1 Sat_0905am_Inspiring_Continuous_Quality_Improvement_Ellner
advertisement

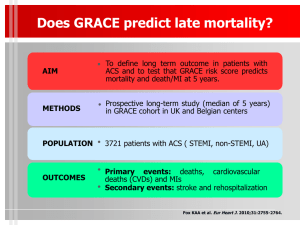
ACS NSQIP: Preventing complications Reducing costs Improving surgical care May 17, 2014 Scott Ellner, DO, MPH, FACS Saint Francis Hospital and Medical Center Disclosures No relevant disclosures related to this presentation. 2 Increasing Focus on Improving Quality While Reducing Costs Decisions are being made now – and we have opportunities to get ahead of CMS actions: • CMS readmissions penalties and valuebased purchasing • Hospital Compare and other public reporting • Physician quality reporting • General surgery registry rule 3 Which Direction will Quality Improvement Go? We’ve Found Common Ground 5 ACS NSQIP: What’s Different? Developed by surgeons Clinical, not administrative, data Risk-adjusted and case-mix adjusted National benchmarking 30-Day patient follow up Audited Trained data collector 6 Clinical Data Better for Measuring Quality 7 Risk and Case-Mix Adjustment Matters To judge care fairly and understand where problems are occurring: Health of the patient must be considered Risk of the procedure must be considered 8 Following Patients After Discharge • Half or more of all complications occur after discharge1 • Quality programs based on admin data don’t track post-discharge • Complications after discharge can lead to readmissions2 Tracking quality can’t stop at the hospital’s door 1 Ko CY. “ACS NSQIP Conference Overview.” Presentation to the 2009 ACS NSQIP National Conference. July 2009. 2 Kassin MT et al. “Risk Factors for 30-Day Hospital Readmissions among General Surgery Patients.” J Am Coll Surg. 2012; 215: 322-30. 9 ACS NSQIP: Proven to Reduce Complications, Save Lives 2009 Annals of Surgery study: Prevent 250-500 complications annually Save 12-36 lives annually Leading to reduced costs 10 Surgical Complications Drive Readmissions 2012 Journal of the American College of Surgeons study: • Surgical complications key driver of 30-day readmissions • SSIs – 22% • Gastrointestinal – 28% • Pulmonary – 8% 11 ACS NSQIP: Better Care, Lower Costs Not only will patients benefit, but hospitals see a significant return on their investment with ACS NSQIP. • Significant cost savings per year • Reduced readmissions and reduced lengths of stay translate to better patient outcomes, better satisfaction and even more cost reduction • Pays for itself by avoiding about a dozen surgical complications 12 ACS NSQIP Meets Regulatory Requirements CMS general surgery registry rule began this FY ACS NSQIP measures reported on Hospital Compare (voluntary) Five ACS NSQIP measures being considered for national adoption by CMS ACS NSQIP’s SSI harmonized with CDC’s NHSN program Joint Commission Quality Check for participation Part of SUSP program supported by AHRQ 13 ACS NSQIP Meets Regulatory Requirements CMS general surgery registry rule began this FY ACS NSQIP measures reported on Hospital Compare (voluntary) Five ACS NSQIP measures being considered for national adoption by CMS ACS NSQIP’s SSI harmonized with CDC’s NHSN program Joint Commission Quality Check for participation Part of SUSP program supported by AHRQ 14 Why the Foley? Everybody gets a catheter Post-Operative Urinary Tract Infections Observed Rate: 2.41% Expected Rate: 1.47% O/E Ratio: 1.64 Status: Needs Improvement 2008 The CAUTI Gang 32-40% of all nosocomial infections Adds an average of 1-3 additional hospital days UTIs increase a patient's hospital costs by 47 % at teaching hospitals and 35 % at community hospitals Roberts RR Clin Infect Dis , 2009 Next Steps Build a guiding coalition Drill down on data Determine why patients developed the infection Share key findings with key stakeholders Share Data Leadership Model the Way Challenge the Process Share a Vision Empowerment CAUTI Sub-Committee Goals – Time Sensitive Drill down Pilot Audit Implementation Sustainability ACS Clinical Guidelines Prior to Insertion: • Education During Insertion: • Trained personnel • Hand hygiene After Insertion: • Secured catheter • Closed Drainage • Urimeter positioning Nurse Driven Protocol Automatic Order Set Catheter Needed? Remove by Post-op Day 2 Catheter Still In? Why? Documentation Situational Leadership Nurse Driven Protocol Patients UTI Pre Intervention Post Intervention N=1,404* N=2,469* 36 2.6% 38 p 1.5% <.05 Pre-Intervention: September 2007 – December 2008 Post-Intervention: January 2009 – December 2010 *Number of patients undergoing general surgery captured in the NSQIP database. 24 C. Difficile Prevention Derkonja DM JAMAintmed 2013 Silver Prices Pickard P Lancet 2012 $160,000 savings/year Barriers 1) 2) 3) 4) Complacency Resistance Exposing failures Challenging years of embedded culture 5) Compliance 6) Training 7) Uneasy Leadership Return on Investment A Business Case for Reducing CatheterAssociated Urinary Tract Infections A Study Using ACS National Surgical Quality Improvement Program Data Return on Investment General & Vascular Surgery UTI Length of Stay (days) Excess Costs/Patient* N=74 Mean Mean Cases Identified Inpatient Comments Patient Occurrences 5 deaths 9 C. Diff (+) 41 28.5 $52,384 2 readmissions 4 ED visits Outpatient 29 33 Zimlichman E JAMAint 2013 6 $758 * Variable Costs 62% Reduction Observed Rate: 1.23% Expected Rate: 1.43% O/E Ratio: 0.86 Status: As Expected 2008 2014 Surgical Checklist Verified with ACS NSQIP Data 31 Take Home Points • ACS NSQIP metrics are actionable • Share data and acknowledge need for change • Implement a CAUTI prevention protocol • Recognize and address barriers • It’s all about leadership