Vomiting
Bloody diarrhea
Failure to thrive
Hypotension
Shock
Soy
Cow’s Milk
Enterocolitis after
ingestion of a specific
food protein.
Main symptoms
Diarrhea – blood (+)
Vomiting
Hypotension/shock
Failure to thrive
FPIES stools (Kabuki, Allergol Int 2007)
Symptoms resolve with removal of allergen from diet.
Usually presents in neonates and infants, “outgrown” by 3 years.
Sicherer, J Pediatr 1998
Am J Med Sci 1940
Onset
Symptoms
Stools with mucus and frank
3 weeks
blood
4 weeks
Intervention
Cow milk to breast
milk
Mucusy bloody stools, sometimes
Cow milk to goat milk
just blood without feces
Frankly bloody stools “sufficient
5 weeks to wet a large part of each
diaper”, anemia, colic
Mucusy bloody stools, vomiting
5 weeks
(lethargic episodes/aspiration)
Outcome
Resolution in 48h,
recurrence when milk
tried again
Resolution in 48h
Cow milk to breast
milk (almost had exlap for Meckel’s)
Resolution in 48h
Cow milk to goat milk
Resolution in 48h,
recurrence at 7 wks,
switched to soy
Joyce D. Gryboski, MD
Infant with 3 episodes of bloody
diarrhea and shock within 1-2h when
challenged with milk
Rapid resolution of symptoms off
of milk
Diagnosis: “milk induced colitis”
21 cases characterized by GI sx (vomiting, diarrhea, usually
mucusy/bloody stools) and poor weight gain that resolved with
elimination of cow’s milk
33% developed signs of shock when challenged
Colon bx (before and after milk elimination) demonstrated rapid
reversal of colitis after milk eliminated – proposed that “milk
induced colitis” be recognized as a distinct entity
2 cases: 32 weeker (1.6 Kg) and a term (2 Kg) infant
Both treated for NEC, thriving on hydrolysate formula, and then had
acute onset recurrence of NEC-like sx when given standard formula
(hypothermia/shock, increased ANC, vomiting, distension,
bloody diarrhea).
Without referencing previous articles, reported that “intolerance to
whole milk protein can cause a syndrome similar to NEC.”
Collected 9 more cases and proposed diagnostic criteria for
“Milk- and soy-induced enterocolitis of infancy.”
Mean age of symptom onset: 11 days - all with FTT, dehydration,
bloody diarrhea
8/9 affected by both milk and soy
Patients rehydrated, some had sepsis workups (all negative);
symptoms resolved on EHF, asked to come back for
challenges with milk and soy (mean age 5.5 months)
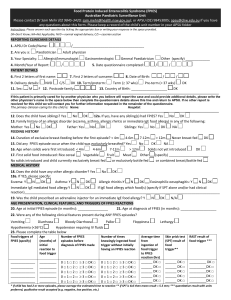
Prior to challenge:
Must be gaining weight with normal stools for at least 2 weeks
NPO for 8 hours
Baseline CBC with diff
All stools 12 hours prior to challenge checked for blood, leukocytes,
and reducing substances
Fed 100 ml of milk or soy formula ….
After the challenge:
Directly observed by physician for 2 hours in case of anaphylaxis, VS
monitored for 8 hours, symptoms monitored for 48h
CBC with diff at +2, 4, 6, 8, 10, 24 hours
Stools for next 48 hours checked for blood, leukocytes, and reducing
substances
Positive challenges in
14/18 (new onset diarrhea
with blood and leukocytes
within 24h)
Vomiting onset 1-2.5h
(4/16 challenges with no
vomiting)
Diarrhea onset 2-10h
(most <6h), some grossly
bloody
Duration of diarrhea
8-72h (most <24h)
No infants with
angioedema, urticaria,
wheezing (i.e.,
type I IgE-mediated allergic
reactions)
Average change in ANC after oral challenge
positive challenges
negative challenges
Powell’s diagnostic criteria for milk- and soy-induced
enterocolitis of infancy:
1.
Sx onset <2 months of age, <9 months at time of work-up
2.
When receiving formula with the offending protein, infant has
watery stools with blood and leukocytes that resolves when
that protein is eliminated
3.
Challenge causes diarrhea with blood and leukocytes within
24 hours
4.
ANC at 6-8h after challenge is increased by >3500/mm3 over
baseline
Cow’s milk protein and soy are most common in US studies
50% of patients reactive to milk also react to soy.
Solid foods:
Peas, lentils, peanuts
Chicken, turkey, fish (fish-PIES?)
