Atiya Khalid
GPST1
A & E;AGH
Defination:
DVT is the formation of a thrombus (blood clot) in a
deep vein, usually in the legs, which partially or
completely obstructs blood flow.
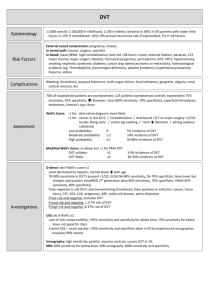
Epidemiology:
1 in 1000 /yr
Male: female = 1.2:1
Two thirds of proven PE have no symptoms of DVT
5-15% with untreated DVT may die from PE
Autopsy studies demonstrate that approximately 80% of all cases of
DVT and PE remain undiagnosed, (even when they are the immediate
cause of death)
Risk factors:
Intrinsic Risk Factors:
Cancer (known or undiagnosed).
Increasing age, being overweight or obese, and male sex.
Heart failure.
Acquired or familial thrombophilia.
Chronic low-grade injury to the vascular wall (vasculitis,
hypoxia from venous stasis, or chemotherapy)
Risk Factors: (contd)
Risk factors that temporarily raise the likelihood of
DVT
Immobility ( following stroke, operation, plaster cast,
hospitalization, or long-distance travel).
Significant trauma or direct trauma to a vein
(intravenous catheter).
Hormone treatment (oestrogen-containing
contraception or HRT ).
Pregnancy and the postpartum period.
Dehydration.
Clinical features
Limb pain and tenderness along the line of the deep veins.
Swelling of calf or thigh (usually unilateral). Can be
bilateral ( iliac bifurcation,pelvic vein,vena caval
involvemnet)
Distension of superficial veins.
Increase in skin temperature.
Skin discolouration (erythema or purple or cyanosed).
A palpable cord (hard, thickened palpable vein).
Low-grade fever ( rare).
There may be pain upon dorsiflexion of the foot (Homans'
sign is not helpful in diagnosis as it is very non-specific_
DVT difficult to diagnose clinically
Many DVTs progress to PE without DVT being clinically
apparent.
In those with classic clinical signs, only about 50% have
DVT.
History, examination and the presence of risk factors can
be unreliable in making the diagnosis, and ambulatory
patients (as in primary care) may be rather different from
hospital inpatients, who are the group most studied.
Cellulitis adds to problem
Severe signs of DVT can resemble cellulitis
Secondary cellulitis may develop with primary DVT
Primary cellulitis may be followed by a secondary DVT
Superficial thrombophlebitis may hide an underlying DVT
Differential Dx
Physical trauma
Calf muscle tear or strain.
Haematoma
Sprain or rupture of a leg tendon.
Fracture.
Cardiovascular dis
Superficial thrombophlebitis
Post-thrombotic syndrome
Venous obstruction or insufficiency, or external compression of
major veins (by fetus, cancer).
Arteriovenous fistula and congenital vascular abnormalities.
Vasculitis.
Heart failure.
D/D Contd
Other conditions include:
Ruptured Baker's cyst
Cellulitis (commonly mistaken as DVT).
Dependent (stasis) oedema.
Lymphatic obstruction.
Septic arthritis.
Cirrhosis.
Nephrotic syndrome
Management:
Refer immediately for same-day assessment and
management:
If DVT is suspected in
a pregnant woman
6/52 post-partum
IVDU
D-dimer testing not available or practical
If D-dimer testing is available, use the Wells Clinical
Prediction Rule to assess the probability of a DVT.
Management:
Risk assessment
Score one point for each of the following:
Active cancer (treatment ongoing or within the last 6 months)
Paralysis, paresis or recent plaster immobilisation of the legs
Recently bedridden for more than 3 days or major surgery within the
last 12 weeks
Localised tenderness along the distribution of the deep venous system
(such as the back of the calf)
Entire leg is swollen
Calf swelling by more than 3 cm compared with the asymptomatic leg
(measured 10 cm below the tibial tuberosity)
Pitting oedema (greater than on the asymptomatic leg)
Collateral superficial veins (non-varicose)
Previously documented DVT
Mx Contd
Subtract two points if an alternative cause is considered
The risk of DVT is likely if the score is two or more, and unlikely
if the score is one or less.
Refer people who are likely to have DVT for same-day assessment
and management.
For people who are unlikely to have DVT:
D-dimer testing if available, and it is reasonably
practical and safe to do so ( results will be reported that
day).
If the D-dimer test is positive, refer immediately for further
assessment and management.
If the D-dimer test is negative, reassure the person, and tell
them to seek urgent medical advice if they develop difficulty
breathing, increased breathing rate, or chest pain (since these
symptoms may indicate pulmonary embolism).
Mx:
Definitive Investigations:
USS
Venography
MRI
Mx
A Practical Approach in GP setting:
Patients likely to have a DVT on the grounds of clinical suspicion
or risk factors should be referred immediately to hospital.
For people who are unlikely to have DVT, perform a D-dimer test
if available.
If the test is positive, refer immediately for further assessment and
management.
If the test is negative, reassure the person, and tell them to seek
urgent medical advice if they develop difficulty breathing, increased
breathing rate, or chest pain (since these symptoms may indicate
pulmonary embolism).
If D-dimer testing is not available or practical, refer for same-day
assessment.
Treat the suspicion of DVT with subcutaneous LMWH if no
contra-indications.1
Target Ranges
Patients with confirmed DVT are usually commenced on
warfarin
A loading dose of warfarin is needed usually
First episode of a proximal vein thrombosis should receive
anticoagulants for 6 months, with a target INR of 2.5 (±0.5
is acceptable), duration-debatable
INR 3.5 if recurrence or mechanical valves
BTSconcluded that if VTE arises after surgery, 4 weeks of
anticoagulation should be adequate.
In other settings, patients with new DVT, PE, or both, who
do not have a persisting underlying cause or risk factor,
should receive anticoagulants for 3/12
Thankyou