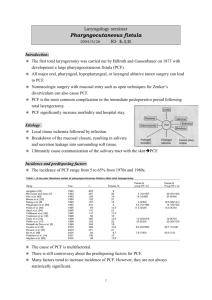
Pharyngocutaneous Fistulas after Salvage Laryngectomy: Need for
Wojciech K. Mydlarz, M.D.
“Pharyngocutaneous Fistulas after
Salvage Laryngectomy: Need for
Vascularized Tissue”
Disclosures
• No Relevant Financial Relationships or
Commercial Interests
Educational Objectives
• Discuss risk factors for fistula after salvage total laryngectomy
• Discuss prevention of fistulas after salvage total laryngectomy
• Discuss outcomes and complications of various surgical management options of fistulas.
Overview
• Background
• Risk factors for pharyngocutaneous fistulas (PCF) after Salvage Total
Laryngectomy (TL)
• Prevention of PCF after Salvage TL: vascularized tissue
• Outcomes
Clinical Background
• Laryngeal Cancer:
• Supraglottis (epiglottis, arytenoids, aryepiglottic folds, false cords)
• Glottis (true cords, anterior and posterior commissures)
• Subglottis
Clinical Background
2006 ASCO
• New cases of laryngeal cancer to be diagnosed
(U.S., 2005): 9,880
• Newly diagnosed cases that will lead to death
(U.S., 2005): 3,770
• 95% of laryngeal cancers are invasive with squamous cell carcinoma as the predominant histologic type
• 40% of patients will have stage III or IV laryngeal cancer (upon first evaluation)
• 25% of healthy people are willing to trade a 20% absolute difference in survival for the opportunity to save their voice
Clinical Background
• Tobacco and/or alcohol use are associated with most cases of laryngeal cancer
• Continued tobacco and/or alcohol use complicates treatment and facilitates medical comorbidity and the development of second primary cancers.
Clinical Background
• Larynx-preservation options include:
– Radiation therapy
– Chemoradiation therapy
– Function-preserving partial laryngectomy procedures
• TL is surgical procedure most feared by patients. Common sequelae:
– Social isolation
– Job loss
– Depression
Clinical Scenario
• 54 year-old man s/p 35 doses of 2 Gray RT over 7 weeks for a
T3NOMO squamous cell carcinoma of the right vocal cord
• 6 months later undergoes biopsy because of suspicion of recurrence.
• PMH significant for non–insulin-dependent diabetes mellitus and hypertension.
• Patient continues to smoke 10 cigarettes per day, which has decreased from 25 cigarettes per day before diagnosis of laryngeal cancer. He consumes about 4 beers per day.
• Biopsy histopathology positive for residual tumor.
Multidisciplinary oncology board recommends salvage TL surgery.
• Potential complications of TL discussed with patient, including
PCF. The patient asks about what are his risks for a fistula?
PCF After Total Laryngectomy
Aarts MCJ et al. “Salvage Laryngectomy After Primary Radiotherapy: What Are Prognostic Factors for the
Development of Pharyngocutaneous Fistulae?” Otolaryngology–Head and Neck Surgery 144(1) 5–9
PCF After Total Laryngectomy
Aarts MCJ et al. “Salvage Laryngectomy After Primary Radiotherapy: What Are Prognostic Factors for the
Development of Pharyngocutaneous Fistulae?” Otolaryngology–Head and Neck Surgery 144(1) 5–9
PCF After Total Laryngectomy
Aarts MCJ et al. “Salvage Laryngectomy After Primary Radiotherapy: What Are Prognostic Factors for the
Development of Pharyngocutaneous Fistulae?” Otolaryngology–Head and Neck Surgery 144(1) 5–9
• multivariate logistic regression analysis: only initial T stage & tumor site remained as independent prognostic factors
• Odds ratio (OR) for tumor stage:
– 2.08 (95% confidence interval [CI] =
1.26-3.45)
– T3-4 in comparison to T1-2 for developing PCF
• OR for tumor site:
– 2.08 (95% CI = 1.25-3.45)
– Non-glottic tumors in comparison with glottic tumors.
PCF After Total Laryngectomy
Paydarfar JA, Birkmeyer NJ. “Complications in Head and Neck Surgery : A Meta-analysis of Postlaryngectomy Pharyngocutaneous
Fistula.” Arch Otolaryngol Head Neck Surg. 2006;132:67-72.
