Paediatric Urology 2, North Western Deanery Urology Teaching
Monday, 29 July 2013
Vesico-ureteric reflux
Ivo Dukic, Zubeir Ali, Mr Guy Wemyss-Holden
Introduction
• Theory and background
• Cases
– EAU Guidelines
– Key papers
– Practical management
– Discussion
• Viva questions as we go along
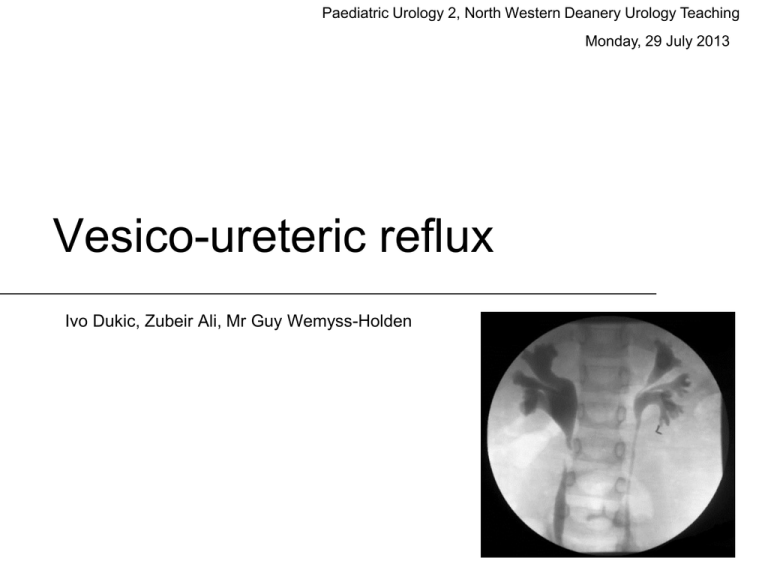
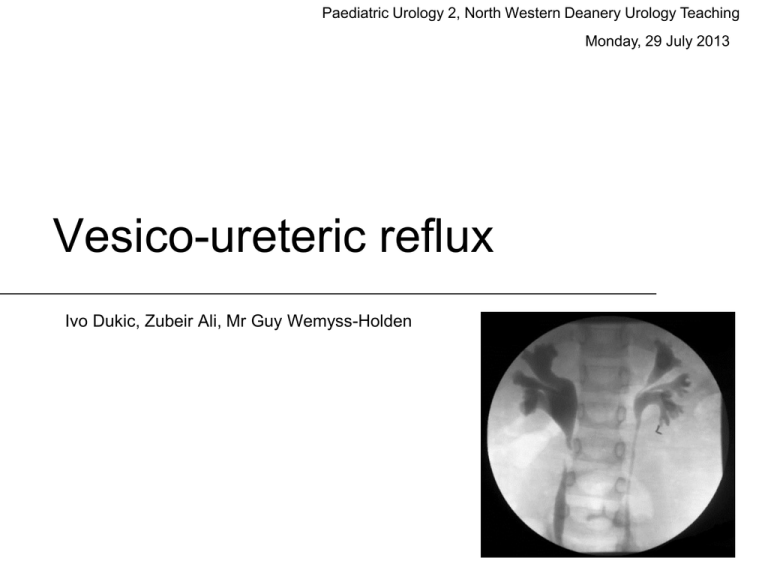
What is the most appropriate grade of vesico-ureteric reflux as per the
international reflux study committee 1985?
12 year old boy, presented following a trauma, what is the most
appropriate grade of vesico-ureteric reflux as per the international
reflux study committee 1985?
Background
• Vesico-ureteric reflux is the:
– “The non-physiological back-flow of urine from the
urinary bladder into the ureter or the renal pelvis and
calyces”
• VUR can be divided into:
– Primary = Congenital anomaly of VUJ
– Secondary = Due to anatomical or functional bladder
outflow obstruction with subsequent reflux e.g.
