Lymphatic System
advertisement

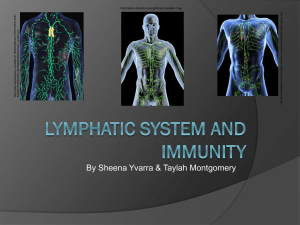
LYMPHATIC SYSTEM ST120: Concorde Career College Lymphatic System Objectives: Define the term lymph. Describe the functions of the lymphatic system. List and identify the structures of the lymphatic system and describe the function of each. Identify the origin of lymph. Lymphatic System Objectives: Trace the flow of lymph through the body. Describe the immune system and describe the immune response. Describe the mechanism by which the immune system helps to maintain homeostasis. Lymphatic System Objectives: Describe common diseases, disorders, and conditions of the lymphatic system including signs and symptoms, diagnosis, and available treatment options. Demonstrate knowledge of medical terminology related to the lymphatic system verbally and in the written form. Lymphatic System Functions of the Lymphatic System Removal of impurities Lymphocyte processing Lymphatic System The lymphatic system parallels (same direction)the circulatory system Lymph vessels return tissue fluid to the blood & protect the body against foreign material The lymphatic system includes: Lymph fluid Lymph vessels Lymph nodes Spleen Thymus And tonsils Lymph Fluid Lymph is the tissue fluid that enters and travels through the lymphatic vessels Plasma flows out of blood capillaries into tissue spaces (interstitial fluid) – AKA Tissue fluid Plasma diffuses out of the capillaries faster than it is reabsorbed, the remaining interstitial fluid is returned to the blood through the lymphatic system Lymphatic Capillaries Lymphatic Capillaries - Carry lymph and resemble blood capillaries Lacteals - Specialized lymphatic capillaries that carry chyle Lymph Vessels Vessels of the lymphatic system start with the smallest blind (dead-ended) lymph capillaries The walls of the lymphatic capillaries are a thin walled, single layer of loosely fit squamous epithelial cells making them highly permeable Lymphatic capillaries join larger lymphatic arterioles that then join lymphatic arteries Lymphatic vessels like the veins of the circulatory system have valves Lymph Flow Lymphatic System Relationship of Lymphatic Vessels to Circulatory System Thoracic Duct Lymph returns to the blood flow through the thoracic duct and the left subclavian vein Lymph from the lower body returns through the thoracic duct Cisterna chyli – dilation at the beginning of the thoracic duct (pouch-like structure) Lymph from a portion of the upper body also empties into the thoracic duct superior to the cisterna chyli Lymph from the upper left quadrant empties into the subclavian vein Two terminal vessels include: Right Lymphatic duct & thoracic duct Lymphahtic Drainage Lacteal Found in the villi of the small intestine Responsible for absorbing fat-soluble nutrients (fatty acids and vit. A,D,E & K) Fats are absorbed by the lacteals as chylomicron Chylomicron: combination of fatty acids and glycerol to form triglycerides Lacteal Lymph nodes and nodules Lymph Node: small ball shaped organs of the lymphatic system Lymph Nodules: groups of lymph cells located beneath the epithelial layer of mucus membranes (ex. Respiratory tract and digestive tract) Peyer’s patches: lymphatic nodules of the ileum Filters pathogens and foreign material before returning to blood Monitor the level of body fluid Hematopoietic function – produce lymphocytes, macrophages, and monocytes Located throughout the body Cervical Axillary Inguinal Regional Lymph Nodes Lymph node Hilus Afferent vessels x4 pg.261 A&P Efferent vessels x1 Capsule Germinal centers Sinuses Trabecula Tonsils Palatine Tonsils (throat) – located at each side of the oropharynx Pharyngeal (Adenoids) – located on the posterior wall of the nasopharynx Lingual Tonsils – located at the base of the tongue Tonsils Lymphedema Abnormal accumulation of fluid in interstitial spaces Causes: Obstruction of a lymphatic vessel (tumors, inflammation) Increased capillary BP Abnormal uptake of fluid by the lymphatic capillaries due to trauma or surgical wound (often seen after mastectomy) Lymphedema Lymphedema Terms Lymphadenitis: inflammation of lymph node/vessels Metastasis: is the spread of a disease from one organ or part to another non-adjacent organ or part, causing a new cancer site Lymphadenopathy: Any disease that usually involves the lymph glands Sentinel Lymph Node Biopsy Method developed to determine if breast cancer has spread to lymph ducts or nodes in the axilla Prevents the patient from having to undergo a lymph node dissection Sentinel Node: first node the breast drains to Nuclear Medicine A radioactive dye is injected into the area where the tumor is located as well as around the areola Hours later photos will reveal the pathway used to exit the breast, this will reveal the sentinel node OR Surgeon injects a blue dye into the breast that assists in visual of the nodes Small incision is made in the axilla A special probe picks up signals form the radioactive