1._Acute_Kidney_Injury_(AKI)
advertisement
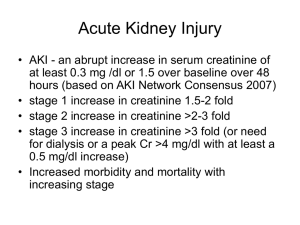
Acute kidney Injury(AKI) Dr Dana Ahmed Sharif Renal Physician MRCP UK/ MRCP London Resource materials • • • • Davidson’s Principles & Practice of Medicine Kumar & Clark Clinical Medicine Oxford textbook of Clinical Nephrology Oxford handbook of Nephrology and hypertension • Renal Association website( www.renal.org) • K/DOQI guideline (www.kidney.org) • AKI network ( www.akinet.org) Renal function • Kidney has many roles: Renal function • Kidney has many roles: - Excretory function Renal function • Kidney has many roles: - Excretory function - Osmolality regulation Renal function • Kidney has many roles: - Excretory function - Osmolality regulation - Acid base balance Renal function • Kidney has many roles: - Excretory function - Osmolality regulation - Acid base balance - BP regulation through salt and water balance Renal function • Kidney has many roles: - Excretory function - Osmolality regulation - Acid base balance - BP regulation through Salt and water balance - Hormone secretion ( Erythropoietin, Vit D3) Definition of Acute Kidney Injury Acute usually reversible decline in renal function* • Rapid time course( < 48 hrs) • Reduction of kidney function: A- Rise in serum creatinine, defined by either: 1- absolute increase in serum creatinine of >0.3mg/dl( >26µmol/l) 2- % increase in serum creatinine of > 50% B- Reduction in urine output, defined as < 0.5ml/kg/hr for more than 6 hrs * Acute kidney injury network Incidence of AKI* • 500 ppm/year – UK ( up to 38,000/yr) • Incidence of AKI needing dialysis 200 ppm/year • Pre renal and acute tubular necrosis (ATN) accounts for 75% of the cases of AKI • 7% of all hospital admissions( 65% of intensive care admission) • • • • Mortality: 5-10% in uncomplicated AKI 50-70% in AKI secondary to other organ failure( intensive care) > 50% in dialysis requiring AKI *Xue JL, Daniels F, Star RA et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol 2006; 17: 1135–1142. Acute kidney injury Pre renal - ↓ Effective renal blood flow: 1- Haemorrhage 2- Volume depletion 3- Low cardiac output 4- Sepsis 5- CCF 6- Cirrhosis - Arterial stenosis/Occlusion - Vasomotor: 1- NSAID 2- ACEI/ ARBs Intrinsic Post renal Diagnosing pre-renal AKI • Is the patient volume depleted? Diagnosing pre-renal AKI • Is the patient volume depleted? • Is cardiac function good? Diagnosing pre-renal AKI • Is the patient volume depleted? • Is cardiac function good? • Is the patient septic? Diagnosing pre-renal AKI • Is the patient volume depleted? • Is cardiac function good? • Is the patient septic? History Examination Investigation Diagnosing pre renal AKI • History • Examination : 1- Signs of Hypovolaemia: a- Low BP( and reduced pulse pressure) b- Postural BP drop ( a fall in systolic BP > 10mmHg) c- Sinus tachycardia and postural increase in heart rate ( increase in HR > 10 beat/min). d- Low JVP even when the patient is supine e- Cool peripheries and vasoconstriction f- Poor urine output Diagnosing pre-renal AKI 2- Sings of hypervolaemia( high extracellular fluid): a- Increased circulating volume: - High BP - Elevation of the JVP b- Increased interstitial fluid: - Peripheral or generalized oedema - Pulmonary oedema (tachypnoea, tachycardia, third heart sound, basal crackles) - Pleural effusion - Ascites . Lab investigation: - Blood tests - urine: including urinary Na( low) Case 1 • 67 yr man – IHD • Admitted with D&V – O/E JVP not seen, BP 100/60 lying, 80/50 standing, pulse 105 bpm • Creatinine 5.8 (0.7-1.2mg/dl) • x2 IV access • Given IV saline • Catheterised and started on furosemide • Function worsened and transferred to renal unit What was the only helpful intervention 1- Inserting a urinary catheter 2- Inserting a CVP line 3- Administering IV fluids 4- Administering diuretics What was the only helpful intervention 1- Inserting a urinary catheter 2- Inserting a CVP line 3- Administering IV fluids 4- Administering diuretics Treatment of pre renal failure • DO NOT put in a urinary catheter • DO NOT GIVE DIURETICS – improving urine volume does not mean an improvement in renal function • CVP line rarely needed – and certainly not substitute for clinical examination Treatment of pre-renal failure • Volume replacement • Improve cardiac function in congestive cardiac failure Treatment of pre-renal failure Volume replacement: fluid, blood, plasma expander… A- Resuscitate: - Hypotensive and