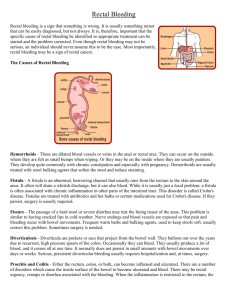
Rectal Bleeding
Matthew Charnock
Sam Newton
PC
HPC
RED FLAGS
ROS
MED Hx
FH
SOCIAL Hx
73 year old female
Suffers from T2DM and Ulcerative Colitis
Presented 3/52 history of rectal bleeding
Mixed in with stool
Loose stools for past 6 weeks
Lost 2 stone in past 12 weeks
Smokes 30/day for 50 years
No abdominal pain
DVT 4 weeks ago
Bloods
Imaging
Colorectal cancer is the third most common cancer in the UK
2nd most common cause of cancer death in the UK
75% occur in people aged 65 or over
Screening in UK - FOBT
Family history
Familial Syndromes
IBD
Smoking
Poor fibre/High fat diet
Alcohol
Etc
Right sided colon cancers
Change in bowel habit , weight loss, anaemia , occult bleeding , mass in right iliac fossa, disease more likely to be advanced at presentation
Left sided colon cancers colicky pain, rectal bleeding , bowel obstruction, mass in left iliac fossa, early change in bowel habit , less advanced disease at presentation
Rectal cancers as above + tenesmus
Jaundice?
Ascites?
Chronic cough?
Abdominal pain
Bloody diarrhoea
Weight loss
Fever
Signs of anaemia
Tenesmus
Peri-anal disease
Extra-intestinal manifestations
In children – FTT, delayed puberty, malnutrition
Crohns VS Ulcerative Colitis
Bloods (FBC, LFTs, ESR/CRP, Anti-
GGT/endomysial antibodies, Iron Studies,
B12/Folate levels)
Imaging
Colonoscopy + biopsy
Barium Follow through
Abdominal xray
Smoking cessation in Crohns
Medical
5 aminosalicyclic acid derivatives
(5ASA’s – mesalazine)
Corticosteroids (in acute flare up)
Enteral nutrition
Immunosuppressants
(cyclosporin/methotraxate/azathioprine)
Cytokine modulators (infliximab)
Indications in UC
Failure of medical treatment
Toxic megacolon
Perforation
Haemorrhage
Cancer prophylaxis
Procedure
Temporary – proctocolectomy with ileoanal pouch formation
Permanent – panproctocolectomy with end ileostomy
Indications in Crohns
Strictures - strictuoplasty
Fistulas – lay open (low)/seton suture (high)
Abscess – drainage +/- Abx
Unresponsive to medical treatment - segmental resection
Intolerable long term symptoms
Site
Contents of bag
Appearance
•
•
•
•
•
•
•
•
•
Obese 59 year old male
No significant past medical history
Presented to GP with a 2 week history of rectal bleeding
Small amount of blood on the toilet paper after defecating
First occurred following straining on the toilet
Also itching around the back passage
No pain, no change in bowel habit, no N+V
Feels otherwise well
ROS- none
•
Rectal examination?
•
Bloods?
•
Imaging?
•
•
•
•
•
•
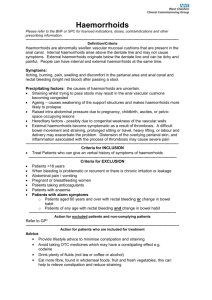
Commonest cause of rectal bleeding
Benign condition in which the venous cushions within the rectum become enlarged
RF’s - prolonged straining and time on the toilet, raised intra-abdominal pressure eg- pregnancy, obesity, heavy lifting etc
Symptoms include- rectal bleeding, rectal itching
(pruritus ani), feeling of discomfort or discharge, may feel mass, may be asymptomatic
Blood should not be mixed in, usually on toilet paper or streaks in the bowl
Classification is broken into internal and external haemorrhoids, internal above the dentate line, external below dentate line.
•
•
•
•
1 st degree- do not prolapse
2 nd degree- prolapse on defecation return spontaneously
3 rd degree- prolapse on defecation, need to be manually reduced
4 th degree- permanently prolapsed
•
•
•
•
•
On rectal exam, typically present at the 3,7 and 11 o clock positions
Internal haemorrhoids may be impalpable and not visible on inspection
Internal haemorrhoids should be painless
Asking the patient to bear down may reveal haemorrhoids on inspection
Important to perform to exclude other anal pathology
•
•
•
1.
