Thank you for joining us!
Our webcast, ‘Ambulation and Secondary
Conditions after SCI,’ will begin at 12:00PM EDT.
Ambulation and Secondary
Complications after SCI
Lee L. Saunders, PhD
Medical University of South Carolina
May 22, 2014
Acknowledgement
• The contents of this presentation were developed under
grants from the Department of Education, NIDRR grant
numbers H133B090005, H133G090059, and H133G050165
and a grant from the National Institutes of Health (NIH),
1R01 NS 48117. However, those contents do not
necessarily represent the policy of the Department of
Education or NIH, and you should not assume
endorsement by the Federal Government.
Collaborators
• James S. Krause, PhD (Principal Investigator)
• Sandra S. Brotherton, PhD, PT (Co-I)
• Sara Kraft, DPT (Co-I)
• David C. Morrisette, PhD, PT (Co-I)
• Student Contributors:
o Nicole D. DiPiro, MS
o Ryan K. Kohout, MD
Objectives
1. Identify the relationship between prescription
medication use and ability to ambulate
distances after SCI.
2. Identify secondary complications related to
assistive walking devices after SCI.
3. Identify the relationship of assistive walking
devices and fall-related injuries after SCI.
Background
• Traumatic spinal cord injury (SCI) is a severe
disabling condition that occurs suddenly and
generally results in permanent sensory and motor
loss.
• Frequently leads to secondary health conditions
that are particularly devastating as they restrict
participation, reduce quality of life (QOL), and
diminish life expectancy.
Background
• The proportion of persons with incomplete SCI
has increased in recent years, most likely due to a
number of factors, including improved techniques
for emergency management.(NSCISC, 2013)
• There are a substantial number of individuals with
incomplete SCI and lower-level lesions who retain
or redevelop the ability to walk to differing
degrees.(Morganti, Scivoletto, Ditunno, Ditunno, & Molinari, 2005; New, 2005;
Wirz et al., 2005)
Background
• Ambulation has been associated with many
positive improvements in both physical health
and subjective well being.
Preliminary Studies
• Persons with SCI who are ambulatory have
shown:
• Higher risk of subsequent injury
• Higher risk of falls
(Krause, 2004)
(Brotherton et al., 2006)
• Among those ambulatory, persons dependent
on others for assistance in walking have
shown:
• Higher levels of pain interference and prescription
pain medication use (Krause et al., 2007a)
• Greater risk of a depressive disorder, however this
relationship was mediated by pain interference (Krause
et al., 2007b)
Purpose
• While studies have shown short-term benefits of
gait training for people with SCI, some research
suggests there may be unforeseen long-term
adverse consequences of ambulation.
• The purpose of this research study was to identify
variations in ambulation after SCI based on use of
assistive devices and/or reliance on people for
ambulation, functionality of ambulation
(distances), and their association with secondary
conditions.
Methods
• IRB approval through MUSC.
• Participants were part of a larger longitudinal
study of health outcomes after SCI.
• Identified through records of a large rehabilitation
hospital in the Southeastern US.
• Inclusion criteria:
o 18+ years at assessment
o 1+ years post-injury
o Traumatic SCI with residual impairment
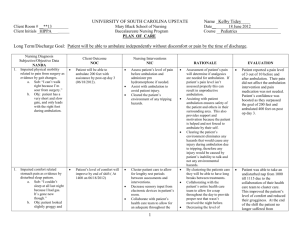
Participants
• Those who reported at least some ambulation
were included:
o Are you able to walk at all? Yes/No
• Overall of 1,689 participants, 31.3% reported
being ambulatory (n=529).
• Those responding yes were asked a series of
follow-up questions regarding:
o Distance, assistive devices, portion of time spent
ambulating around the home and community
o Secondary health conditions
Ambulation Questions
Participant Demographics
Characteristic
Ambulatory
Non-ambulatory
Gender
p
0.0023
Male
69.6
76.6
Female
30.4
23.5
Race
0.1272
White
72.4
73.2
Black
20.6
22.2
Other
7.0
4.7
Injury Level
<.0001
C1-C4
24.4
14.4
C5-C8
31.6
36.8
Non-cervical
44.0
48.8
Age at Assessment
50.0 (14.2)
47.7 (12.7)
0.0010
Years Post-injury
13.6 (8.5)
17.0
<.0001
RESULTS
Reliance on Devices and People
for Walking and Ability to Walk
Community Distances
Brotherton, S.S., Saunders, L.L., Krause, J.S., & Morrisette, D.C. (2012).