dye and gets “excited” when over an affected node All blue and radioactive nodes are removed Spleen Highly vascular and friable (easily crumbled/delicate) Located behind the stomach Contains lymphoid nodules (white pulp) Filters blood (red pulp) cleans out foreign materials/microorganisms Stores blood (approximately 200 ml) aids in maintenance of BP during severe hemorrhage Hematopoietic function: lymphocytes, monocytes, leukocytes, fixed plasma cells In a fetus the spleen produces erethrocytes Spleen Hilus Splenic artery Splenic vein Spleen cont. #1 organ injured in MVA’s (motor vehicle accidents) despite being protected by the lower ribs Splenectomy: surgical removal of the Spleen Lymphatic System Reticuloendothelial System Responsible for destruction of obsolete RBCs, bacteria, cancer cells, and other potentially harmful foreign substances. Utilizes monocytes distributed throughout the body such as Kupffer’s cells located in the liver Thymus Located in the mediastinum Composed of two lateral lobes bound by a connective tissue capsule Proper function dependent on thymosin Produces T-cells important in cell mediated immunity Thymus Lymphatic System Lymphatic and Immune Systems Thymus Bone marrow Spleen Tonsils Lymph nodes Lymph capillaries Lymph vessels Lymphocytes Lymph Lymphatic System Immunologic Defenses Provide the body with general defenses against disease. Nonspecific Defenses Specific Defenses Lymphatic System Nonspecific Defenses Chemical and Mechanical Barriers Phagocytosis Natural Killer Cells Inflammation Fever Interferon Lymphatic System Occurrence of Infection Not every exposure to a pathogen results in infection. Portal of Entry Virulence Toxins Dose Predisposition Lymphatic System Barriers Against Infection Chemical Body secretions Mechanical Skin Mucous Cilia membranes First Line of Defense Our first line of defense against microbes include: Skin Mucous membranes Secretions Skin Unbroken skin prevents microbes from entering the body (keratin) Broken skin such as Burns, Cuts, Scratches open the doors for an invasion of microbes such as Staphylococcus aureus Sweat glands and Sebaceous gland secrete acids that kill or inhibit the growth of bacteria on the skin Mucous Membranes Line tracts open to the exterior of the body (respiratory, digestive, urinary) Goblet cells secrete mucous to line the membranes and “catch” microbes Cilia catch and pass debris up to the pharynx to be expelled Glands in the stomach produce highly acidic gastric juice that kills most bacteria Helicobacter Pylori is an exception… can cause stomach and duodenal ulcers Second Line of Defense If pathogens penetrate the 1st line of defense they will encounter the body’s 2nd line of defense Circulatory and chemical defenses Circulatory Defenses: Phagocytes Complement proteins Iron Fever Inflammatory response Interferons Phagocytes Leukocytes responsible for phagocytosis Phagocytosis: the process of surrounding and ingesting another microbe Granulocytes Neutrophils – motile and effective phagocytes Eosinophils – attach to parasites and secrete peroxide ions which kill them. Play a larger phagocytic role during allergic response Basophils Agranulocytes Monocytes – enter body tissues and mature into stationary macrophages or travel through blood to infection site (wandering macrophages) Kupffer cells (liver), microglia (brain) Lymphocytes – are not phagocytes but are important in the immune response Phagocytosis Chemotaxis – chemicals attract phagocytes to injured tissues or bacteria Adherence – antibody molecules secrete a serum protein that can coat a bacterial cell and promote attachment (opsonization) Ingestion – phagocyte surrounds the microbe Pseudopods: “false feet” that extent to cover a microbe The resulting sac is called a Phagosome Digestion – phagosome is moved into the cytoplasm (phagolysosome) and enzymes (from the lysosomes) destroy the bacteria Degranulation – digestion process Complement proteins Group of 25-30 serum proteins found in blood plasma Circulate inactive until needed in the antibodyantigen reaction Activated Proteins: increase inflammatory response, assist in lysis of antigen, attracts phagocytes Complement cascade: sequence of proteins “bore” holes into bacteria causing an accumulation of fluid that eventually ruptures the cell Iron Virulence of bacteria increases when free iron is present Leukocytes: produce interleukin-1 (IL-1), stimulates the liver to store iron depriving bacteria of necessary free iron Inflammatory response Inflammation is a beneficial and necessary response to injury The four signs of inflammation include: Pain Heat Redness Swelling Three stages of inflammation include: Vasodilatation Phagocyte migration Tissue repair Inflammatory Response Vasodilation: Increased blood flow to area and increased permeability of blood vessels Histamine, kinins, and prostaglandins: chemicals released by damaged tissues responsible for vasodilatation Fever An abnormally