PCF After Total Laryngectomy
Paydarfar JA, Birkmeyer NJ. “Complications in Head and Neck Surgery : A Meta-analysis of Postlaryngectomy Pharyngocutaneous
Fistula.” Arch Otolaryngol Head Neck Surg. 2006;132:67-72.
PCF After Total Laryngectomy
Paydarfar JA, Birkmeyer NJ. “Complications in Head and Neck Surgery : A Meta-analysis of Postlaryngectomy Pharyngocutaneous
Fistula.” Arch Otolaryngol Head Neck Surg. 2006;132:67-72.
PCF After Total Laryngectomy
Paydarfar JA, Birkmeyer NJ. “Complications in Head and Neck Surgery : A Meta-analysis of Postlaryngectomy Pharyngocutaneous
Fistula.” Arch Otolaryngol Head Neck Surg. 2006;132:67-72.
Prevention of PCF:
Vascularized Tissue-Pectoralis
Patel UA, Keni SP. “Pectoralis myofascial flap during salvage laryngectomy prevents PCF.” Otolaryngology-head and Neck Surgery
141, 190-195.
Prevention of PCF:
Vascularized Tissue-Pectoralis
Patel UA, Keni SP. “Pectoralis myofascial flap during salvage laryngectomy prevents PCF.” Otolaryngology-head and Neck Surgery
141, 190-195.
Prevention of PCF:
Vascularized Tissue-Pectoralis
Gil Zm et al. “The role of Pectroalis Major Muscle Flap in Salvage TL.” Arch of Otolaryngology-Head and Neck Surgery 135, 1019-
1023.
Prevention of PCF:
Vascularized Tissue-Pectoralis
Gil Zm et al. “The role of Pectroalis Major Muscle Flap in Salvage TL.” Arch of Otolaryngology-Head and Neck Surgery 135, 1019-
1023.
Prevention of PCF:
Vascularized Tissue-Free Flap
Fung K, et al. “Prevention of Wound complications following salvage TL using free vascularized tissue.” Head and Neck May 2007.
Prevention of PCF:
Vascularized Tissue-Free Flap
Fung K, et al. “Prevention of Wound complications following salvage TL using free vascularized tissue.” Head and Neck May 2007.
Prevention of PCF:
Vascularized Tissue-Free Flap
Fung K, et al. “Prevention of Wound complications following salvage TL using free vascularized tissue.” Head and Neck May 2007.
Prevention of PCF:
Vascularized Tissue-Free Flap
Fung K, et al. “Prevention of Wound complications following salvage TL using free vascularized tissue.” Head and Neck May 2007.
Prevention of PCF:
Vascularized Tissue-Free Flap
Withrow KP, et al. “Free Tissue Transfer to Manage Salvage Laryngectomy Defects After Organ Preservation Failure.” Laryngoscope
117, May 2007.
Prevention of PCF:
Vascularized Tissue-Free Flap
Withrow KP, et al. “Free Tissue Transfer to Manage Salvage Laryngectomy Defects After Organ Preservation Failure.” Laryngoscope
117, May 2007.
Prevention of PCF:
Vascularized Tissue-Free Flap
Withrow KP, et al. “Free Tissue Transfer to Manage Salvage Laryngectomy Defects After Organ Preservation Failure.” Laryngoscope
117, May 2007.
Outcomes of Vascularized
Tissue Transfer
Clark JR, et al. “Morbidity After Flap Reconstruction of Hypopharyngeal Defects.” Laryngoscope 116, May 2006.
Outcomes of Vascularized
Tissue Transfer
Clark JR, et al. “Morbidity After Flap Reconstruction of Hypopharyngeal Defects.” Laryngoscope 116, May 2006.
Outcomes of Vascularized
Tissue Transfer
Clark JR, et al. “Morbidity After Flap Reconstruction of Hypopharyngeal Defects.” Laryngoscope 116, May 2006.
Outcomes of Vascularized
Tissue Transfer
Clark JR, et al. “Morbidity After Flap Reconstruction of Hypopharyngeal Defects.” Laryngoscope 116, May 2006.
Outcomes of Vascularized
Tissue Transfer
Clark JR, et al. “Morbidity After Flap Reconstruction of Hypopharyngeal Defects.” Laryngoscope 116, May 2006.
Summary
• PCF can occurr after salvage TL
• Previous radiotherapy, tumor location and T stage are important risk factors
• Vascularized tissue plays a role in prevention of PCF after Salvage TL
• Pectoralis major and free flaps can both be used to help prevent PCF with good outcomes
Questions?