Corneal biomechanical properties and their association with
advertisement

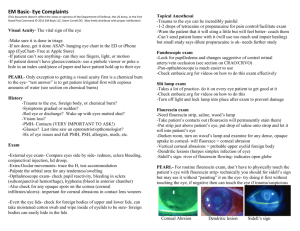
Corneal biomechanical properties and their association with intraocular pressure (IOP) and central corneal thickness (CCT) Dimitrios P. Bessinis1, Pandelis A. Papadopoulos,2,3, Alexandros A. Papadopoulos2, Konstantinos Kakoulidis3 and Andrej Cernak3 1. Department of Ophthalmology, Evaggelismos General Hospital, Athens, Greece 2. Ophthalmo-Check Eye Center, Athens, Greece 3. Department of Ophthalmology, Slovak Medical University, Bratislava, Slovakia the authors declare that they have no financial interest in the products mentioned in the study RATIONALE We hypothesized and investigated the association of intraocular pressure (IOP) and central corneal thickness (CCT) with the biomechanical properties of the cornea, including the applanation lengths, the peak distance and the peak radius of the highest concavity as well as the deformation amplitude. Assesment of biomechanical properties as well as IOP and CCT was made with Corvis ST. Corvis ST is a Non-Contact Tonometer which allows the measurement of IOP and CCT with a high speed Scheimpflug camera (4300 fps) and records the movement reaction to the cornea to an air impulse. MATERIALS AND METHODS Fifty five eyes of 28 patients were examined with Corvis ST for IOP, CCT and biomechanical properties. Statistical analysis was performed with SPSS software for Windows using Spearman’s correlation. The Oculus Corvis ST Datasheet of Corvis ST Still image from the Scheimpflug camera Higher IOP was associated with higher applanation length 2, lower peak distance, higher peak radius and lower deformation amplitude Higher CCT was associated with higher applanation length 2, lower peak distance, higher peak radius and lower deformation amplitude CONCLUSIONS In our investigation a correlation was detected between IOP, CCT and corneal biomechanical properties. It appears that a higher IOP and a thicker cornea results in bigger concavity and rebound of cornea to normal state. On the contrary the peak distance of the highest concavity and the deformation amplitude is lower when IOP and CCT are high. It seems that even though there is an association of IOP and CCT it may not be in the way previously believed. Neither IOP nor CCT interact with applanation length 1, which is the highest deformation length of the cornea immediately after the air impulse. Based on our results we suggest that applanation length 1 may be a key to understanding corneal biomechanics as it is independent of other factors such as IOP and CCT. REFERENCES 1. 2. 3. 4. 5. 6. 7. Ambrosio R, Jr., Nogueira LP, Caldas DL, Fontes BM, Luz A, Cazal JO, Alves MR, Belin MW (Evaluation of corneal shape and biomechanics before LASIK. Int Ophthalmol Clin 51:11-38.2011). Bueno-Gimeno I, Espana-Gregori E, Gene-Sampedro A, Lanzagorta-Aresti A, Pinero-Llorens DP (Relationship among corneal biomechanics, refractive error, and axial length. Optom Vis Sci 91:507-513.2014). Hassan Z, Modis L, Jr., Szalai E, Berta A, Nemeth G (Examination of ocular biomechanics with a new Scheimpflug technology after corneal refractive surgery. Cont Lens Anterior Eye.2014). Koprowski R, Lyssek-Boron A, Nowinska A, Wylegala E, Kasprzak H, Wrobel Z (Selected parameters of the corneal deformation in the Corvis tonometer. Biomed Eng Online 13:55.2014). Lau W, Pye D (Changes in corneal biomechanics and applanation tonometry with induced corneal swelling. Investigative ophthalmology & visual science 52:3207-3214.2011). Roberts CJ, Dupps WJ, Jr. (Biomechanics of corneal ectasia and biomechanical treatments. J Cataract Refract Surg 40:991-998.2014). Valbon BF, Ambrosio R, Jr., Fontes BM, Luz A, Roberts CJ, Alves MR (Ocular Biomechanical Metrics by CorVis ST in Healthy Brazilian Patients. J Refract Surg 30:468-473.2014).