2.
3.
Conservative- increase dietary fibre, decrease time on the toilet, strain less, lose weight, laxative (for 1 st and 2 nd degree)
Non- surgical (for 3 rd /4 th or 1 st /2 nd not responding to conservative)
Banding
Sclerotherapy
Infrared coagulation
1.
Surgical (3 rd /4 th not responding or very large)
Circular stapled haemorrhoidectomy (better than traditional)
•
•
•
•
•
•
•
•
64 year old female
PMH of IHD and PVD
Presented with a 1 month history of LIF abdominal pain, bloating and change in bowel habit- constipated
Also noticed single episode of blood mixed in with stool
Also noticed intermittent nausea although no vomiting
No pyrexia
Otherwise well
ROS- frothy urine?
•
O/E- patient relatively well, abdo- some tenderness in the
LIF, PR- NAD
•
Bloods?
•
Imaging?
•
•
•
•
1.
2.
3.
Herniation's of mucosa through colonic muscle
Remember terminology
Diverticulosis- ASYPTOMATIC but has diverticula
Diverticular disease- SYPTOMATIC with diverticula
Diverticulitis- Infection with inflammation of a diverticula
RF’s- Age, low dietary fibre, obesity
More likely to occur on the left in Caucasians and commonly occur at the insertion points of blood vessels
•
•
1.
2.
3.
4.
1.
2.
3.
4.
Diverticular disease:
Abdo pain, usually left sided
Abdo bloating
Change in bowel habit
Rectal bleeding
Diverticulitis:
More severe LIF pain with localised tenderness
Pyrexia, fever, tachycardia- may be in shock
Possibly N+V
Haemorrhage and other complications
•
•
1.
2.
Bloods- FBC, U+E, CRP, ESR, Clotting, Group+ save
Imaging-
Colonoscopy- exclude other pathology and confirm diagnosis, NOT in acute presentation- why?
Barium enema
3.
4.
Erect CXR- why?
AXR- may show evidence of complications
5.
CT- useful acutely when colonoscopy CI’d
•
•
•
•
1.
2.
Fistula-
Colovesical- pneumaturia- frothy urine
Colovaginal
•
•
3.
Coloenteric
Bowel obstruction
Abscess
Perforation
Stricture
Haemorrhage
•
•
1.
Diverticular disease-
High fibre diet
2.
3.
1.
Good fluid intake
May require laxatives, antispasmodics, analgesia
Diverticulitis-
May require hospital admission
2.
3.
4.
5.
Antibiotics- may need broad spectrum
Fluids
Analgesia
Manage complications- eg may require blood transfusion etc
•
•
•
•
1.
2.
3.
15-30% may need surgery
Emergency procedure for acute diverticulitis is a
HARTMANNS procedure
Involves removing affected part and bringing part of the large bowel to the surface of the skin to create a temporary colostomy which can be reversed at a later date upon recovery
Surgery may also be performed for complications including:
Fistula
Obstruction
Stricture (possibly)
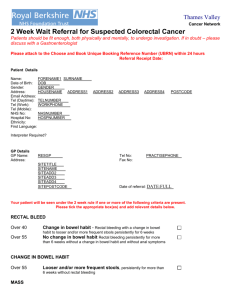
Person
40 years of age and older
60 years of age and older
Symptoms and signs
Rectal bleeding with a change in bowel habit towards looser stools and/or increased stool frequency persisting for
6 weeks or more.
Rectal bleeding persisting for 6 weeks or more without a change in bowel habit and without anal symptoms. A change in bowel habit to looser stools and/or more frequent stools persisting for 6 weeks or more without rectal bleeding.
Of any age A right abdominal mass consistent with involvement of the large bowel. A palpable rectal mass (intraluminal and not pelvic; a pelvic mass outside the bowel would warrant an urgent referral to a urologist or gynaecologist).
Women (not menstruating)
Men of any age
Unexplained iron deficiency anaemia and haemoglobin
10 g/100 mL or less.*
Unexplained iron deficiency anaemia and haemoglobin
11 g/100 mL or less.*
* Anaemia considered, on the basis of history and examination in primary care, not to be related to other sources of blood loss (e.g. ingestion of nonsteroidal anti-inflammatory drugs) or blood dyscrasia.
1.
2.
Anal fissure
Gastroenteritis
3.
4.
Angiodysplasia
Meckel's diverticulum
5.
Polyp
6.
7.
Trauma
Rectal varices
Any Questions?