File - Department Of Pulmonary Medicine
advertisement

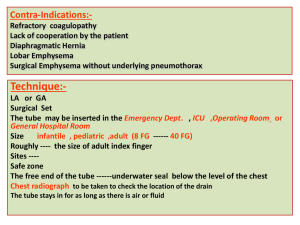
Dr. Navdeep Singh Junior resident Pulmonary medicine DEFINITION A chest drain is a tube inserted through the chest wall between the ribs and into the pleural cavity to allow drainage of air (pneumothorax), blood (haemothorax), fluid (pleural effusion) or pus (empyema) out of the chest. This allows drainage of the pleural contents and reexpansion of the lung. In the case of a pneumothorax or haemothorax this helps restore haemodynamic and respiratory stability by optimising ventilation/perfusion and minimizing mediastinal shift. INDICATIONS OF ITS USE • Pneumothorax not all pneumothoraces require insertion of a chest drain. Primary spontaneous pneumothorax :Patients with underlying lung disease and traumatic pneumothoraces usually require chest drainage. The differential diagnosis between a pneumothorax and bullous disease requires careful radiological assessment persistent or recurrent pneumothorax after simple aspiration tension pneumothorax should always be treated with a chest drain after initial relief with a small bore cannula or needle in any ventilated patient with a pneumothorax as the positive airway pressure will force air into the pleural cavity and quickly produce a tension pneumothorax large secondary spontaneous pneumothorax in patients over 50 years of age iatrogenic eg.following insertion of a central venous catheter. Not all will require drainage. Pleural effusion Pleural fluid Malignant pleural effusion Simple pleural effusions in ventilated patients Empyema and complicated parapneumonic pleural effusion Traumatic pneumothorax or haemopneumothorax Peri-operative eg. thoracotomy, oesophageal surgery, cardiothoracic surgery Insertion of a chest drain Before insertion of the chest drain: Consent Consent should be obtained and documented as per Trust guidance. The identity of the patient should be checked and the site and insertion of the chest drain confirmed by reviewing the clinical signs and the radiological information. PRE-DRAINAGE RISK ASSESSMENT Risk of haemorrhage: where possible, any coagulopathy or platelet defect should be corrected prior to chest drain insertion but routine measurement of the platelet count and prothrombin time are only recommended in patients with known risk factors. The differential diagnosis between a pneumothorax and bullous disease requires careful radiological assessment. Similarly it is important to differentiate between the presence of collapse and a pleural effusion when the chest radiograph shows a unilateral “whiteout”. Lung densely adherent to the chest wall throughout the hemithorax is an absolute contraindication to chest drain insertion. The drainage of a post pneumonectomy space should only be carried out by or after consultation with a cardiothoracic surgeon. EQUIPMENT Equipment required for insertion of chest drains. Sterile gloves and gown Skin antiseptic solution, e.g. iodine or chlorhexidine in alcohol Sterile drapes Gauze swabs A selection of syringes and needles (21–25 gauge) Local anaesthetic, e.g. lignocaine (lidocaine) 1% or 2% Scalpel and blade Suture (e.g. “1” silk) Instrument for blunt dissection (e.g. curved clamp) Guidewire with dilators (if small tube being used) Chest tube Connecting tubing Closed drainage system (including sterile water if underwater seal being used) Dressing Equipment may also be available in kit form. CONSENT AND PREMEDICATION Unless there are contraindications to its use, premedication (benzodiazepine or opioid) should be given to reduce patient distress. Premedication could be an intravenous anxiolytic—for example, midazolam 1–5 mg titrated to achieve adequate sedation—given immediately before the procedure or an intramuscular opioid given 1 hour before, although neither drug has e clearly superior. PATIENT POSITION The preferred position for drain insertion is on the bed, slightly rotated, with the arm on the side of the lesion behind the patient’s head to expose the axillary area. An alternative is for the patient to sit upright leaning over an adjacent table with a pillow or in the lateral decubitus position. Insertion should be in the “safe triangle” CONFIRMING SITE OF DRAIN INSERTION A chest tube should not be inserted without further image guidance if free air or fluid cannot be aspirated with a needle at the time of anaesthesia. Imaging should be used to select the appropriate site for chest tube placement. Fluoroscopy, ultrasonography, and CT scanning can all be used as adjunctive guides to the site of tube placement.Before insertion, air or fluid should be aspirated; if none is forthcoming, more