ORAL ANTICOAGULANTS IN
THE 21ST CENTURY: A
PRACTICAL GUIDE TO USING
NEWER AGENTS
Katherine Vogel Anderson, Pharm.D., BCACP
University of Florida Colleges of Pharmacy and Medicine
Disclosures
I have nothing to disclose
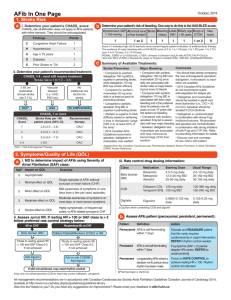
Case
BV is a 75 year old white male who has just been
diagnosed with a. fib. His past medical history is
significant for hypertension (taking chlorthalidone)
and seasonal allergies.
Which oral anticoagulant do you
recommend?
A. Apixaban
B. Dabigatran
C. Rivaroxaban
D. Warfarin
Objectives
Identify new oral anticoagulants (OACs)
Determine the current place in therapy for OACs
Review appropriate transitions between parenteral
anticoagulants and OACs (and vice versa)
Highlight pharmacotherapy scenarios when
changing between OACs
Identify OAC options peri-procedure
A History Lesson…
1930s
heparin
1950s
warfarin
1990s
LMWH
2001
fondaparinux
2010
dabigatran
2011
rivaroxaban
2012
apixaban
2013…
What do I
choose?
*All are FDA approved for stroke prevention
secondary to a. fib
warfarin
rivaroxaban and apixaban
dabigatran
FDA-Approved Doses
Mechanism
Apixaban
Dabigatran
Rivaroxaban
Warfarin
Activated
factor Xa
inhibitor
Direct thrombin
inhbitor
Activated
factor Xa
inhibitor
Vitamin K
antagonist
Dose for stroke
prevention
secondary to
a. fib
5mg twice
daily
150mg twice
daily
20mg once
daily
Renal dose
adjustment
2.5mg twice
daily
75mg twice
daily
15mg once
daily
Dosed to
achieve an
INR between
2 and 3
Not required
Also approved for VTE treatment and prevention
If it isn’t broken, why fix it?
What’s wrong with warfarin?
Monthly monitoring
Drug interactions
Takes lots of time…
New OACs
BUT new OACs…
• Don’t require monitoring
• Fewer interactions
• Quicker onset of action
• Lack antidotes
• Require renal adjustment
• Are expensive
In a nutshell…
Katsnelson M et al. Circulation 2012;125: 1577-1583
A wise man once said…
“Inferiors revolt in order that they may be
equal, and equals that they may be superior.
Such is the state of mind, which creates
revolutions.”
—Aristotle. In: Politics. Book V; Part II; 350 B.C.E.
Nedeltchev K. Stroke 2012;43: 922-923
Back to our case…
Which oral anticoagulant do you
recommend?
A. Apixaban
B. Dabigatran
C. Rivaroxaban
D. Warfarin
Warfarin
Pharmacogenomic dosing?
Regardless – treat to an INR between 2 and 3
You JJ et al. Chest 2012;141(2)(Suppl): e531S-e575S
Coumadin (warfarin) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2011 Oct.
But…
Which oral anticoagulant do you
recommend?
A. Apixaban
B. Dabigatran
C. Rivaroxaban
D. Warfarin
Prodrug?
Yes
Food?
No effect
Drug interactions
P-gp substrate:
Verapamil decrease dabigatran dose
Dronedarone decrease/don’t use
Renal adjustment
CrCL < 30ml/min 75mg twice daily
Pros the oldest of the new
Cons GI intolerance; renal dose not prospectively studied
Heidbuchel H et al. Europace 2013;15: 625-651
But…
Which oral anticoagulant do you
recommend?
A. Apixaban
B. Dabigatran
C. Rivaroxaban
D. Warfarin
Prodrug?
No
Food?
Mandatory
Drug interactions
P-gp AND CYP3A4 substrate:
Amiodarone, diltiazem, verapamil –
caution if CrCL is less than 50ml/min
AVOID with strong inhibitors
Renal adjustment
CrCL 15 – 50ml/min 15mg once daily
Pros once daily dosing; renal adjustments
Cons once daily dosing; food requirement
Heidbuchel H et al. Europace 2013;15: 625-651
But…
Which oral anticoagulant do you
recommend?
