Strategies for Reversing Anticoagulation
advertisement

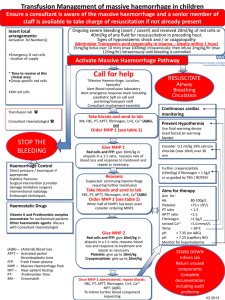
Strategies for Reversing Warfarin Anticoagulation W. Cederquist, MD, Anesthesiology PGY-V Mentor: Paul Picton, MD Case Discussion – Practical Updates in Anesthesiology 2014 Tues, February 4th, 2014 Disclosures • No conflicts of interest to report Case Presentation (1) • HPI: 70 y.o. ASA 3 man presenting to ED with 12 hours of vomiting, loose stools and RLQ abdominal pain. • PMH: HTN and atrial fibrillation on warfarin • VS: T 39°C; BP 108/63; HR 74 regular; RR 16; SpO2 96% RA. • Exam: 72 in, 100kg, BMI 30. Neurologic, HEENT, cardiopulmonary, GU, MSK and skin wnl. Tenderness at McBurney’s point, Rosving’s sign. Case Presentation (2) • Labs: WBC 14.3 (4-10 K/mm3) 80% PMNs Hct 46.8 (40-50 %) Plt 173 (150-400 K/mm3) COMP Within normal limits aPTT 31.6 (22.0-32.0 s) PT 28.4 (9.8-12.5 s) INR 2.8 Case Presentation (3) • CT abdomen/pelvis with IV/PO contrast • Surgical plan: Laparoscopic appendectomy Case Presentation (4) Surgery Note: “The patient will be transfused 3 units of FFP to correct his INR to less than 1.5. The patient will have immediate INR check and will be continued to be transfused with FFP should he remain therapeutic... Once his INR is reversed, the patient will be taken to the operating room...” Perioperative Course (1) 1349 1425 1624 1745 2040 2125 2136 2212 2230 0146 0200 0300 Arrival to ED INR 2.8 CT abdomen/pelvis Ciprofloxacin/Metronidazole Administered 1st FFP 2nd FFP Arrived in Pre-Op Area INR 2.2 3rd FFP and 4th FFP INR 1.7 5th FFP Facial edema and urticaria noted Perioperative Course (2) 0412 0421 0431 0502 0545 0611 0845 0851 0858 0901 0942 1325 Patient In Room Anesthesia Induction End Urology Consult for Difficult Foley Placement Surgical Incision Converted to Open Ileocecetomy INR 1.7 EBL 300cc Surgical Dressing Complete Extubated Awake Transported to PACU INR 1.8 Admitted to Surgical Ward Perioperative Course (3) • Post Op Course - complicated by paroxysmal atrial fibrillation • Outcome - warfarin restarted at discharge to home on postoperative day #4 Goals and Objectives • Identify the hemostatic defect in warfarin therapy • Evaluate the safety and efficacy of three methods to correct warfarin anticoagulation • Critically appraise the association between an elevated prothrombin time and bleeding risk • Introduce prothrombin complex concentrate as an alternative to FFP for warfarin reversal Classical Coagulation Pathway aPTT PT/INR Differential Diagnosis Anticoagulants warfarin, argatroban, heparin Liver disease multiple etiologies Vitamin K deficiency malnutrition, antibiotic use Factor deficiency hemophilia, autoimmune disease, coagulation factor inhibitors Warfarin Factors II VII IX X ACCP Guidelines 8th Edition (2008) Coagulation Factor Activity vs INR Gulati et al. Archives of Pathology & Laboratory Medicine ( 2011) Classical Coagulation Pathway Question • What three general strategies are available for the correction of warfarin-induced coagulopathy? - discontinue warfarin (days) - supplement vitamin K (12 - 24 hours) - replace clotting factors (immediate) Vitamin K Supplementation Phytonadione ACCP Guidelines 8th Ed Intravenous Vitamin K - 178 patients on warfarin - vitamin K 3 mg IV - PT/PTT checked on day of procedure Burbury et al. Br J Haematology (2011) Intravenous Vitamin K Normal Range Burbury et al. Br J Haematology (2011) Added to Chest Guidelines Recommendations: “Anticoagulation reversal for non-major bleeding