complex imaging than a chest radiograph is required. The use of ultrasonography guided insertion is particularly useful for empyema and effusions as the diaphragm can be localised and the presence of loculations and pleural thickening defined. Using real time scanning at the time of the procedure can help to ensure that the placement is safe despite the movement of the diaphragm during respiration. The complication rate following image guided thoracocentesis is low with pneumothoraces occurring in approximately 3% of cases. Success rates of image guided chest tube insertion are reported to be 71–86%. TRIANGLE OF SAFETY ANTERIOR: LATERAL BORDER OF PECTORALIS MAJOR. LATERAL: LATERAL BORDER OF LATTISMUS DORSI/MID-AXILLARY LINE. INFERIOR: LINE IN 5TH INTERCOSTAL SPACE/ IMAGINARY HORIZONTAL LINE FROM NIPPLE. SUPERIOR: BASE OF AXILLA. SIGNIFICANCE:MINIMIZE THE RISK OF INJURY,BLOOD VESSEL,MUSCLES,HEART TISSUE AND INTERNAL MAMMARY ARTERY AND DECRREASED SCARING Insertion site Fourth or fifth intercostal space in the anterior axillary or mid-axillary line. Second intercostal space in the mid-clavicular line alternate site dissection through the pectoralis muscle leaves a visible scar loculated anterior pneumothorax with the use of a small bore catheter (10 to 14 Fr) rather than a standard chest tube. DRAIN SIZE Chest drains come in a range of sizes suitable for a variety of purposes (typically 10-36Ch) and may be inserted via an open surgical incision (thoracostomy) or using the Seldinger technique incorporating a guide wire and dilator system. The following chest drain tube sizes are available for use in adult patients within the Trust 12Ch 18 Ch 20Ch 28Ch 32Ch Specific Considerations How to choose a chest tube size? Pneumothorax — A 16 to 24 Fr chest tube. Traumatic pneumothorax — 28 to 40 Fr chest tube drainage of blood in addition to air may be necessary. Malignant effusion — A 20 to 24 Fr chest tube Empyema —28 to 36 Fr chest tube May need more than one tube for loculated areas Hemothorax — 32 to 40 Fr chest Larger caliber helps prevent occlusion Insertion of a small bore drain under image guidance with a guidewire does not require blunt dissection. These have been successfully used for pneumothorax, effusions, or loculated empyemas. Medium bore tube (16–24 F) Large bore tube (>24F): Large bore drains are recommended for drainage of acute haemothorax to monitor further blood loss. The use of large bore drains has previously been recommended as it was felt that there was an increase in the frequency of drain blockage, particularly by thick malignant or infected fluid. The majority of physicians now use smaller catheters (10–14 French (F)) and studies have shown that these are often as effective as larger bore tubes and are more comfortable and better tolerated by the patient The use of small bore pigtail catheters has allowed outpatient treatment of malignant pleural effusions which have not responded to chemotherapy. Empyemas are often successfully drained with ultrasonically placed small bore tubes with the aid of thrombolytic agents. In the case of acute haemothorax, however, large bore tubes (28–30 F minimum) continue to be recommended for their dual role of drainage of the thoracic cavity and assessment of continuing blood loss. ASEPTIC TECHNIQUE Aseptic technique should be employed during catheter insertion. Prophylactic antibiotics should be given in trauma cases. ANAESTHESIA Local anaesthetic should be infiltrated prior to insertion of the drain. Local anaesthetic is infiltrated into the site of insertion of the drain. A small gauge needle is used to raise a dermal bleb before deeper infiltration of the intercostal muscles and pleural surface. Local anaesthetic such as lignocaine (up to 3 mg/kg ) is usually infiltrated. Chest Tube Insertion chest tubes are inserted into the pleural space by four methods: 1. Tube thoracostomy with a guidewire and dilators. 2. Tube thoracostomy with a trocar. 3. Operative tube thoracostomy. 