Posterior urethral valves, spina bifida
Coleman, R., 2011. Early management and long-term outcomes in primary vesicoureteric reflux. BJU international, 108 Suppl 2, pp.3–8.
Epidemiology
•
•
•
•
1% of children
10 times as common in white children
Newborns – M>F
Higher grades of VUR in males and more
spontaneous resolution
• Children >1yrs – F 5-6x >M
Case 1
• A 20 month girl has been referred to you from the GP
following a febrile episode. The urine sample taken at
the time has a confirmed E Coli UTI.
• The mum tells you that she has had no problems since
birth but there was a dilated kidney which was checked
and resolved in the first 6 months
• What are the causes for antenatal hydronephrosis?
Case 1
• What are the causes for an antenatal
hydronephrosis?
• PUJ obstruction (40%)
• VUJ obstruction or megaureter
• Vesico-ureteric reflux – 16.2% (7-35%)
– Posterior urethral valves (60% VUR)
– Cloaca (60% VUR), Duplex kidney (46%)
– Neurogenic bladder
Tekgül, S. et al., 2013. EAU and ESPU guidelines on
Paediatric Urology. European Association of Urology.
Sung, J. & Skoog, S., 2012. Surgical management of
vesicoureteral reflux in children. Pediatric Nephrology (Berlin,
Germany), 27(4), pp.551–561
Case 1
• How do you investigate a child with
hydronephrosis in the postnatal period?
Case 1
• How do you investigate a child with
hydronephrosis in the postnatal period?
– Typically 7 days after birth
– Immediately if bilateral, oligohydranmnios,
solitary kidney, pulmonary hypoplasia
– Renal USS
– MAG 3 renography 4-6 week of life
– VCUG recommended in bilateral
hydronephrosis, ureterocele, ureteral dilation
and abnormal bladders
Case 1
• How would evaluate the patient?
– Which factors are important?
• History
• Examination
• Investigations
Management goals
1. Prevent recurring febrile UTI
2. Main goal in management of patients with
VUR is preservation of renal function
3. Minimise the morbidity of treatment and
follow up
Peters, C.A. et al., 2010. Summary of the AUA Guideline on
Management of Primary Vesicoureteral Reflux in Children. The
Journal of urology, 184(3), pp.1134–1144.
Evaluation
• Risk factors
– Age
– Sex
– Reflux grade (VCUG)
– Lower urinary tract dysfunction
– Anatomic abnormalities
– Kidney status
Evaluation
•
•
•
•
•
Blood pressure
Height and weight
Urine for blood, proteinuria, bacteriuria
Serum creatinine
Renal USS and consider
– VCUG
– DMSA
Investigations
• EAU guidelines 2013
– VCUG recommend at age 0-2 year after first
proven febrile UTI
– If reflux diagnosed, DMSA recommended
(usually for grade 3 and above)
– In those with LUTD and febrile UTI, VCUG
recommended at may have a worse final
treatment outcome (Swedish Reflux Study 2010)
– Performing a VCUG
Investigations
• Alternative “top down approach” - ESPR
•
•
•
•
DMSA at time of febrile UTI
VCUG if DMSA reveals renal involvement
Misses VUR in 5-27%,
Avoids unnecessary VCUG in >50% of screened
Classification of VUR
Lebowitz, R.L. et al., 1985. International system of radiographic Diamond, D.A. & Mattoo, T.K., 2012. Endoscopic Treatment of
grading of vesicoureteric reflux. International Reflux Study in
Primary Vesicoureteral Reflux. New England Journal of
Children. Pediatric radiology, 15(2), pp.105–109.
Medicine, 366(13), pp.1218–1226.
Case 1
Grades?
Abnormality?
Why does lower pole
system relfux more
frequently?
Diamond, D.A. & Mattoo, T.K., 2012. Endoscopic Treatment of Primary
Vesicoureteral Reflux. New England Journal of Medicine, 366(13), pp.1218
1226.
Case 1
• What management options would you
recommend?