tachycardic B- Replacement C- Maintenance Treatment of pre-renal failure Volume replacement: fluid, blood, plasma expander… A- Resuscitate: - 0.9% Normal saline - be aware of fluid overload (high BP, RR, basal lung crackles and low satO2) - fluid challenge ( trial 200-300ml N saline IV in 10min, then re-assess, repeat if necessary) B- Replacement: depends on a- Degree of hypovolaemia b- Ongoing losses c- Whether oligo-anuric d- Cardiovascular status Treatment of pre-renal failure - A rough guide ( be aware of elderly and those with poor left ventricular function): - first litre over 2 hours, THEN REASSESS - second litre over 4 hours, THEN REASSESS - third litre over 6 hours, THEN REASSESS *Remember to add insensible loss, if not sure or think you over done it, stop all fluid and reassess the patient C- Maintenance: Once euvolaemic, and assume no other losses, match urine out put plus 30mls/hour (insensible loss may be higher if febrile) Acute kidney injury Pre renal Intrinsic Vascular 1- Vasculitis 2- Thrombotic microangiopathy 3- Scleroderma renal crisis 4- Renal vein thrombosis 5- Cholesterol emboli Post renal Acute GN Acute TIN ATN Glomerluonephritis tubulointestitial nephritis acute tubular necrosis Acute kidney injury Pre renal Intrinsic Vascular 1- Vasculitis 2- Thrombotic microangiopathy 3- Scleroderma renal crisis 4- Renal vein thrombosis 5- Cholesterol emboli Post renal Acute GN Acute TIN ATN (Glomerluonephritis) (tubulointestit ial nephritis) acute tubular necrosis Ischaemic Nephrotoxic Acute kidney injury Pre renal Intrinsic Vascular 1- Vasculitis 2- Thrombotic microangiopathy 3- Scleroderma renal crisis Post renal Acute GN Acute TIN ATN (Glomerluonephritis) (tubulointestit ial nephritis) acute tubular necrosis Ischaemic Nephrotoxic 4- Renal vein thrombosis 5- Cholesterol emboli Endogenous 1- Haemoglobinuria 2- Myoglobinuria 3- Casts and Crystals Exogenous 1- Nephrotoxic drugs 2- Radiocontrast Diagnosing Intrinsic Renal AKI • Has pre-renal and post renal been excluded? • History - Drug, Rash, joints, nose bleed, haemoptysis, hearing loss, claudication, IHD, diabetes, fever or night sweat, Recent infection • Examination - Oedema, rash, mouth ulcer, hearing loss, uveitis, AF, ischaemic toe, bruits, evidence of scleroderma, prosthetic valve or stigmata of Endocarditis • Laboratory investigations - Urine including microscopy for dysmorphic RBC, Protein, Bence Jones protein, protein/creatinine ratio or 24hr protein excretion - Blood – nephritic screen – ANA, dsDNA, ANCA, antiGBM, Immunoglobulines protein electrophoresis, Rh-factor, HBV, HCV, HIV, cryoglobulins, blood film, CK, C3,C4, ASO-titre , ESR and CRP . US kidneys . Renal biopsy Criteria for distinction between prerenal and intrinsic causes of renal dysfunction Pre renal Intrinsic Urine specific gravity > 1.020 < 1.010 Urine osmolality(mOsm/Kg) > 500 < 500 Urine Na+ (mmol/l) < 20* > 40 Fractional excretion of Na+ < 1% > 1%** * Except in diuretics or dopamine ** remains low in contrast nephropathy and myoglobinuria Case 2 What did they do right? • • • • • 56 years old man Cough, haemoptysis and joint pain O/E JVP +6cm Creatinine 7.5mg/dl( 0.7-1.2) on admission IV access, started on IV fluid and diureticsSOB worsened • Transferred to renal unit after 1 week when renal function failed to improve What was done correctly 1. Omission of urine catheter 2. Administered IV fluids and diuretics 3. Transfer to renal unit after 1 week What was done correctly 1. Omission of urine catheter 2. Administered IV fluids and diuretics 3. Transfer to renal unit after 1 week Treatment of intrinsic renal AKI • GN – autoimmune – immune suppression/ plasma exchange • Infective Bacterial Endocarditis – antibiotics • Interstitial nephritis - Stop offending medication - Corticosteroids Treatment of intrinsic renal AKI • ATN - In-hospital mortality 19-37%* - Recovery could take up to 6 weeks** - Self correcting (full 60%, some 30%, dialysis 5-10%) - Very severe – permanent cortical necrosis * Oxford handbook of Nephrology and Hypertension 2009 ** Kumar and Clark/ Clinical Medicine July 2012 Acute kidney injury Pre renal Intrinsic Post renal Obstruction 1- Bladder out-let obstruction 2- Bilateral ureteral obstruction Nature of Obstruction • Outside - Tumours, prostate, retroperitoneal fibrosis, cervical Ca • Within wall - Tumours, strictures • Within lumen - Stones, tumours Diagnosing post renal AKI • History - pain, anuria, haematuria, prostatism • Examination - palpable bladder, central abdo mass, PR, PV • Observation • Laboratory investigations - Urine - Blood - Imaging – US, CT Treatment of Post renal AKI • Obtain drainage of Urine - Bladder catheter – per urethra, suprapubic - Retrograde drainage - Antegrade drainage Case 3 • • • • • • • 82 years old man Not passed urine for 20 hrs O/E: large bladder and prostate on PR Creatinine: 8.3 mg/dl USS- dilated bladder Urine catheter inserted, start to pass lots of urine Following day creatinine – 4.2 but then over subsequent days rises to 5.1 then 5.8 then 6.4. still passing lots of urine What is the right intervention A- Restrict fluid to reduce urine output B- Give IV normal saline C- Remove catheter D- Investigate for other causes of renal failure What is the right intervention A- Restrict fluid to reduce urine output B- Give IV normal saline C- Remove catheter D- Investigate for other causes of renal failure Post recovery diuresis • Occurs post resolution of AKI - Post relief of obstruction - Post ATN • Important to check fluid status - Clinical exam - BP and pulse - Daily weight - Input and output chart • Treatment – IV fluids replace electrolyte Complication of AKI • 64 years old man admitted with: Potassium 7.4 Urea: 90 Creatinine: 8.5 What is the first line treatment A- Insulin and dextrose B- IV calcium gluconate C- Ca+2 resonium D- Low potassium diet E- Dialysis What is the first line treatment A- Insulin and dextrose B- IV calcium gluconate C- Ca+2 resonium D- Low potassium diet E- Dialysis Other Complications of AKI • • • • Pulmonary oedema Acidosis Uraemia Other electrolyte disturbance such as hyerphosphataemia and hypocalcaemia Who is a risk? Many cases of AKI should never occur in the first place 1- Elderly 2- Pre-existing renal disease 3- Surgery, trauma, sepsis or myoglobinuria 4- Diabetes 5- Volume depletion( Nil By Mouth, bowel obstruction, burn) 6- LV dysfunction 7- Nephrotoxic drugs 8- Cirrhosis (reduce arterial volume) Common nephrotoxins • NSAID • Diuretics, ACEI, ARB2 especially in volume depleted patient • Antibiotics, Aminoglycosides, Vancomycin • Amphotericin B • Immunosuppressant (ciclosporin, tacroliums) and chemotherapy (Cisplatin) • IV contrast Reducing risk perioperatively • Three principles: 1- Avoid dehydration 2- Avoid nephrotoxins 3- Review clinical status and renal function those at risk • Optimize volume status 1- No patient should go to theatre dehydrated 2- Review daily weight, input and output chart 3- Calculate losses especially those NBM ( use 0.9% N saline and NOT 5% Dextrose) Reducing risk perioperatively • Optimize blood sugar control in DM ( use sliding scale • Catheterize those with prostate disease • Avoid surgery if possible immediately after a contrast procedure • Stop nephrotoxic drugs 24-48hrs preoperatively • Review the patient EARLY postoperatively Have you.. • Have seen the result of K and acted appropriately? • Assessed the patient’s volume status and treated pulmonary oedema or corrected hypovolaemia? • Taken full history and examined patient head to toe? • Excluded palpable bladder? • Seen the patient’s regular drugs? And stopped nephro-toxins? • Arranged urgent ultrasound(within 24hr)* • Performed urine test and send for microscopy and MSU • Checked acid-base status and intervened appropriately? • Checked for any previous tests of renal function? • Checked Hb, Calcium and Phosphate? • Send blood for full nephritic and myeloma screen if you are suspecting intrinsic renal failure? * NCEPOD recommendation/ National Confidential Enquiry in to patient outcome and death. www.ncepod.org.uk Acute kidney injury Pre renal - ↓ Effective circulatory volume: 1- Haemorrhage 2- Volume depletion 3- Low cardiac output 4- Sepsis 5- CCF 6- Cirrhosis Intrinsic Vascular: 1- vasculitis 2- Thrombotic microangiopathies Post renal Acute GN Acute TIN ATN ( Glomerluonephritis) (tubulo-intestitial nephritis) (acute tubular necrosis) Obstruction 1- Bladder out-let obstruction 2- Bilateral ureteral obstruction 3- hypertensive emergencies Ischaemic Nephrotoxic - Arterial stenosis/Occlusion Endogenous - Vasomotor: 1- Haemoglobinuria 1- NSAID 2- ACEI/ ARBs 2- Myoglobinuria 3- Myoglobin casts 4- Intratubular crystals Exogenous 1- Nephrotoxic drugs 2- Radiocontrast Summary • 3 categories of AKI • Simple clinical assessment will define which • Be aware of life threatening complications and emergency treatment • Recognise those at risk