備 一般皮膚保護功能 訪客管制 訪客於進入醫院或病室前,應觀察是否有發 燒等感染症狀 建議限制訪客人數及行動路線與活動區域, 如非必要儘量勿讓訪客進入病室 應教導進入病室的訪客如何正確使用個人防 護裝備與執行手部衛生 其他訪客可在適當的距離(約15公尺)探視 病人 在顧及個資保護情況下留存所有訪客紀錄 照護個案注意事項 手部衛生 侵入性醫療措施 環境清潔與消毒 織品/布單與被服處理 廢棄物處理 遺體處理 工作人員暴露後處置 手部衛生五時機 before donning gloves and wearing PPE on entry to the isolation room/area before any clean/aseptic procedures being performed on a patient after any exposure risk or actual exposure with the patient’s blood and body fluids after touching (even potentially) contaminated surfaces/items/equipment in the patient’s surroundings after removal of PPE, upon leaving the care area 侵入性醫療措施 隔離病室內應有專屬儀器設備,盡量避免使 用可重複使用之儀器或醫材設備 非專用且非拋棄式的醫療設備於病人使用後, 依循廠商或醫院政策進行清潔消毒 減少不必要的針頭與刀片使用 抽血與檢驗應限於照護病患之最低需求 針頭不可回套或朝向身體 妥善密封並處理存放尖銳物品之容器 儘量避免執行的醫療處置 實驗室生物安全 避免進行非必要常規之臨床檢驗 – 考量是否排除感染後再進行 適當的防護裝備 – 雙層手套、面罩、防水實驗袍、N95口罩 盡可能使用密閉式全自動分析儀器 可能產生氣膠之步驟,應在Class II BSC進行 以500ppm含氯消毒劑消毒儀器設備 – 或根據原廠儀器操作手冊規定 環境清潔 負責清潔的人員應被告知需有額外的防護措 施,並經過適當的訓練 受汙染醫療環境應進行清潔消毒,清潔人員 務必穿戴防護配備(手套、N95口罩、連身型 防護衣、鞋套或防水長筒鞋套、護目裝備等) 若病人接觸過的物體無法在安全措施下消毒, 則應將物體火化 消毒方式 接觸到血液、分泌物、體液(包含嘔吐物、 尿液、糞便、精液等)、器官的環境表面應 立即使用消毒劑或1:100的稀釋漂白水 ( 500ppm )消毒 受到血液、分泌物、體液(包含嘔吐物、尿 液、糞便、精液等)、器官嚴重汙染的表面, 使用消毒劑或1:10的稀釋漂白水 ( 5000ppm )消毒 感謝 桃園縣政府衛生局 提供 織品/布單與被服 工作人員應依建議穿戴適當的個人防護裝備 處理使用過的被服及布單織品應盡量避免抖動,以 防止污染空氣、環境表面和人,並儘速送洗 離開病室前裝入標示明確、防水、密封的袋子或籃 子中,不可以直接帶出病室 使用清潔劑洗滌並沖洗乾淨後,使用1:100的稀 釋漂白水(500ppm)浸泡約30分鐘,再依常規標準 程序進行乾燥 若無法安全的處理或嚴重汙染,建議整袋以燒毀方 式處理 生物醫療廢棄物 處理廢棄物的人員應依建議穿戴適當的個人 防護裝備 所有廢棄物視同生物醫療廢棄物處理,處理 過程中應盡量避免攪動,並裝入防滲漏的袋 中或加蓋的容器中 液態的醫療廢棄物(如病人的嘔吐物、尿液 與糞便)可依規定倒入馬桶或衛生下水道由 汙水處理系統處理 處理過程中應注意避免噴濺 遺體處理 病人遺體運送過程中應使用防水性屍袋 工作人員搬運遺體裝入屍袋的過程中,應全 程依建議穿戴適當的個人防護裝備和不露腳 趾的鞋子 屍袋外面如有污物,應以1:10的稀釋漂白 水(5000ppm)抹拭 不可以打開屍袋瞻仰遺容、清洗遺體和進行 入殮準備,也不可對屍體進行防腐處理 遺體應依傳染病防治法規定儘速火化 暴露後處置 經皮膚或黏膜暴露到疑似或確定伊波拉病毒 感染病例的血液、分泌物、體液(包含嘔吐 物、尿液、糞便、精液等)、器官時,應立 即使用肥皂和清水清洗皮膚表面,黏膜(如 結膜)則應使用大量的清水或洗眼液沖洗 工作人員追蹤 未適當防護下接觸伊波拉病毒感染疑似或確 定病例之醫療照護工作人員 – 無症狀者應自主健康管理與接受醫療評估與追 蹤,包括每天2次的體溫監測,直到暴露後的第 21天為止 – 如出現發燒等症狀,應立即停止工作,通報單 位主管,在有症狀期間不應該繼續工作,並立 即接受所需之醫療協助 "As health care professionals, we strive to provide evidence-based care driven by science rather than by the media or mass hysteria. We need to apply these principles to planning for Ebola as well." 結論 料敵從寬 – 疫區回國人士出現發燒等症狀,提高警覺 – 不明原因出血熱,詢問旅遊史與接觸史 – 必要時,隔離病患,通報進行檢驗 禦敵從嚴 – – – – 一般病患:標準防護措施 疑似或確診病患:接觸與飛沫防護措施 良好的支持性治療 落實感染管制措施,保護醫療工作人員 故用兵之法,無恃其不來,恃 吾有以待也;無恃其不攻,恃 吾有所不可攻也。 孫子兵法‧九變篇