4. Tube thoracoscopy through a single-port thoracoscope Operative Tube Thoracostomy It is important to emphasize that operative tube thoracotomy can be very painful. Therefore, it is recommended that patients be given a narcotic or an anxiolytic medication 10 to 15 minutes before the procedure and that liberal doses of local anesthetic be used. To perform an operative tube thoracostomy, a 3- to 4cm incision is made in the skin parallel to the chosen intercostal space. The incision should be made down to the fascia overlying the intercostal muscle. This fascia is then incised throughout the length of the incision, with care taken not to cut the muscle. Once the fascia has been incised, the muscle fibers are spread with a blunt-tipped hemostat until the intercostal interspace is identified. Then, an incision is made in the intercostal fascia just above the superior border of the inferior rib over which the tube will pass. The parietal pleura is then penetrated by pushing a blunt-tipped hemostat through it. The hole in the parietal pleura is then enlarged by means of the operator's index finger. At this time, the operator should palpate the adjacent pleural space to detect any adhesions. Then, the chest tube with its distal end clamped is inserted into the pleural space. A hemostat is used to guide the tube into the pleural space as the operator's finger is withdrawn Operative tube thoracostomy. A: The physician's index finger is used to enlarge the opening and to explore the pleural space. B: Placement of chest tube intrapleurally using a large hemostat. Single-Port Thoracoscopy A rod-lens telescope was placed into the most proximal port of a 28 F chest tube. Then under direct visualization, the chest tube was placed into the costodiaphragmatic gutter and the telescope was removed. A flexible pleuroscope should not be used because of its larger diameter and potential for damage to the distal flexible portion of the scope when placed or removed from within the chest tube. Guidewire tube thoracostomy. A: Making a small skin incision slightly larger than the diameter of the chest tube. B: Introduction of 18-gauge needle into the pleural space. C: Insertion of wire with end into the pleural space. D: With guidewire in place, the tract is enlarged by advancing progressively larger dilators over the wire guide. Introduction of the dilators is facilitated by rotating and advancing the dilators in the same plane of the wire guide. E: Introduction of the chest tube inserter or chest tube assembly over the guidewire. F: The guidewire and the chest tube inserter have been removed, leaving the chest tube positioned within the pleural space. Trocar Tube Thoracostomy A: Insertion of trocar into the pleural space. Note the position of the hands, the position of the trocar relative to the ribs, and the cephalad position of the flat edge of the trocar. B: Insertion of chest tube through the trocar. COMPLICATIONS The most serious complications of tube thoracostomy are insertion of the tube ectopically, namely, into the lung, stomach, spleen, liver, or heart. These complications are more likely when a trocar chest tube is used. With the operative method, digital exploration of the insertion site delineates whether the tract leads into the pleural space and whether any tissue or organ is adherent to the parietal pleura at the planned site of tube insertion. Verification of Chest Tube Placement After the chest tube has been inserted and connected to a drainage system, a chest radiograph should be obtained to verify the correctness of its position. Ideally, both a posteroanterior (PA) and a lateral view should be obtained, because certain ectopic locations may not be apparent on the PA view alone. A CT scan should be obtained when the chest tube does not drain adequately and the chest radiograph is noncontributory. Draining systems: Prevent air & fluid from returning to the pleural space Most basic concept Tube open to atmosphere vents air Tube from patient Straw attached to chest tube from patient is placed under 2cm of fluid (water seal) Just like a straw in a drink, air can push through the straw, but air can’t be drawn back up the straw When the pleural pressure is positive, the pressure in the rigid straw becomes positive, and if the pressure inside the rigid straw is greater than the depth to which the straw is inserted into the saline solution, air (or liquid) will enter the bottle and will be vented to the atmosphere (or collect in the bottle). If the pleural pressure is negative, fluid will be drawn from the bottle into the rigid straw and no extra air will enter the system of the pleural space and the rigid straw. This system is called a water seal because the water in the bottle seals the pleural space from air or fluid from outside the body. Prevent air & fluid from returning to the pleural space This system works if only air is leaving the chest If fluid is draining, it will add to the fluid in the water seal, and increase the depth As the depth increases, it becomes harder for the air to push through a higher level of water, and could result in air staying in the chest Prevent air & fluid from returning to the pleural space Tube open to atmosphere vents air Tube from patient For drainage, a second bottle was added The first bottle collects 2cm fluid Fluid drainage the drainage The