Association between reliance on devices and people for walking and ability
to walk community distances among individuals with spinal cord injury.
Journal of Spinal Cord Medicine, 35(3), 156-161.
Reliance on Devices
• Purpose: To identify and describe maximum
walking distances and the reliance on assistive
devices and/or people.
• Distances:
o Maximum Walking Distance
• 10m, 150ft, 1000ft
o Able to climb stairs
• Yes/No
• Devices
o Walker, cane(s), crutch(es), long leg brace(s), short leg
brace(s) people
Ambulation
• 4.3% could not walk 10 meters (~33 ft)
• 20.6% could walk 10 meters (but not 150 ft)
• 27.8% could walk 150 ft (but not 1000 ft)
• 47.3% could walk 1000 feet
• 72.1% could walk up a flight of 12-14 stairs
Ambulation
• Home
o 71.5% walk a majority of
the time
o 5.7% walk/wheel 50/50
o 22.8% wheel a majority
of the time
• Community
o 68.8% walk a majority of
the time
o 4.3% walk/wheel 50/50
o 26.8% wheel a majority
of the time
Reliance on Devices
• 33.4% did not use devices or people to assist in
ambulation
• 30.2% used one device or a person
• 22.7% used 2
• 13.7% used 3+
Reliance on Devices
• 25.1% used a walker
• 20.6% used a crutch(es)
• 34.1% used a cane(s)
• 6.8% used a long leg brace(s)
• 21.7% used a short leg brace(s)
• 11.3% used another person for assistance
Relationship between Prescription
Medication Use and Ability to
Ambulate Distances
Kohout, R., Saunders, L.L., & Krause, J.S. (2011). The relationship
between prescription medication use and ability to ambulate
distances after spinal cord injury. Archives of Physical Medicine and
Rehabilitation, 92, 1246-1249.
Prescription Medication and Distances
• To investigate the association of prescription
medication for spasticity and pain with maximum
ambulatory distance.
• Primary Outcome: Maximum walking distance
o <150m, <1000ft, 1000ft+
Prescription Medication and Distances
• Primary Predictor
o Prescription medication use for pain or spasticity
• Minor – never, sometimes
• Heavy – weekly, daily
• Control Variables
o Gender (male, female)
o Race (white, black)
o Injury level (cervical, non-cervical)
o Pain severity (Brief Pain Inventory Score)
Prescription Medication and Distances
Variable
Maximum Walking Distance (ft)
>1000
150-999
<150
p-value
0.0508
Sex
Male
51.3
27.1
21.6
Female
46.6
19.6
33.8
0.0194
Race
White
52.9
22.2
25.0
Black
38.4
33.7
27.9
0.6392
Injury level
Cervical
51.7
23.9
24.4
Non-cervical
47.8
25.4
26.9
<.0001
Prescription use
Heavy
35.0
30.4
34.6
Minor
67.0
17.8
15.1
42.6±13.6
45.6±14.4
50.5±14.7
0.0061
2.6±2.1
3.8±2.6
4.3 ±2.5
<.0001
Age
Pain Severity
Prescription Medication and Distances
Variable
Walk <150
Walk 150-999ft
OR (95% CI)
p-value
Male (vs. Female)
0.51 (0.30-0.90)
1.14 (0.64-2.01)
0.019
White (vs. Black)
0.67 (0.34-1.32)
0.45 (0.24-0.83)
0.87
Cervical (vs. Non-C)
1.49 (0.85-2.60)
1.61 (0.95-2.76)
0.236
Age
1.04 (1.02-1.06)
1.01 (0.99-1.03)
<.001
Pain Severity
1.21 (1.08-1.36)
1.11 (0.99-1.24)
0.003
Heavy medication
(v. minor)
2.82 (1.57-5.04)
2.52 (1.45-4.39)
<.001
Conclusions
• Heavy prescription medication use for pain and
spasticity was inversely related to a person’s
ability to achieve community ambulation
distances of 1000ft or more.