Rice, oat, barley
Squash, sweet potatoes
Fruits (apple, pear, banana, peach)
Most with FPIES triggered by a solid food also have history
of reacting to milk and/or soy.
Food allergy – adverse
immune response to a food
IgE dependent:
Oral allergy syndrome,
GI anaphylaxis
IgE associated/cellmediated:
Eosinophilic esophagitis/
gastritis/enteritis/colitis, AD
Cell-mediated:
FPIES (Dietary protein
enterocolitis), dietary protein
proctitis
Sicherer, Sampson, JACI Primer 2010
To quote every article: “Not well understood”
Clinical observation
Possible conclusions
Resolves with EHF or
amino acid formula
Triggered by food protein antigens
Does NOT occur to
exclusively breast-fed
infants
Quantity of food antigen in human milk not
adequate to elicit a clinical response?
In exclusively breast-fed
infants, occurs when
solids are added to diet
The quantity of solid food protein overwhelms
protective effect of breast milk?
Human milk contains factors that promote
tolerance?
Clinical observation
Possible conclusions
Most patients with solid
FPIES are already on EHF
Immaturity of gut’s food protein tolerance
mechanisms plays major role
Rarely develop FPIES to
new foods >1 year old
Almost all outgrow FPIES
by 3 years old
SPT/sIgE negative; sx not
consistent with type-1
hypersensitivity
Likely not IgE-mediated
In infants with “gastrointestinal milk allergy”*…
…their peripheral mononuclear cells secrete higher
levels of TNF- which increases intestinal permeability
(Heyman, Gastroenterology 1994)
…there is elevated TNF- in stools after challenge
(Majaama, Clin Exp All 1996)
*may or may not be FPIES
Case report: 8 mo male with rice FPIES (Mori, Clin Dev Imm 09)
Measured IL-4, IFN-γ, IL-10 expression by peripheral blood T-cells
pre/post a positive challenge (at 8 mo) and negative challenge (at 14 mo)
4 hours after positive challenge: vomiting, diarrhea, lethargy requiring
IVF resuscitation.
Pre
Post
+
Neg
14 mo
8 mo
Duodenal biopsy of 28 infants (mean 49 days) with active cow’s milk
FPIES (Chung, JACI 02)
Dx confirmed by challenge; compared to 10 controls
Specimen stained for:
Relevance
Result
TNF-α
Inflammatory cytokine,
5GI permeability
Markedly 5 in FPIES (pos.
corr. with villous atrophy);
absent in controls
TGF-β1
6T-cell inflammation (via
Treg?); 5 with gut maturation,
secreted in breast milk
Low in FPIES & control
TGF-β RI
High affinity receptors for
TGF-β1
Low in most FPIES vs.
control (& neg. corr. with
villous atrophy)
TGF-β RII
No difference between
FPIES and control
Eosinophilic Inflammation Is Prominent In FPIES –
Multi-center Case-series Study (Nomura, JACI Abstract 2009)
Included 114 patients (inclusion criteria did not require challenge)
Peripheral blood eosinophils >20% in 50% of patients
Stool eos in 69%
Elevation of Fecal Eosinophil-Derived Neurotoxin in FPIES
(Nomura, JACI Abstract 2010)
Included 38 controls vs. 6 FPIES (inclusion criteria did not require
challenge)
1.4% of controls with EDN > 20 ng/g; 83% of FPIES (with clinical
sx present) had EDN > 20 ng/g
Mature gut
Immature gut
Tregs, IL-10
IL-4 (TH2)
IFN-γ (TH1)
Cytotoxic
T-cells, ?Eos
TGF-β1 and
receptors
TNF-α
Tolerance
FPIES
Toxic appearing infant with
poor perfusion and bloody
diarrhea….