second bottle is the water seal With an extra bottle for drainage, the water seal will then remain at 2cm With this system, the bottle adjacent to the patient acts as a collection bottle for the drainage, and the second bottle provides the water seal and the air vent. Therefore, the degree of water seal does not increase as the drainage accumulates. The water-seal bottle functions identically in both the one and two-bottle systems. Restore negative pressure in the pleural space Tube to vacuum source Tube open to atmosphere vents air Tube from patient Straw under 20 cmH2O Fluid drainage Suction control 2cm fluid water seal Collection bottle It is desirable to apply negative pressure to the pleural space to facilitate reexpansion of the underlying lung or to expedite the removal of air or fluid from the pleural space. Suction at a fixed level, usually -15 to -20 cm H2O, can be applied to the vent on a one- or two-bottle collection system with an Emerson pump. Three-bottle systems are unwieldy to set up and are cumbersome to move if the patient needs to be transported. Following insertion of the chest drain it is essential to :• check the underwater seal oscillates during respiration • order a repeat chest x-ray to confirm the position of the tube and the degree of lung re-expansion and exclude any complication advise the patient to keep the underwater bottle below the drain insertion site,` upright and avoid compressing the tube by sitting or lying on it • ensure regular analgesia is prescribed whilst the chest drain is in place Commercially Available Drainage Systems An acceptable drainage system should have the following characteristics: (a) the water seal should be easily visualized, so one can determine whether the chest tube is patent and whether an air leak is present. Some systems have a one-way valve that does not contain water, but one can (and should, if dealing with a pneumothorax) fill the chamber with water to view the bubbling. (b) the tube should be functional when no suction is applied. (c) the volume of the collection chamber should be adequate and the markings should be such that the drainage is easily quantitated. (d) there should be a pop-off valve to provide a safety factor if pressure builds up in the system. Pleur-Evac Unit Pleur-Evac collection system, which is analogous to a three-bottle collection system. The area labeled C is the calibrated collection system; W is the water-seal chamber; S is the suction-control chamber. Arrows demonstrate the pathway for air to leave the pleural space. If the suction vent is left open to atmospheric pressure, the Pleur-Evac system functions as a two-bottle collection system. When suction is applied, atmospheric air enters through S and leaves through the suction apparatus. Care of a Chest Tube Is there bubbling through the water-seal bottle or the water-seal chamber on the disposable unit? Is the tube functioning? What is the amount and type of drainage from the tube? Bubbling through Water-Seal Chamber If the patient is receiving water-seal drainage without suction, the presence of bubbling in the water seal usually indicates a persistent air leak from the lung into the pleural space. If no air bubbles are seen on the initial inspection of the water seal, the patient should be asked to cough, and the water seal should be observed for bubbling. The coughing maneuver increases the patient's pleural pressure and should demonstrate small air leaks into the pleural space. If the patient is receiving suction, disconnection or partial disconnection anywhere between the water seal and the patient will lead to bubbling through the water seal Leaks in the system may be detected by clamping the chest tube at the point where it exits from the chest. If bubbling through the water seal persists, the drainage system itself is responsible for the leak, and it should be examined thoroughly for leaks. If the bubbling stops when the chest tube is clamped, then the air is coming from the pleural space. The presence of bubbling through the water seal does not necessarily indicate a communication between the lung and the pleural space. If the chest tube is not inserted far enough into the pleural space, one or more of the holes in the chest tube may lie outside the pleural space. Patients with poor tissue turgor, the negative pleural pressure will cause air to enter the pleural space around the chest tube at the insertion site. At times it may be difficult to tell whether the air is leaking around the chest tube or whether it is due to a bronchopleural fistula. One may make this differentiation by measuring the level of PCO2 in the air coming from the chest tube. Is