the OSU EVD Presentation
advertisement
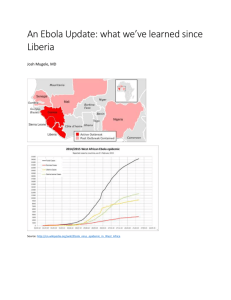
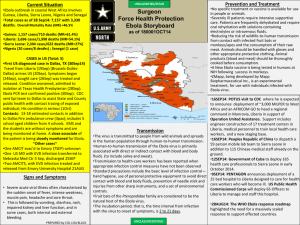
Ebola Viral Disease October 21, 2014 Overview Historical perspective Current epidemic update OSUWMC preparedness Signage and marketing Screening Isolation activation Inpatient management Staff education and training; simulations Challenges Challenges Balancing preparedness and informative education with alarmism Forced isolation/treatment Global presence of our university community Dynamic nature of the epidemic Changing protocols Other problems to not forget…. Enterovirus D68, Influenza Ebola Epidemiology Acute infection starts as a non-specific febrile illness Fever (>100.4), severe headache, muscle pain, malaise; progression to include GI symptoms (diarrhea and vomiting) Symptoms may appear 2-21 days after exposure 8-10 day window the most common Significant dehydration and electrolyte disturbances Small vessel involvement Increased permeability due to cellular damage Multi-organ system failure Hemorrhage may develop in the second week Poor prognosis associated with shock, encephalopathy, extensive hemorrhage Jay Varkey, MD; Emory University Hospital Ebola Historical Perspective Family Filoviridae Two genera: marburgvirus and ebolavirus Enveloped RNA virus Five subtypes of Ebola virus Zaire (EBOV) Sudan (SUDV) Tai Forest (TAFV) Bundibugyo (BDBV) Reston (RESTV) No vaccines/treatments approved for humans Case-fatality rates of up to 90% in African settings Jay Varkey, MD; Emory University Hospital Ebola Historical Perspective 1976: Simultaneous outbreaks in Zaire (now DRC) & Sudan Zaire: 318 cases and 280 deaths (88% mortality) Sudan: 284 cases and 151 deaths (53% mortality) 1976 & 1979: Small-to-midsize outbreaks Central Africa 1995: Large outbreak in Kikwit (DRC) 315 cases (81% mortality) Since 2000: Near-yearly outbreaks in Gabon, DRC or Republic of Congo 2000-2001: Largest outbreak on record (Sudan) 425 cases (53% mortality) Jay Varkey, MD; Emory University Hospital Current EVD Epidemic West African outbreak limited to: Guinea: 1519 cases / 862 deaths Liberia: 4249 cases / 2484 deaths Sierra Leone: 3410 cases / 1200 deaths Total: 9178 cases / 4546 deaths Senegal (8/29/14) and Nigeria (9/5/14) no longer considered at risk Early August 2014 – first health care workers brought from West Africa to Emory University Hospital Other individuals brought from West Africa since then September 30, 2014 – first case diagnosed in the US (Dallas) of a Liberian man traveling to the US Patient passed away October 8, 2014 www.cdc.gov and Fox News Current EVD Epidemic Two nurses at Dallas hospital have tested positive for Ebola (October 10th and October 14th) Second nurse traveled through NE Ohio from 10/1010/13 Over 100 people in NE Ohio on quarantine/isolation or monitoring of temperatures Risk points of when a health care worker can most commonly become infected: From exposure to body fluids during patient care From error during doffing of PPE From time when patient is intubated or during certain procedures due to increased aerosolization of secretions www.cdc.gov and Fox News EVD Preparedness at OSUWMC Both UH and UHE ED’s need to be prepared for walk-ins and EMS traffic Volunteer team designated for inpatient care Medical Team Nursing RT/team Six hours of training in three two-hour phases “Buddy System” for PPE Point of Care testing equipment for in-room use for routine labs EVS, solid and liquid waste plans developed EVD Preparedness at OSUWMC All patients planned to be admitted to 5 Ross – this may change after mid-December when old James available Will have a donning/doffing room adjacent to each room Entry restricted to assigned care team with log 2 nurses per patient – one inside/one outside If critically ill, consider two inside/one outside Team huddle including Critical Event Officer and senior clinical leaders two times per day No transport outside room unless approved by the Critical Event Officer All deviations to SOP’s need to be approved by Critical Event Officer prior to implementation EVD Preparedness at OSUWMC Collaboration between the CMO’s of Franklin County Hospitals, Columbus Public Health and COTS Outreach to regional hospital leadership and MedCare ambulance service “Secret shopper” simulations Three+ have been completed Screening questions in outpatient IHIS workflows with BPA that fires if screen positive to alert rest of care team Working closely with University officials on how this will affect the rest of campus Challenges Balancing preparedness and informative education with alarmism Forced isolation/treatment Global presence of our university community Dynamic nature of the epidemic Changing protocols Other problems to not forget…. Enterovirus D68, Influenza Special thanks to Drs. Naeem Ali, Julie Mangino, and Christina Liscynesky for resources and data