should be with 1-3 mg intravenous vitamin K (Grade 1B).” Question • What three general strategies are available for the correction of warfarin-induced coagulopathy? - discontinue warfarin (days) - supplement vitamin K (12 - 24 hours) - replace clotting factors (immediate) Replacement of clotting factors Blood Product (FFP) Multiple factor replacement (Prothrombin Complex Concentrate) Single factor replacement (Recombinant Factor VIIa) What’s in it? Stanworth. Hematology (2007) Professional Guidelines • ASA Practice Guideline for Perioperative Blood Transfusion (2006): “FFP should be given … to achieve a minimum of 30% plasma factor concentration (usually achieved with administration of 10-15 ml/kg FFP), except for urgent reversal of warfarin anticoagulation, for which 5-8 ml/kg FFP usually will suffice.” American Society of Anesthesiology. Anesthesiology (2006) Making Assumptions Surgery Note: “The patient will be transfused 3 units of FFP to correct his INR to less than 1.5…and will be continued to be transfused with FFP should he remain therapeutic... ” Assumptions: 1) FFP will decrease the bleeding risk Will FFP decrease the bleeding risk? - review of FFP - multiple clinical endpoints - evidence supporting FFP is weak Stanworth. Hematology (2007) Making Assumptions Surgery Note: “The patient will be transfused 3 units of FFP to correct his INR to less than 1.5…and will be continued to be transfused with FFP should he remain therapeutic... ” Assumptions: 1) FFP will decrease the bleeding risk 2) FFP will correct the INR to < 1.5 Change in INR per unit FFP Holland LL, Brooks JP. Am J Clin Path (2006) Will FFP decrease the INR to 1.5? Starting INR 1.5-1.8 Median INR change = 0.07 Less than 1% achieve normalization of the INR. Abdel-Wahab et al. Transfusion (2006). Where did that number come from? Where did that number come from? Holland LL, Brooks JP. Am J Clin Path (2006) Replacement of clotting factors Blood Product (FFP, whole blood) Multiple factor replacement (Prothrombin Complex Concentrate) Single factor replacement (Recombinant Factor VIIa) Prothrombin Complex Concentrate PCC II VII IX Hemophilia B X How is it made? Ion exchange chromatography II VII IX X Adult dose: 25-50 U/kg Pasteurize Effect of PCC on clotting factors Pabinger et al. J. Thromb Haemost (2008). PCC vs FFP PCC FFP Onset immediate limited by acquisition time and infusion rate Duration ~ 3-6 hours ~ 3-6 hours Volume ↓↓↓ ↑↑↑ Risks thrombosis allergic rxn, TRALI, TACO, infection Cost +++ + Added to Chest Guidelines Recommendation: “For patients with warfarinassociated major bleeding, we suggest rapid reversal of anticoagulation with four-factor PCC rather than with plasma (Grade 2C).” ACCP Guidelines 9th Edition (2012) Coming soon to a pharmacy near you PCC II IX X PCC 3 factor PCC II IX X 3 factor PCC Clinical Trials - 202 patients taking warfarin - equal in terms of “effective hemostasis” - possibly fewer adverse events Sarode et al. Circulation (2013) New Oral Anticoagulants - direct thrombin inhibitors (dabigatran) - factor Xa inhibitors (-xabans) - consider PCC if all else fails Heidbuchel et al. Europace (2013) Conclusions • Identify the hemostatic defect in the coagulopathic patient presenting for emergency surgery. • Use vitamin K for procedures that can be delayed 12 hours, otherwise use FFP. • Minor elevations in INR are unlikely to be corrected by plasma transfusion. • Prothrombin complex concentrate is a promising alternative but further studies are needed.