Sepsis, NEC
Surgical emergency
Infection: NEC, bacterial enterocolitis (SSYCE), rotavirus
Anatomic: volvulus, Meckel’s, AVM, intussusception, anal fissure
Hematologic: coagulopathy, HDN
Allergic: eosinophilic gastroenteropathies, food protein-induced
proctocolitis, GI anaphylaxis
Misc: swallowed maternal blood
Index of suspicion of typical cow’s milk protein-induced
enterocolitis (Hwang, J Korean Med Sci 2007)
142
consecutive infants
15-45 days old
admitted for
vomiting/diarrhea
71%
11%
17%
Infection
FPIES (cow’s milk)
Other
Infection: NEC, bacterial enterocolitis (SSYCE), rotavirus
Anatomic: volvulus, Meckel’s, AVM, intussusception, anal fissure
Hematologic: coagulopathy, HDN
Allergic: eosinophilic gastroenteropathies, food protein-induced
proctocolitis, GI anaphylaxis
Misc: swallowed maternal blood
Index of suspicion of typical cow’s milk protein-induced
enterocolitis (Hwang, J Korean Med Sci 2007)
Failure to thrive
Eosinophil count (serum)
WBC count (serum)
Metabolic acidosis
Platelets
Methemoglobinemia
Albumin
Fecal blood or
leukocytes
Infection: NEC, bacterial enterocolitis (SSYCE), rotavirus
Anatomic: volvulus, Meckel’s, AVM, intussusception, anal fissure
Hematologic: coagulopathy, HDN
Allergic: eosinophilic gastroenteropathies, food protein-induced
proctocolitis, GI anaphylaxis
Misc: swallowed maternal blood
Index of suspicion of typical cow’s milk protein-induced
enterocolitis (Hwang et al, J Korean Med Sci 2007)
Failure to thrive
Albumin
Infection: NEC, bacterial enterocolitis (SSYCE), rotavirus
Anatomic: volvulus, Meckel’s, AVM, intussusception, anal fissure
Hematologic: coagulopathy, HDN
Allergic: eosinophilic gastroenteropathies, food protein-induced
proctocolitis, GI anaphylaxis
Misc: swallowed maternal blood
Do not laparotomize FPIES (Jayasooriya, Ped Emer Care 2007)
“A case of food protein-induced enterocolitis syndrome,
leading to unnecessary surgery, is presented.”
FPIES: 16-Year Experience (Mehr, Pediatrics 2009)
Australian retrospective case series of 35 children with FPIES (66 total
episodes); age at presentation 5.5 ± 2.4 months
71% of children with ≥2 episodes before diagnosis (20% with 4 episodes)
1 child with laparotomy
2
19
FPIES
5
Initial episodes
presenting to ED
“food allergy”
4
4
4
2
Discharge diagnoses
sepsis
gastroenteritis
intussusception
no dx
Clinical differentiation of allergic GI disorders of infancy from FPIES
Disorder
Key features
Distinction from FPIES
GI anaphylaxis
(Type-1 immediate
hypersensitivity)
Acute vomiting, diarrhea,
angioedema, urticaria,
wheezing, hypotension
Cutaneous/respiratory
involvement, SPT/specific IgE
positive
Eosinophilic
Gastroenteropathies
Depends on site of
eosinophilic inflammation in
GI tract: vomiting,
obstruction, gastric or
colonic bleeding, diarrhea,
FTT
Gradual onset of sx after
ingestion, gradual
improvement after elimination
(weeks); many with positive
SPT/specific IgE
Food protein-induced
proctocolitis
Blood streaked stools,
eosinophilia in colon bx
No vomiting or systemic sx,
usually breast-fed, thriving
Sicherer, JACI 2005
Not IgE-mediated so skin prick testing and specific
IgE is typically negative.
Thorough history!
Infant with 5 ICU admissions, each after ingestion of cereal added to
formula (Wegrzyn, Pediatrics 2003)
FTT, low albumin, plt >500k, temp <36 °C identified as most unique
presenting features in case series (Mehr, Hwang)
Powell’s criteria - inpatient oral food challenge with IV access,
physician supervision.
Dose for challenge is arbitrary; 0.15 to 0.6 g protein per Kg reported
Gastric Juice Analysis in Cow’s Milk ProteinInduced Enterocolitis (Hwang, J Korean Med Sci 2008)
Challenged 17 consecutive patients to confirm diagnosis of
FPIES to cow’s milk; 16 with positive challenge (needed IVF)
Gastric juice analyzed at 3 hours post challenge: >10 WBC per
HPF in 15/16 patients with FPIES.
Spergel, AAAAI 2010
Atopy patch test for the diagnosis of FPIES
(Fogg/Spergel et al, Ped All Imm 2006)
19 infants with suspected FPIES
(some with reactions to multiple foods)
Patch tested with suspected foods
(off at 48h, read at 72h)
Within 2 weeks orally challenged with
suspected foods
APT predicted results of OFC in 27/32 cases
(Sens 100%, Spec 71%, PPV 75%, NPV 100%)
Will APT revert to negative when they outgrow
FPIES?
