orb cl disorders
advertisement

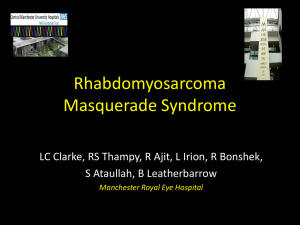
Diseases of the orbitcategories of orbital diseases, clinical presentation & evaluation Orbital cellulitis & Blow-out fracture of the orbit Dr. Ayesha Abdullah 13.09.2012 LEARNING OBJECTIVES By the end of this lecture the students would be able to; 1. Categorize orbital diseases, correlate the common symptoms & signs of orbital diseases with the underlying structural and functional disorder 2. Outline the protocol for the clinical evaluation of a patient presenting with orbital disorder 3. Differentiate between preseptal and true orbital cellulitis & explain why it is considered to be an ocular emergency 4. Describe the causes, clinical presentation, complications & line of management of orbital cellulitis 5. Explain the mechanism of BOF of the orbit, describe its clinical presentation, complications & outline the management. REVIEW (mark as true/false) • Structures that enter the orbit through the annulus of Zinn include: T • a. the nasociliary nerve F • b. the lacrimal nerve F • c. the frontal nerve F • d. the trochlear nerve T • e. the abducent nerve The following are true about the orbit: F • it has a volume of about 300 ml • the nasal bone forms part of the F medial orbital wall • the palatine forms part of the floor T • the lateral wall is the thickest orbital T wall • the lesser wing of sphenoid forms F part of the lateral wall The orbital septum • Spreads like a sheet at the back of the orbit • Separates the lids from the intraorbital contents • If weak the intraorbital fat can herinate through it • Is a weak barrier to the spread of infection inside the orbit • Is attached to the trochlea F T T F F CLASSIFICATION OF ORBITAL DISEASES 1. Congenital anomalies 2. Infections; orbital cellulitis 3. Inflammations; thyroid ophthalmopathy, orbital inflammatory syndrome ( pseudotumour) 4. Tumours; primary , secondary 5. Vascular malformations; Carotid-Cavernous Fistula (CCF), orbital varices 6. Traumatic disorders; blow-out fracture Congenital abnormalities A defect in the roof of the orbit Infections Inflammations Tumours / neoplastic disorder Vascular malformations Traumatic disorders COMMON SYMPTOMS & SIGNS OF ORBITAL DISEASES • Symptoms – Pain; orbital/ periorbital/ with ocular movements – Visual disturbances, loss/ blurring/ – Diplopia/ squint – Swelling of the eyelids/ periorbital area/ mass – Protrusion of the eyeball • Signs • Related to the eyeball – Proptosis; forward displacement of the eyeball – Dystopia; horizontal/vertical displacement of the eyeball in the coronal plane which may/ may not coexist with the forward displacement – Enophthalmos ; recession of the globe into the orbit – Nanophthalmos ; a very small eyeball Proptosis & dystopia Vertical dystopia Proptosis Horizontal dystopia Proptosis, diplopia, enophthalmos • Conjunctival & lid signs; swelling of the lid, conjunctival chemosis, injection ( redness) • Ocular motility disturbances; restrictive or muscle entrapment disorders, neurological disorders- strabismus • Corneal signs; secondary to exposure of the cornea • Posterior segment signs; venous dilatation & tortuosity , vascular occlusions, optic disc (OD) swelling, optic atrophy, choroidal folds Conjunctival, lid & ocular motility signs Fracture Fracture of floor floorof ofthe the orbit orbit The eye can’t move up, why? Patch of anesthesia • Other signs; bruit (carotid-cavernous fistula/CCF), pulsations (CCF, orbital roof defects), palpable mass • Sight threatening signs are exposure keratopathy, pupillary abnormalities ( RAPD) & optic disc or vascular changes in the retina • Common causes of proptosis in adults – Thyroid eye disease – Tumours • Common causes of proptosis in children – Orbital cellulitis – Tumours – Congenital malformations of the orbital bones What is this? Clinical evaluation of orbital disorders • History • Examination – Assessment of visual functions; Visual acuity & colour vision – Examination of the anterior segment – Examination of the pupils – Examination of the posterior segment – Examination of the Extra Ocular Muscles – Intraocular pressure measurements • Special tests – Exophthalmometry ( measuring globe protrusion & displacement – proptosis, dystopia) – Local palpation – Bruit & pulsations – Checking for cranial nerve dysfunctions – (II, III, IV, V, VI, VII,VIII) Clinical test; measuring proptosis Hertel Exophthalmometer Exophthalmometery Looking for proptosis/enophthalmos over the patient’s head • IMAGING – Ultrasonography (US) – CT scan – MRI – Plain radiographs ( Caldwell & Waters view)- mostly taken over by CT & MRI Summary ? Case #1 A one-year old baby presented to the OPD of the department of Ophthalmology with the complaint of a red swollen left lower lid for the last two days. On examination the lid was red, warm & mildly tender to touch. His vision was normal, the eye had mild conjunctival redness, pupils were normal and the ocular movements were also normal. Watch the photograph…. Some questions 1. What kind of orbital condition is this? 2. What structures are affected? 3. What more information should we ask for to? 4. What possible causes can you think of? 5. Is the condition confined to the lids or has it involved the eyeball? 