the Chest Tube Functioning? If the patient is not receiving suction, one should observe the level of the liquid in the water seal. If the chest tube is patent and in the pleural space, the level of the liquid should move higher on inspiration in the limb of the water seal proximal to the patient, indicating a more negative pleural pressure. Of course, if the patient is receiving mechanical ventilation, the level of liquid in the proximal limb will go down on inspiration because the pleural pressure becomes more positive. When no fluctuations are observed synchronous with respiratory movements, the patient should be asked to make a maximal inspiratory effort, and if still no movement is observed, it indicates that the chest tube is not functioning. If a chest tube is not functioning, its functional status should be restored, or it should be removed. Chest tubes can become obstructed with tissue around the holes or by clots within the tube. The simplest method for restoring patency is to flush the tube with 50 mL of saline. Amount and Type of Drainage The amount and the character of the drainage from the chest tube should be recorded for each 24-hour period. The amount of drainage is most easily quantitated by marking the level of the liquid in the collection chamber each day. This record-keeping is important because many therapeutic decisions based on the quantity of the drainage. The character of the drainage is best described by quantitating the percentage of solid drainage material. This quantitation is easily done by marking the level of the sediment in the collection chamber each day. If the increase in volume of the entire collection system is known and if the increase in volume of the solid sediment is known, it is simple to calculate what percentage of the daily drainage is solid. Monitoring/recording The frequency of observations depends on clinical presentation/progress and medical request but should happen at least 4 hourly. Fluid within the tube should swing with respiration due to changes in intrapleural pressure. With normal respiration, the fluid should rise on inspiration and fall on expiration. Absence of swinging indicates that the drain is occluded or is no longer in the pleural space. It may be necessary following clinical assessment and unsuccessful flushing of the drain to obtain a chest xray to determine the underlying cause. A drain inserted for drainage of a haemothorax (+/- pneumothorax) needs blood loss to be recorded accurately with any sudden increases in drain volume referred immediately for medical review. With fractured ribs most bleeding is from the intercostal vessels, which slows down as the lung reinflates. However continued bleeding into the drain bottle is indicative of pathology that may need thoracic surgical intervention. After thoracic trauma more than 1500ml of blood into the bottle initially or continued bleeding of greater than 200ml/hr requires discussion with the thoracic surgeons. When to clamp? Clamping drain A bubbling chest tube should never be clamped. Drainage of a large pleural effusion should be controlled to prevent the potential complication of reexpansion pulmonary oedema. In cases of pneumothorax, clamping of the chest tube should usually be avoided. If a chest tube for pneumothorax is clamped, this should be under the supervision of a respiratory physician or thoracic surgeon, the patient should be managed in a specialist ward with experienced nursing staff, and the patient should not leave the ward environment. If a patient with a clamped drain becomes breathless or develops subcutaneous emphysema, the drain must be immediately unclamped and medical advice sought. Changing the drain bottle When changing the drain bottle because it is overfull, temporary clamping of the drainage tube may be necessary to prevent ingress of air into the pleural cavity. It is acceptable to clamp the tube between thumb and forefinger. This has the advantage of removing the risk of inadvertently leaving the tube clamped. Suction A patient who is free from pain, to the degree that an effective cough can be produced, will generate a much higher pleural pressure differential than can safely be produced with suction. This combined with a functional underwater seal will result in re-inflation of the lung. If a patient cannot re-inflate his own lung or persistent air leak is preventing re-inflation, high volume, lowpressure thoracic suction in the range of 3-5kPa (approx 30-50cmH2O) should be used. Mobility If appropriate, patients should be encouraged to walk around. If the drain is on suction the patient will be restricted to the bedside. Exercise to prevent