• Results may provide insight for clinicians involved
in medication management for those with SCI.
Ambulation and Secondary
Complications Related to
Devices after SCI
Saunders, L.L., Krause, J.S., DiPiro, N.D., Kraft, S., & Brotherton, S.
(2013). Ambulation and secondary complications related to devices
after spinal cord injury. Journal of Spinal Cord Medicine, 36(6), 652659.
Devices and Secondary Complications
• Purpose: To assess pain intensity, pain
interference, and fatigue among persons with SCI
who are ambulatory.
• Primary outcomes:
o Pain Intensity (Brief Pain Inventory)
o Pain Interference (Brief Pain Inventory)
o Fatigue (Modified Fatigue Impact Scale)
Devices and Secondary Complications
• Primary Predictors:
o Wheel chair use (None, 50% or less, 51% or more)
o Assistance from people (yes, no)
o Long leg braces (0, 1, 2)
o Short leg braces (0, 1, 2)
o Cane (0, 1, 2)
o Crutches (0, 1, 2)
o Walker (yes, no)
Devices and Secondary Complications
High Pain
Intensity*
Wheel chair (v. none)
p
High Pain
Interference*
0.0010
<.0001
50% or less
2.05 (1.39-3.03)
2.11 (1.43-3.12)
51% or more
1.04 (0.75-1.44)
0.72 (0.51-1.02)
People (v. no)
Yes
0.0442
1.51 (1.01-2.27)
Cane (v. none)
0.1232
1.38 (0.92-2.09)
0.0006
<.0001
Unilateral (1)
1.86 (1.35-2.56)
2.11 (1.52-2.93)
Bilateral (2)
1.61 (0.78-3.32)
1.67 (0.79-3.46)
Long leg brace (v. none)
0.0625
0959
Unilateral (1)
2.06 (1.21-3.77)
1.60 (0.86-2.95)
Bilateral (2)
0.95 (0.52-1.73)
0.60 (0.30-1.19)
*controlling for age, gender and race
p
Devices and Secondary Complications
Severe Fatigue
Wheel chair (v. none)
0.0186
50% or less
1.99 (1.12-3.52)
51% or more
0.79 (0.44-3.52)
People (v. no)
Yes
p
0.4057
1.31 (0.69-2.48)
Cane (v. none)
Unilateral (1)
2.49 (1.52-4.08)
Bilateral (2)
1.78 (0.58-5.43)
Long leg brace (v. none)
0.0014
0.2323
Unilateral (1)
1.56 (0.63-3.90)
Bilateral (2)
0.37 (0.09-1.56)
Conclusions
• Among ambulatory persons with SCI, increased
pain intensity, pain interference, and fatigue is
seen among those with minimal wheelchair users
(1-50%) as well as those who reported use of
assistive devices that provide less support during
ambulation.
Pain and Fatigue as Mediators of the
Relationship between Mobility Aid
Usage and Depressive
Symptomatology
Dipiro, N. D., Saunders, L. L., Brotherton, S., Kraft, S., & Krause, J. S.
(2014). Pain and fatigue as mediators of the relationship between
mobility aid usage and depressive symptomatology in ambulatory
individuals with SCI. Spinal Cord, 52, 316-321.
Pain, Fatigue, Depression
• Purpose: To test a mediational model where pain
(intensity and interference) and fatigue mediate
the relationship between use of mobility aids and
moderate to severe depressive symptomatology.
• Primary Outcomes:
o Patient Health Questionnaire-9 (PHQ-9) scores of 10+
were used to indicate moderate to severe depressive
symptomatology.