A. Apixaban
B. Dabigatran
C. Rivaroxaban
D. Warfarin
Prodrug?
No
Food?
No effect
Drug interactions CYP3A4 substrate:
Reduce dose to 2.5mg/avoid with strong
CYP3A4 and P-gp inhibitors
Renal adjustment If SCr is greater than 1.5mg/dl, patient is
greater than 80 years old, patient weighs
less than 60Kg 2.5mg twice daily
Pros renal dose prospectively studied
Cons twice daily dosing; newest of the new
Heidbuchel H et al. Europace 2013;15: 625-651
Some considerations
Although new OACs are substrates for P-gp and
CYP, they are not inhibitors
PPI use does not have a clinical effect on efficacy
Bleeding risk increases with antiplatelet agents
Compliance is key effectiveness fades fast
12
– 24 hours after last dose = no anticoagulation
The decision is made...
… A new OAC will be prescribed for BV
So – what’s next?
Do we really NOT monitor?
What if BV has a procedure?
What if BV wants to switch to warfarin?
Let’s get started…
Heidbuchel H et al. Europace 2013;15: 625-651
Patient anticoagulation cards: www.noacforaf.eu
PPI: No prospective evidence, but consider a PPI for
high risk patients (i.e. history of GI bleed)
Follow up visits:
Compliance
S/Sx
thromboembolism and/or bleeding
Side effects
Medication reconciliation
Labs: 3, 6, 12 months and as needed
Heidbuchel H et al. Europace 2013;15: 625-651
Coagulation Monitoring
Dabigatran
Apixaban
Rivaroxaban
Plasma peak (after
ingestion)
2 hours
1 – 4 hours
2 – 4 hours
Plasma trough (after
ingestion)
12 – 24 hours
12 – 24 hours
16 – 24 hours
PT
N/A
N/A
Prolonged
INR
Increase
Increase
Increase
aPTT
>2xULN @ trough N/A
suggests risk
N/A
Anti-Xa
N/A
Quantitative
ECT
>3xULN @ trough N/A
suggests risk
Heidbuchel H et al. Europace 2013;15: 625-651
No data YET
N/A
Transitions in Therapy
To a new OAC…
heparin upon discontinuation (~2 hours)
From low molecular weight heparin (LMWH) when
the next dose of LMWH is due
From
From a new OAC…
To
warfarin similar to “bridging”
The
new OAC is taken simultaneously with warfarin until the
INR is within the appropriate therapeutic range
To
LMWH when the next dose of OAC is due
Heidbuchel H et al. Europace 2013;15: 625-651
Transitions in Therapy
From warfarin to a new OAC:
As
soon as the INR is less than 2
If INR is between 2 and 2.5 start the next day
For INR greater than 2.5 It depends
How
high is the INR?
Wait and hold
Draw a new INR
If INR is less than 2.5, proceed as above
Heidbuchel H et al. Europace 2013;15: 625-651
Peri-procedural management of OAC
When do you stop the new OAC?
Evaluate
Patient factors = age, renal
function, history of bleeding
AND
Procedure factors
No bleeding risk
Minor bleeding risk
Major bleeding risk
No need to hold the OAC
Heidbuchel H et al. Europace 2013;15: 625-651
Peri-procedural management of OAC
Hold the OAC 24 hours prior
Hold the OAC 48 hours prior
Resume OAC 6 – 8 hours after the procedure IF immediate and complete
hemostasis is achieved AND re-bleeding risk is minimal.
If invasive procedure, resumption of OAC may be deferred for 48 - 72 hours
Heidbuchel H et al. Europace 2013;15: 625-651
Management of bleeding
Heidbuchel H et al. Europace 2013;15: 625-651
Two Clinical Questions
What about aspirin?
Post-ACS:
ASA
or clopidogrel + new OAC = increased bleeding
apixaban or rivaroxaban may be preferred
Within the first year ASA + decreased OAC dose
After the first year OAC alone
What about valves?
NOT
for valvular atrial fibrillation
NOT for mechanical valve replacement
Heidbuchel H et al. Europace 2013;15: 625-651
Back to our case…
Which oral anticoagulant do you
recommend?
A. Apixaban
B. Dabigatran
C. Rivaroxaban
D. Warfarin
My answer
I’m old school…
But, if pressed to choose a new one….
Thanks for
your
attention!