complications such as a frozen shoulder or deep venous thrombosis is essential, as are deep breathing exercises to aid re-expansion of the lung. Dressings Dressings should be changed daily for the following reasons:to enable the insertion site to be monitored for signs of infection. A swab should be taken from the chest drain site if there are any clinical signs of infection - to monitor for surgical emphysema - to ensure the chest drain remains well placed and the anchor suture is in tact complications Are rare, 1-3% Chest tube malposition — Chest tube malposition is the most common complication of tube thoracostomy Lung parenchyma perforation Empyema Subcutaneous tube placement Perforation of the ventricle or atrium, and abdominal organs (spleen, liver, stomach, colon) Other complications include cardiogenic shock from chest tube compression of the right ventricle, mediastinal perforation with contralateral hemothorax and pneumothorax bleeding from intercostal artery injury infection at the chest tube site 1. One of the most common complications is misplacement of the chest tube. 2. Many life-threatening complications occur when the tube is first inserted and include insertion of the chest tube into the lung, stomach, spleen, liver, or heart. 3. A PA and lateral chest radiograph should always be obtained after a chest tube is inserted. 4. Pleural infection is another complication of tube thoracostomy. The administration of antibiotics to patients who have chest tubes for thoracic trauma may decrease the prevalence of empyema. 5. The antibiotic chosen should have activity against Staphylococcus aureus because this is the organism that causes the most infections. subcutaneous emphysema, which usually presents as soft tissue crepitus around the drain site but may rapidly spread to virtually any place in the body. The presence of subcutaneous emphysema in patients with tube thoracostomies indicates one of three possibilities : (a) a side-hole on the chest tube is lying outside the pleural space within the chest wall, allowing air to enter the tissue planes (b) the chest tube is blocked. (c) the drainage system cannot cope with the air leak. The latter situation is unusual and may be related to a chest tube that is too small or a massive air leak. Injection of Materials Through Chest Tubes Fibrinolytic or a DNAase in a patient with a loculated complicated parapneumonic effusion . Tetracycline derivative or a different sclerosing agent through the chest tube in a patient with a malignant pleural effusion. There is a commercially available adapter called a Thal-Quick Chest Tube Adapter . CHEST TUBE REMOVAL Remove when: Original indication for placement is no longer present Tube becomes nonfunctional. The following criteria should be met prior to removing the chest tube: The lung should be fully expanded Daily fluid output should be less than 100 to 200 mL/day An air leak should not exist, either during suction or coughing Once these criteria are met, the chest tube can be placed on water seal. CXR on water seal after 6 hours Some will clamp the chest tube for four to six hours, then confirm the absence of pneumothorax prior to removing the chest tube. Mechanical ventilation does not prevent removal of CT if no air leak is present. Following inspiration, the patient performs a Valsalva maneuver and the tube is removed with simultaneous covering of the insertion site with the gauze dressing In case Parapneumonic Effusions and Empyema chest tubes should be left in place until the volume of the pleural drainage is less than 50 mL for 24 hours and until the draining fluid becomes clear yellow. The amount of sediment (representing WBCs and debris) in the collection system should be quantitated daily and the chest tube should not be removed if more than 5 mL sediments collect daily. In case of pneumothorax The chest tube should remain in place for 24 hours after the lung reexpands and the air leak ceases. If the chest tubes are removed too soon after the lung reexpands and the air leak ceases, there is a high likelihood of an early recurrence if removed within 6 hours of expansion. Thoracentesis Thoracentesis also known as thoracocentesis or pleural tap is an invasive procedure to remove air or fluid from pleural space for diagnostic and therapeutic purposes. INDICATIONS for Diagnostic thoracentesis Establish the cause of a pleural effusion. When an effusion is suspected on physical examination Confirm by radiographic Thoracentesis is not generally required in patients: Small amount of pleural fluid And a secure clinical diagnosis (eg, with viral pleurisy) Thoracentesis should be considered in patients with suspected