Management options
• Conservative therapy
–
–
–
–
–
–
–
VUR spontaneous resolution, watchful waiting
Regular toileting, hygiene
Urine surveillance
Treat underlying bladder dysfunction
Treat constipation
Prompt treatment of breakthrough infections
Repeat imaging as required
VUR Prognosis
Grade
Spontaneous resolution over 5 year
period
I
82%
II
80%
III
46%
IV
30%
V
13%
Coleman, R., 2011. Early management and long-term outcomes in primary vesicoureteric reflux. BJU international, 108 Suppl 2, pp.3–8.
VUR - Prognosis
• Resolution of VUR correlates with renal and
bladder functional status
– Yeung et al, 94% resolution with normal bladder
function, 37% with abnormal renal function, none with
abnormal bladder function
• Older the child when VUR diagnosed the less
likely their reflux will resolve
• Secondary reflux has worse prognosis
Yeung, C.K. et al., 2006. Renal and bladder functional status at
diagnosis as predictive factors for the outcome of primary
vesicoureteral reflux in children. The Journal of urology, 176(3),
pp.1152–1156; discussion 1156–1157.
Medical therapy
• Intermittent antibiotic prophylaxis
• Continues antibiotic prophylaxis (CAP)
• Bladder rehabilitation in those with LUTD
Management guidelines
• All patients diagnosed in first year of life should
be treated with CAP
• Definitive surgical or endoscopic correction is
preferred in those with frequent breakthrough
infections
• If presenting at 1-5 years of age
– Grade 1-2 reflux and no symptoms, close surveillance
without Abx prophylaxis may be an option
– Grade 3-5 reflux, CAP is preferred option for initial
therapy, surgical correction is reasonable alternative
Case 2
• 4 year old boy with Grade III VUR
diagnosed on VCUG at paediatric hospital
• Referred with ballooning of the foreskin,
possible balanitis and a febrile infection in
the last 12 months
Case 2
• What factors are important in evaluation?
Evaluation
• Risk factors
– Age
– Sex
– Reflux grade (VCUG)
– Lower urinary tract dysfunction
– Anatomic abnormalities
– Kidney status
– Balanitis episodes, BXO, frequency of
balanitis
Case 2
• What management options are available
for this patient?
• What would you advise is the best
management and why?
Case 2
• Circumcision
– NNT 4 to prevent febrile UTI in Grade 3 or
above VUR
– Alternative view, no difference in those
undergoing Cohen procedure with or without
circumcision
Singh-Grewal, D., Macdessi, J. & Craig, J., 2005. Circumcision
for the prevention of urinary tract infection in boys: a systematic
review of randomised trials and observational studies. Archives
of Disease in Childhood, 90(8), pp.853–858.
Kwak, C. et al., 2004. Effect of circumcision on urinary
tract infection after successful antireflux surgery. BJU
international, 94(4), pp.627–629.
Case 2
• You start the patient on CAP and arrange
an early review in your clinic in 4 months
time. However, the child is admitted twice
in the next four months with a febrile UTI?
• How would you proceed?
Management options
• Continue with CAP (alternate antibiotics)
• Surgical treatment
– Subureteral injection of bulking materials
Grade
Reflux resolution after
one treatment
1 and 2
78.5%
3
72%
4
63%
5
51%
Elder, J.S. et al., 2006. Endoscopic therapy for vesicoureteral
reflux: a meta-analysis. I. Reflux resolution and urinary tract
infection. The Journal of urology, 175(2), pp.716–722.
STING and HIT procedures
•
•
•
•
•
•
Endoscopic – STING (subureteric Teflon injection)
O'Donnell and Puri 1986
75% success after one treatment.
Few problems and can be repeated
Learning curve Kirsh et al 2003.
Safety in animals migration of particles to distant sites (brain
and lung)
• Other agents attempted but PTFE gives highest response
rates; deflux (dextranomer hyaluronic coploymer) is the only
FDA approved substance for endoscopic correction of Gd II-IV
• HIT – Hydrodistention implantation technique
Diamond, D.A. & Mattoo, T.K., 2012. Endoscopic Treatment of Primary
Vesicoureteral Reflux. New England Journal of Medicine, 366(13),
pp.1218–1226.