Pain, Fatigue, Depression
• Predictor Variables
o Injury level (C1-C4, C5-C8, Non-cervical)
o Race (white, non-white)
o Gender (male, female)
o Age & time post-injury
o Assistive devices (cane, crutch, leg brace, walker, people)
o Wheelchair usage (<50%, 50%, 50-99%, always)
o Pain intensity (BPI)
o Pain interference (BPI)
o Fatigue (Modified Fatigue Impact Scale)
Pain, Fatigue, Depression
Model 1*
Model 2*
2.63 (1.32-5.23)
1.26 (0.52-3.07)
~50%
2.30 (0.96-5.51)
1.38 (0.48-4.02)
More than 50% but not always
1.07 (0.56-2.06)
1.64 (0.75-3.60)
Always
0.29 (0.13-0.63)
0.55 (0.22-1.38)
People (v. no)
Yes
Wheelchair usage (v. <50%)
Pain intensity (v. mild)
Moderate
1.42 (0.74-2.70)
Severe
3.32 (1.35-8.19)
Pain interference (v. mild)
Moderate
Severe
4.65 (2.42-8.94)
10.22 (4.35-24.04)
Fatigue (vs. non-disabling)
Disabling
*controlling for injury level, race, gender, age, time post-injury
7.44 (3.38-16.37)
Conclusions
• Only use of people for ambulation and using a wheelchair
less than 50% of the time were related to depression
symptoms. Other devices were not significantly
associated with depressive symptoms.
• The use of people to assist in ambulation is associated
with greater odds of moderate-to-severe depressive
symptomatology, while alwaysusing a wheelchair is
associated with lower odds.
• Pain and fatigue mediate the relationship between usage
of those assistive devices and depressive symptomatology.
Fall-related Injuries
Saunders, L.L., DiPiro, N., Krause, J.S., Brotherton, S., & Kraft, S.
(2013). Risk of fall related injuries among ambulatory participants
with spinal cord injury. Topics in Spinal Cord Injury Rehabilitation,
19(4), 259-266.
Fall-related Injuries
• Purpose: To assess the relationships between
walking devices and health behaviors with fallrelated injuries (FRI) among persons with SCI who
are ambulatory.
• Primary outcome: FRI in the past year
o “In the past year, how many falls have you had that
resulted in an injury serious enough to receive medical
care in a clinic, emergency room, or hospital?”
• Dichotomized as Yes/No
Fall-related Injuries
• Predictor variables:
o Maximum walking distance
o % time spent walking at home
o % time spent walking in community
o Walk slower compared to people without disability
o Poorer balance compared to people without disability
o Assistive devices (people, walker, cane/crutch/braces)
o Exercise
o Alcohol use
o Pain medication misuses
Fall-related Injuries
• 20.3% reported at least 1 FRI in the past year
• Among those reporting FRI
o 56.3% reported 1
o 20.8% reported 2
o 8.3% reported 3
o 14.6% reported 4+
Fall-related Injuries
Odds Ratio (95% CI)*
People (vs. no)
Yes
0.0770
2.22 (0.92-5.39)
% time walking at home (vs.
walk more than wheel)
0.0004
½ and ½
2.39 (0.95-6.06)
Wheel more than walk
0.26 (0.11-0.61)
Poorer balance (vs. no)
Yes
0.0017
2.41 (1.33-4.38)
Exercise (vs. Same/More)
0.0044
Much less/Less
2.77 (1.51-5.09)
Don’t know
1.62 (0.76-3.46)
Pain medication misuse (vs. no)
Yes
*controlling for demographics
p-value
0.0071
2.53 (1.29-4.97)
Fall-related Injuries
• Health care providers should be aware of the risk
for FRI among those who are ambulatory.
• Not only should ambulatory ability be taken into
account but also health behaviors, including pain
medication use.
Conclusions
• These analyses demonstrated there are groups of
people, among those who are ambulatory with SCI,
who are at increased risk for secondary conditions.
• This was especially seen among persons who
reported using a wheelchair, but used it less than half
of the time.
• Clinicians should be aware of the risks of secondary
health conditions among persons with SCI who are
ambulatory.
• We found increased risks also among those who
frequently use prescription medications for pain
and/or spasticity.
Future Research
• Assess changes in ambulation status and the
relationship of those changes with secondary
health conditions.
• As we saw increased risks among those who used
wheelchairs, but used them minimally, we should
assess transition from ambulation to wheelchair
use.
• Look at broader outcomes, including QOL and
participation.
Contact Us
• Lee Saunders: saundel@musc.edu
• Website: http://www.longevityafterinjury.com