elevated body temperature (controlled by hypothalamus) Systemic response frequently caused by viral or bacterial invasion Symptoms include heat, shivering and increased metabolism rate Vasodilatation and sweating signify the temperature falling “ fever breaking” Interferons- produced by T-cells Released to protect other cells by interferring with the ability of the virus to reproduce as it moves from cell to cell Proteins produced by leukocytes, T-lymphocytes, and fibroblasts in response to infection “interfere with viral replication” Proteins enter surrounding cells and inhibit the synthesis of proteins needed by invading viruses for multiplication They interfere with viral replication Pg. 269 A&P Third line of Defense Immune response: lymphocytes secrete antibodies that attach to microbes and inhibit or destroy them - Called humoral antibodies Formation of antibodies is stimulated by the presence of specific pathogens Effective circulating antibodies gives us our immunity Acquired Immunity Active acquired immunity: Immunity that develops after a person has had a disease Natural – individual has an infection and produces antibodies Artificial – vaccinations Passive acquired immunity Attenuation: process of weakening a pathogen Natural – antibodies pass through the placenta or in colostrum Artificial – antiserum (immune individual > susceptible individual) Pasteur – rabies vaccine Sabin – polio vaccine Lymphatic System Specific Defenses Immunity Final defense against disease Inborn (Passive) Acquired Natural (Active or Passive) Artificial (Active) Lymphatic System Inborn Immunity Species Racial Individual Lymphatic System Acquired Immunity Develops throughout the lifespan May occur naturally May be induced Lymphatic System Natural Acquired Immunity Active Contraction of the disease Antibodies protect from recurrence May be long term or life long Passive Mother to fetus via placenta Mother to infant via breast milk May last six months or slightly longer Lymphatic System Artificial Acquired Immunity Immunization Vaccines Live Weakened (attenuated) Dead Toxoid Recombinant DNA May be long term or life long Humoral Immunity Pg. 272 A&P Cell-mediated Immunity Pg. 272 A&P Antigens Any substance that the body regards as foreign and stimulates the production of antibodies aka is immunogenic Antibodies – A disease fighting protein created by the immune system in response to the presence of that specific antigen Immunoglobulins produced by B-lymphocytes Bind to receptor site of specific antigen B-lymphocytes mature into: Plasma cells – produce antibodies in response to an antigen (secretes them into blood) Memory cells – produces antibodies quickly when the body is exposed to the same antigen again Agammaglobulinemia: inability to produce antibodies (have no gammaglobulin) T-cells: Involved in cell-mediated immune response Lymphoid stem cells that migrate to the thymus Cytotoxic T cell: Helper T cells: Memory T cell: Natural killer cell: B-cells: Function in Humoral immunity pg. 272 A&P Organ Transplants Tissue Rejection: cells of the recipient do not recognize the tissue of the donor as self and attack/destroy the transplanted tissue To minimize chance of rejection recipients and donors tissue should be antigenically similar. Close family members are ideal donors Immunosuppressive drugs: suppresses recipients formation of antibodies/suppress the immune system Terms Isograft: genetically identical twin Allograft: close family member Xenograft: different species, Pig Anaphylactic Reaction Anaphylaxis: severe allergic reaction that can be lifethreatening Signs/Symptoms: Itching, swelling, difficulty breathing, hives, urticaria Severe difficulty breathing, laryngeal edema, bronchospasm Treatment: Epinephrine – bronchodilation, decrease laryngeal spasm, ^BP Steroid – inhibit reaction Levoped (vasopressor) - ^BP Ringer’s Lactate – Fluids Box13-4 Latex Allergy Many items used in the OR contain latex, daily exposure can cause a latex-sensitivity Latex allergic patients should be scheduled as the first case of the day in an OR so there is not latex dust in the room form previous surgeries Examples of latex in the OR Tape, elastic bandages, electrode pads, gloves, tourniquets, endotracheal tubes,………. Box 13-3 AIDS Acquired immunodeficiency syndrome (AIDS) Human immunodeficiency virus (HIV) has the most obvious effect in certain types of T-cells – virus that causes AIDS Characteristics: Vulnerability to opportunistic infections Major decrease in T-lymphocytes Kaposi’s Sarcoma Transmission: Sexual contact “dirty” hypodermic needles mother > fetus Blood transfusion Hemolytic Transfusion Reaction Occurs after a patient receives a transfusion of mismatched blood Agglutination: clustering and destruction of RBC’s Box 13-5 Autoimmunity Autoimmune disorder: the bodies immune system regards normal body tissues as foreign. Can not distinguish self from non-self Rheumatoid arthritis Ulcerative colitis MS Box 13-6