HIT
Double
HIT
1
2
Swedish reflux trial
• 203 children, age 1-2 years, grade III/IV
reflux, randomised 3 treatments, 2 year
follow up
Endoscopic
injection
Antibiotic
prophylaxis
Surveillance
Resolution
71%
39%
47%
Febrile UTI
23%
19%
57%
Scar formation
7%
0%
11%
Brandström, P. et al., 2010. The Swedish reflux trial in children:
IV. Renal damage. The Journal of urology, 184(1), pp.292–297.
Case 3
• 1 year old girl who is asymptomatic
referred by the paediatricians as her sister
has been diagnosed with VUR
• How would you evaluate and manage this
patient?
Primary VUR - Aetiology
• Genetic basis for VUR – autosomal dominant
• Siblings of patients with VUR have a 27%
average prevalence of reflux
• Offspring of parents with VUR have an
almost 36% prevalence
Peters, C.A. et al., 2010. Summary of the AUA Guideline on
Management of Primary Vesicoureteral Reflux in Children. The
Journal of urology, 184(3), pp.1134–1144.
Tekgül, S. et al., 2012. EAU guidelines on vesicoureteral
reflux in children. European urology, 62(3), pp.534–542.
Sibling screening
• Associated with lower grades
• Significantly earlier resolution
• If discovered with UTI, often high grade
Sibling screening
• EAU recommends informing parents of
high prevalance of VUR in siblings and
offspring
• If screening perfomed, renal USS
• VCUG recommended if evidence of renal
scarring, or history of UTI
• In toilet trained children no value in
screening for VUR
Tekgül, S. et al., 2012. EAU guidelines on vesicoureteral
reflux in children. European urology, 62(3), pp.534–542.
Case 4
• 6 year old girl referred by GP for
management of VUR
• Initial presentation at 1 year of age with
temp of 39.2°C and irritability, E Coli in
urine. Subsequent VCUG showed Grade
IV VUR and renal scarring on USS.
• Toilet trained at 2 years of age, antibiotics
stopped at this point
Case 4
• How would you assess the patient?
Case 4
• Does she need further investigation?
– Which investigations and why?
Case 4
The parents have a number of concerns
which the GP was unable to answer
1. Will the girls VUR resolve?
Case 4
1. Should she have further treatment?
2. What circumstances would warrant
further treatment?
3. What are the treatment options?
Surgical Management
• Cystoscopic
– STING / HIT / Double HIT procedure
• Open surgery
–
–
–
–
Cohen
Lich-Gregoir
Glenn Anderson, Politano-Leadbetter
Psoas hitch ureteroneocystostomy
• Laparoscopic reflux correction
Cohen cross trigonal (1975)
Mure, P.-Y. & Mouriquand, P.D.E., 2004. Surgical Atlas The Cohen procedure. BJU
International, 94(4), pp.679–698.
Leadbetter Politano
Steffens, J. et al., 2006. Surgical Atlas Politano-Leadbetter ureteric reimplantation. BJU
International, 98(3), pp.695–712.
Lich-Gregoir (extravesical)
Riedmiller, H. & Gerharz, E.W., 2008. Antireflux surgery: Lich-Gregoir extravesical ureteric
.
tunnelling. BJU International, 101(11), pp.1467–1482
Laparoscopic Correction
• Laparoscopic
• Most well described Gil-Vernet procedure
• Lower success rates than open procedures
Success rates of surgery
• 98% in some centres
– Problems with ureteral obstruction
– Contralateral obstruction or reflux
• 10 year results of Internaional Reflux
Study in Children concluded that no
difference between ureteral reimplantation
or antibiotic prophylaxis in those with
Grade III/IV reflux <11 years
Jodal, U. et al., 2006. Ten-year results of randomized treatment
of children with severe vesicoureteral reflux. Final report of the
International Reflux Study in Children. Pediatric Nephrology,
21(6), pp.785–792.