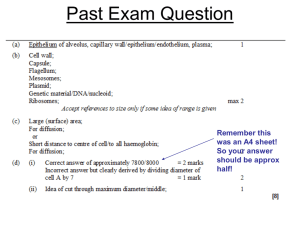
Comorbidities in
Rheumatoid Arthritis
Dr Barb Blumenauer MD FRCPC
Comorbidity Associated With RA
•
Comorbidity in RA can be due to the disease, due to its treatment or
due to lack of exercise, increased incidence of smoking etc
•
RA increases standardized mortality rates(SMR) 50-60% compared
to age and sex matched general population.
•
RA patients tend to die prematurely and estimates range from 7-20
years
•
Disease control may impact survival although SMR haven't changed
with advances in treatment but this may reflect the increased life
expectancy of the population as a whole
•
Methotrexate has been shown to decrease mortality and there is
evidence as well for anti-TNF therapy
Mortality
•
Most of excess mortality due to premature cardiovascular deaths
•
Higher incidence of smoking in RA patients versus general
population which could impact survival
•
RA patients often less physically active
•
Prednisone has been shown to increase risk of CVD and increases
with increasing daily dose and total cumulative dose.
Cardiovascular Comorbidity in
RA
•
RA patients have increased incidence of MI and this is present even
before onset and diagnosis of RA
•
RA patients less likely to survive MI with increased mortality in the
first 30 days post MI
•
Standard CV risk assessment such as Framingham underestimates
the risk.
•
No clear tool to estimate risk but many feel RA should be stratified
and treated as per a diabetic
•
Some evidence multiplying Framingham by a factor of 1.4-1.6 gives
better estimate
Cardiovascular Disease in RA
•
RA patients may get more small vessel disease not surgically
treatable
•
NSAIDS causing even 4-5 mm Hg elevation in blood pressure can
increase MI risk as shown in Vioxx clinical trials
•
RA patients are used to pain and may mistake chest pain due to MI
as being MSK in origin and not seek or delay in seeking treatment
and vice-versa ER personnel may make same mistake
•
Target LDL 1.9 or less in RA patients
•
Tight BP control as well
Neurologic Disease in RA
•
Increased incidence of CVA in RA patients
•
Rarely peripheral neuropathy
•
Arava and Plaquenil rarely cause neuropathy
Infection in RA
•
Some treatments may increase risk of infection however RA is an
independent risk for infection
•
Infection risk higher with longer disease duration or increased
disease activity
•
Although some drugs may increase risk of infection BC data ( Dr
Diane Lacaille) shows that treatment of RA with DMARDs actually
reduces risk of infection compared to RA patients not on treatment
•
•
Prednisone significantly increases infection risk
Biologics may increase infection but generally patients who make it
through the first 3 months without infection don't have increased
risk thereafter
Infection in RA
•
Increased risk of lung ( may be due to smoking, interstitial lung
disease)
•
Also increased risk of skin and joint infection
•
Joint infections occur in native and artificial joints
•
Beware a disconcordant joint it may be infected rather than a flare
•
To reduce infection stop smoking, ensure vaccinations including
influenza, pneumovax and Twinrix UTD, reduce/avoid PDZ, control
disease activity
•
Consider shingles vaccination before DMARDs beyond Plaquenil and
sulfasalazine are started
Infection in RA
•
Beware TB reactivation as patients immunocompromise may be due to
effects of treatment or RA
•
PPD may be falsely negative when RA disease activity high
•
If PPD 5 or more need prophylactic treatment to use biologic therapy
•
Be on the look out for atypical infections including MAIC – I have had 3
patients within a year
•
Snowbirds ( does half of everybody else's practice run away for the
winter?) often in areas where histoplasmosis and coccidiomycosis
endemic and they may not present in a typical fashion
•
Leukopenia or neutropenia common which could increase infection (
Felty's syndrome etc.)
Lymphoproliferative Disease
•
Leukemia and lymphoma rates about double those of general
population
•
Methotrexate, Imuran and anti-TNF agents increase risk of
lymphoma as does longer RA duration and increased disease activity
•
Smoking increase lymphoma risk as well
Malignancy in RA
•
Aside from lymphoma and leukemia also increased risk of lung
cancer and skin cancers in RA
•
Patients should practice safe sun and check skin regularly for any
abnormalities
•
Literature supports lower incidence of colon CA which may be
secondary to NSAIDs – will colon CA rates rise with more judicious
use of NSAIDS with CVD risk concerns?
•
Anti-TNF agents may slightly increase risk of lymphomas and skin
cancers and ?lung CA(data contradictory) but appear to decrease
risk of colon and breast cancer
Lung Disease in RA
•
RA patients at increased risk of lung disease and it is often
subclinical
•
Likely increases risk of pulmonary infection
•
May be secondary to drugs such as methotrexate, Arava, gold
•
Patients with ILD have increased mortality
•
Registry data suggests doubling of mortality rate in RA patients with
ILD who take anti-TNF agents
C1-C2 Subluxation
•
Synovitis can lead to instability but usually in long standing disease
•
Patients with symptoms or after 10 or so years of disease should be
screened periodically and pre-operatively with cervical flexion and
extension views to exclude significant subluxation
•
Usually if greater than 8 -10 mm surgical fixation required
•
NEVER passively flex a rheumatoid neck because if they have this
you can compromise the cord and paralyze or kill them
•
RA patients shouldn't have neck manipulation from ANY
practitioner and need to be specifically advised chiropractic neck
manipulation could be unsafe
Ocular Comorbidities
•
Episcleritis and scleritis most common eye involvement but rare with
advent of better treatment
•
Can lead to ocular perforation if not controlled
•
Watch for glaucoma if on high dose prednisone
•
Cataracts with PDZ
Osteoporosis
•
RA independent risk factor for OP
•
RA Automatically moves patient up one risk category for fracture
•
Prednisone also automatically increases risk one category i.e. low,
medium or high risk for fracture
•
Therefore RA patient on PDZ high risk for fracture regardless of
BMD values
•
Reduce/avoid PDZ, stop smoking and increase activity to reduce risk
of OP
•
Start OP prophylaxis if you start PDZ unless certain it will be a
short course except in women of child bearing potential due to
concern about fetal bone malformation in subsequent pregnancy
Depression
•
RA patients have a higher incidence of depression and this can be
compounded by dugs such as Prednisone
•
Many depressed patients feel it is the RA that is the problem but
treating RA often improves function, pain and quality of life
Rare RA Comorbidities
•
Vasculitis rare in RA but occurs and sometimes in association with
methotrexate
•
Renal disease rare from an RA perspective but chronic NSAIDS can
cause issues as can gold and cyclosporine.
Conclusions
•
RA is associated with significant co morbidities than can reflect
disease severity, duration or treatment
•
Generally controlling disease activity can reduce some of these issues
•
Stratifying CV risk problematic with the tools available currently
but they are high risk and should be treated as such due to their
excess death from CV disease and increased rates of premature
death
•
Patients should quit smoking
•
Avoid/reduce PDZ
•
Methotrexate confers a survival advantage ( less dead is almost
always better than more dead)
Conclusions
•
Ensure immunizations are UTD but live vaccines contradicted with
most DMARD agents
•
Promote fitness ( RA FIT website great)
•
Maintain ideal body weight- being obese is a pro-inflammatory state
•
Be vigilant about BP control
•
Watch for infections including atypical ones
•
Diagnose RA early and control disease to give patient best chance to
avoid comorbidities!