CHF in the following circumstances: A unilateral effusion is present, particularly if it is left-sided Bilateral effusions are present, but are of disparate sizes There is evidence of pleurisy The patient is febrile The cardiac silhouette appears normal on chest radiograph The alveolar-arterial oxygen gradient is widened out of proportion to the clinical setting CONTRAINDICATIONS There are no absolute contraindications to diagnostic thoracentesis Relative contraindications to the procedure: Anticoagulation or a bleeding diathesis PT or PTT greater than twice normal Platelet count less than 25,000/mm3 Serum creatinine concentration greater than 6 mg/dL Active skin infection at the point of needle insertion A very small volume of pleural fluid <1 cm distance from the pleural fluid line to the chest wall on a decubitus radiograph risk of thoracentesis generally outweighs the usefulness of pleural fluid analysis Mechanical ventilation does not increase the risk for developing a pneumothorax compared with nonventilated patients. however, mechanically ventilated patients are at increased risk of developing tension physiology or persistent air leak (bronchopleural fistula) if a pneumothorax does occur. Selection of Site Site can be confirmed by: Chest x-ray Chest ultrasound When fluid is present between the lung and the chest wall, tactile fremitus is lost, and the light percussion note becomes dull. Accordingly, thoracentesis should be attempted one interspace below the spot where tactile fremitus is lost and the percussion note becomes dull. Thoracentesis should usually be performed posteriorly several inches from the spine, where the ribs are easily palpated. The exact location for the thoracentesis attempt should be just superior to a rib. The rationale for this location is that the arteries, veins, and nerves run just inferior to the ribs (Fig. 28.2), so that if the needle is just superior to a rib, the danger of damage to these structures is minimized physical exam in the diagnosis of pleural effusion: • percussion • auscultatory percussion • breath sounds • chest expansion • tactile vocal fremitus • vocal resonance • crackles • pleural friction rub Thoracocentesis kit Basic materials: Lidocaine 1% or 2% Aqueous heparin, 1000 U/mL Atropine Antiseptic solution Alcohol swabs Sterile gloves Six 4 × 4-in. gauze pads Sterile drape with center hole Sterile drape (to cover bed) Adhesive tape Two 5- to 10-mL syringes One 50- to 60-mL syringe One No. 25 needle, 5/8 in. long Two No. 20 to No. 22 needles, 1.5 in. long Band-aids Additional materials for therapeutic thoracentesis Two No. 14 needles and catheters One 3-way stopcock One sterile container for pleural fluid One 50-mL syringe (additional Positioning of Patient Technique A: The skin is injected using a 25-gauge needle with a local anesthetic agent. B: The periosteum is injected with the local anesthetic. C: The pleural space is entered and pleural fluid is obtained. D: The thoracentesis attempt is too high, and air bubbles are obtained. E: The thoracentesis attempt is too low, and neither bubbles nor fluid is obtained. COMPLICATIONS Pain at the puncture site Bleeding Hematoma Hemothorax Hemoperitoneum Pneumothorax (12-30%) Empyema Soft tissue infection Spleen or liver puncture Make sure sitting upright Vasovagal events Seeding the needle tract with tumor Retained intrapleural catheter fragments have been reported. Therapeutic aspiration Indications The three main indications for therapeutic thoracentesis are to remove the pleural fluid in patients with parapneumonic effusions or empyema, to relieve the symptom of dyspnea secondary to a pleural effusion to remove the pleural fluid so that the status of the lung underlying a pleural effusion can be evaluated Technique A: A standard 14-gauge needle attached to a syringe is introduced into the pleural space. B: A 14-gauge catheter is threaded through the needle and is directed down toward the costodiaphragmatic recess. C: The needle is withdrawn from the pleural space, and its end is covered immediately with the guard. Fluid can be withdrawn from the pleural space using the three-way stopcock and the syringe. How much pleural fluid can be withdrawn large volumes of pleural fluid can be removed safely if the pleural pressure is monitored during thoracentesis and if thoracentesis is terminated when the pleural pressure falls below -20 cm H2O (26). Pleural pressure can be monitored by a U-shaped manometer. procedure should be terminated if the patient developed chest pain, more than minimal coughing, or shortness of breath, or if no more fluid could be obtained. complications Therapeutic thoracentesis is