6. Why do you think so? 7. Would you like to have more information? Some more information……… • The child had a history of insect bite on the lid two days ago, the swelling increased thereafter. The insect bite mark was visible • There was no history of trauma or symptoms suggestive of flu or URTI • His temperature was normal Some more questions • What should be the management, keeping in mind the nature of the problem? • What could be the complications of such a case? • Is there any role of health education in this case? Don’t’ forget simple things can get complicated • Let us see an other case…….. Case #2 • A 12 year old child was brought to the OPD of the department of ophthalmology with a history of red swollen left upper lid for the last 5 days. He also had fever for the last two days along with headache. On examination the child had a grossly swollen lid. His visual acuity was 6/18 OD & 6/6 OS. The lid was warm and tender. The eye was moderately proptosed with conjunctival chemosis. The pupil was slow to react to light and the ocular movements were painful & limited. The temperature was 1010 F & the child generally looked unwell…….. Ocular signs Some questions…. 1. What kind of orbital condition is this? 2. What structures are affected? 3. What more information should we ask for to get an idea about the cause of the problem? 4. Is the condition confined to the lids or has it involved the eyeball? 5. Why do you think so? 6. What possible causes can you think of? 7. Would you like to have more information? Some more information……. • The child had a history of recurrent flu and upper respiratory tract infections. He had history of blocked nose and thick greenish nasal discharge was noted on examination. • The child was put on intravenous antibiotics but didn’t get better • A subsequent CT scan was done which showed……. The antibiotics were changed to intravenous ampicillin/sulbactam and after 5 days were changed to oral amoxicillin/clavulanic acid for a total of 14 days of antibiotics. Orbital abscess Some more questions • What should be the management, keeping in mind the nature of the problem? • What do you think can be done with the abscess? • Is there any role of health education in this case? Conclusion about the two cases • What is the difference between the two cases? • We consider the second case an ocular emergency, why? • How did the subperiosteal abscess form in the second case? • What other complications could happen in the second case? Ocular/intracranial/orbital • What could be included in the differential diagnosis?.... Differential diagnosis of red swollen lids 1. 2. 3. 4. Prespetal cellulitis Orbital cellulitis Contact dermatitis Focal lesions like stye, chalazion ( especially if infected) 5. Allergic reaction ( angioedema) 6. Tumours ( specifically Rhabdomyosarcoma in children & malignant lid tumours, primary or secondary in adults) Management Preseptal cellulitis 1. Symptomatic; analgesics & NSAIDS 2. Specific: 3. For mild infection oral antibiotics with antihistamines in case of dual pathology like in insect bite 4. Very severe infections may require intravenous penicillins to avoid true orbital cellulitis 5. Lid abscesses should be drained 6. Third generation cephalosporins in penicillin allergy 7. In general practice it requires oral antibiotics and referral to an ophthalmologist especially when more severe and in children Management Orbital Cellulitis • • • • Admit Requires care by an ophthalmologist Symptomatic; antipyretic, NSAIDS Specific ; hospitalization & antibiotic therapy – – – – Braod spectrum antibiotic (I/V); Ceftazidime or cefotaxime Ampicillin for H Influenzae infection Cloxacillin for Staphylococcus aureus infection Metronidazole 500mg tds, PO when anaerobic infection is suspected especially in adults – Vancomycin in case of allergy to the above mentioned Management Orbital Cellulitis • Surgical intervention in case of local abscess or unresponsive cases • Consultation with ENT specialist, neurosurgeon & paediatrician if required Let us summarize • Preseptal orbital cellulitis & orbital cellulitis are both infections. • It is more common in children • The route of infection could be from the nearby infectious focus like infected sinuses, skin wound or spread of infection via blood • The most common cause especially in children is ethmoidal sinusitis • • Both preseptal and orbital cellulitis may have: – Fever – Eyelid edema – Pain – Red eye – Child is ill-appearing • Orbital cellulitis signifies spread of inflammation to the posterior orbital contents that is the eyeball, extraocular muscles: helpful signs to distinguish it are:– Proptosis – Decreased visual acuity ( may be normal in the beginning) – Red eye with conjunctival chemosis of moderate to intense congestion – Painful limited eye movements – Afferent pupillary defect Why is OC an emergency • Prior to the availability of antibiotics, patients with orbital cellulitis had a mortality rate of 17%, and 20% of survivors were blind in the affected eye. However, with prompt diagnosis and appropriate use of antibiotics, this rate has been reduced significantly • blindness can still occur in up to 11% of cases. Orbital cellulitis due to methicillin-resistant Staphylococcus aureus can lead to blindness despite antibiotic treatment. • The infection can spread to the meninges and brain & may cause death • That is why it is an emergency Ocular & orbital complications of OC • Corneal scarring from exposure Extraocular muscle palsies Optic nerve damage • Central retinal artery and central retinal vein occlusion • Orbital abscess • Visual loss and blindness Extraocular complications of OC • • • • Brain abscess Meningitis Cavernous sinus thrombosis Osteomyelitis of skull and orbit bones Cavernous sinus thrombosis Brain abscess References • Orbit, eyelids & lacrimal system. American Academy of Ophthalmology; 1997-98 • Jack J Kanski. Clinical ophthalmology a systematic approach. 5th ed;2003:557-89 • Parsons’ diseases of the eye. Diseases of the adnexa-diseases of the orbit. 19th ed. 2004; 505-524 • Newell F W. The orbit. In Ophthalmology principles & concepts.7th ed; 1992:259-69 WEB RESOURCES • http://www.emedicine.com/oph/topic75 8.htm. • http://www.emedicine.com/oph/orbit/e xophthalmos • http://www.ccmcresidents.com/wpcontent/uploads/2011/08/242.full_.pdf