Food Allergy Testing: Atopy Patch Test
(Spergel, AAAAI meeting 2010)
Discussed 20 patients with FPIES (all with negative SPT),
patch tested prior to OFC
5/5 with negative APT had negative OFC
12/15 with positive APT had positive OFC
Sens 80%, Spec 100%, PPV 100%, NPV 62.5%
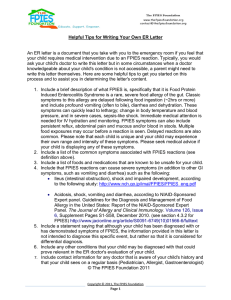
Note: these
recommendations
are based on
expert opinion.
If presenting for the first time with signs of shock – thou shalt
perform an extensive evaluation to rule out other causes
(e.g. r/o sepsis)
If accidental ingestion occurs in a child with FPIES, take
child to ED for observation, have a letter with instructions
from the allergist to the ED physician.
15-40% may be hypotensive and require IV fluid
resuscitation, ±corticosteroids (to suppress cellmediated inflammation)
No known role for antihistamines, anti-IgE, epinephrine
Sicherer, JACI 2005
FPIES rarely presents vs. new foods after 1 year old
During 1st year:
If cow’s milk FPIES –
switch to EHF, then AA
formula if still symptomatic
(skip soy formula), delay
introduction of solids.
Milk
FPIES
50% vs. soy
33% vs. solids
If solid FPIES – switch to EHF/AA
formula, eliminate grains, legumes,
poultry, ?fish.
Solid
FPIES
80% vs. >1 food
65% vs. milk/soy
50% vs. another grain
After 1st year – inpatient challenges with culprit food 12-18 months
after last reaction; observed challenges with untried foods.
Sicherer, JACI 2005
For the IM trained A/I fellows:
Extensively hydrolyzed (casein) formulas:
Alimentum
Nutramigen
Pregestemil*
Elemental (amino acid) formulas:
Neocate
Elecare
Nutramigen AA
*Contains short/medium chain fatty acids for special cases: short bowel, liver disease, etc
Prospective follow-up of oral food challenge in FPIES
(Hwang, Arch Dis Child 2009)
23 infants with cow’s milk FPIES, diagnosed via OFC at mean age of 36
days, randomized into 2 groups:
Cow’s milk challenge:
11
8
4
(6 mo)
(10 mo)
3
0
(14-16
mo)
(18-20
mo)
Soy milk challenge:
12
3
1
(6 mo)
(10 mo)
0
(14-16
mo)
Based on these findings, authors recommend soy OFC at 6-8 months and
cow’s milk OFC at 12 months (when most will have negative challenge)
Food
Resolution Rate
Study
Milk
60% by 3 yo
Sicherer 1998
64% by 10 mo
(100% by 20 mo)
Hwang 2009
55% by 32 mo
Seppo 2010
83% by 3 yo
Mehr 2009
20% by 3 yo
Sicherer 1998
27% by 3 yo
Nowak-Wegrzyn 2003
67% by 3 yo
Fogg 2006
92% by 10 mo
(100% by 14 mo)
Hwang 2009
28% by 34 mo
Seppo 2010
80% by 3 yo
Mehr 2009
40% by 3 yo
Nowak-Wegrzyn 2003
50% by 42 mo
Seppo 2010
58% by 45 mo
Seppo 2010
Soy
Rice
Oat
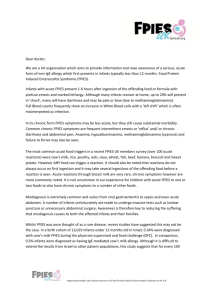
The Incidence, Manifestations And Natural Course Of
(Cow’s Milk) FPIES (Katz, JACI abstract 2010)
Medical center in Israel: 98.4% of all newborns born over 2 years
successfully contacted (n=13,019)
2.9% with suspicion of cow’s milk intolerance
0.33% determined to have FPIES (25/44 confirmed by OFC). 95%
tolerated CM by age 3.
Index of suspicion of typical cow’s milk protein-induced
enterocolitis (Hwang, J Korean Med Sci 2007)
142 consecutive infants 15-45 days (not exclusively breast
fed)admitted for vomiting and/or diarrhea over 3 years.
11.3% (n=16) with FPIES (all confirmed by OFC)
Clinical Characteristics of Children with Food
Protein-Induced Enterocolitis (Seppo, JACI abstract
2010)
Mt. Sinai Medical Center, NYC
“We analyzed records of children with FPIES evaluated in
the Allergy Clinics between 2001 and 2009. 76 children
with FPIES were identified.”