associated with the same complications as diagnostic thoracentesis, including vasovagal reaction, pneumothorax, pleural infection, and hemothorax. In addition, reexpansion pulmonary edema and hypovolemia may complicate therapeutic thoracentesis. Reexpansion pulmonary edema — Potentially life-threatening complication of tube thoracostomy It usually occurs unilaterally after rapid reexpansion of a collapsed lung in patients with a pneumothorax Can also follow evacuation of large volumes of pleural fluid (>1.0 to 1.5 liters) or after removal of an obstructing tumor. The incidence of edema appears to be related to the rapidity of lung reexpansion. Patients typically present soon after the inciting event, although presentation can be delayed for up to 24 hours in some cases. A mortality rate as high as 20 percent has been described. Treatment is supportive, mainly consisting of supplemental oxygen and, if necessary, mechanical ventilation. The disease is usually self-limited. Prevention — drain only 1-1.5 liters of fluid at a time; if need to take more, wait 2-4 hours between drainages Fibrinolytics Definition: are Drugs that cause lysis of already formed thrombus Fibrinolyic drugs 1. Streptokinase. 2. Anistreplase. 3. Urokinase 4. Tissue plasminogen activators ( t -PA). Mechanism of Action acts directly or indirectly to convert plasminogen to plasmin within the thrombus Plasmin degrades fibrin clots and other plasma proteins (non-fibrin specific) Use of fibrinolytics in pulmonolgy Fibrinolytic agents are used to allow complete drainage of locules and partial debridement of the pleural surface. Instillation of fibrinolytics into the pleural cavity may help prevent fibrin deposits and loculations. Clinical success rate ranges from 62 to 100 percent Streptokinase Is a protein synthesized by B-hemolytic streptococci. Mechanism of Action acts indirectly by forming plasminogen-streptokinase complex which converts inactive plasminogen into active plasmin. It is the least expensive. T 1/2 = half an hour. 1.5 million units of stk is used. Side effects 1. Bleeding due to activation of circulating plasminogen. 2. Hypersensitivity due to antigenicity (rash, fever, allergic reaction). 3. Hypotension. 4. not used in patients with streptococcal infections (have antistreptococcal antibodies and may develop fever, allergic reactions and resistance upon treatment with streptokinase). Disadvantages (less than streptokinase alone). 1. Expensive. 2. Antigenic. 3. Allergic reactions. 4. Bleeding due to minimal fibrin specificity Urokinase Human enzyme synthesized by the kidney, obtained from either urine or cultures of human embryonic kidney cells. acts directly converting plasminogen to active plasmin. urokinase is also effective when compared to saline alone for intrapleural treatment of loculated parapneumonic effusions. Compared with placebo, intrapleural instillation of urokinase is effective in improving chest-tube drainage and the radiographic appearance of the chest; early use of urokinase may be more effective than late use when catheter drainage alone has failed. Comparison of urokinasewith streptokinase shows no difference in effectiveness. Disadvantages 1. Expensive. 2. Systemic lysis. Advantages 1. Not antigenic. 2. No Hypotension. Tissue Plasminogen Activators ( t - PA ) Alteplase • • Alteplase ( Single Chain ). Reteplase ( Deleted Form ). Tenecteplase All are recombinant human t - PA. Synthesis by recombinant DNA technology. Tissue plasminogen activator (t-PA) has been shown to be effective in reducing the duration of required chest tube placement in children with complicated parapneumonic effusions (using 4 mg of t-PA in 30 to 50 ml of saline instilled through the chest , which is clamped for 1 hour before applying suction to the tube). No adverse events have been noted. In our practice, 10 mg of t-PA in 50 ml of saline is instilled through the chest catheter, followed by 20 ml of a saline “flush.” If possible, the patient’s position is every 10 min for1hbefore the catheter is connected to suction. complications of intrapleural fibrinolysis hemorrhage, allergic reactions, transient chest pain promotion of bronchopleural fistula formation. intrapleural instillation of thrombolytic agents may alter systemic coagulation parameters, many studies have shown that this effect does not occur. Contraindications to thrombolytic therapy Absolute contraindications include: Recent head trauma or caranial tumor Previous hemorrhagic shock Stroke Active internal bleeding Major surgery within two weeks Relative contraindications include: Active peptic ulcer, diabetic retinopathy, pregnancy, uncontrolled hypertension Thank you