Urology
advertisement

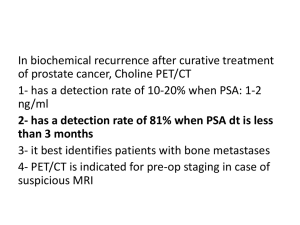
CCG/QEH Urology Agreements An update for General Practitioners -Edgar Paez-Consultant Urologist -Freeman Hospital –Newcastle upon Tyne and Queen Elizabeth Hospital-Gateshead July 2014 CCG/QE Agreement-Proposed Pathways • • • • Review of agreements due Recent NICE guidance New commissioning guidance Initiate first line assessment/treatment in primary care • Attempt to reduce “un-necessary” secondary care referral • Reduce cost of treatment Suspected cancer referral • Prostate • Bladder and renal -Haematuria SUSPECTED CANCER-PROSTATE • Men presenting with symptoms suggesting prostate cancer should have a digital rectal examination (DRE) and prostate-specific antigen (PSA) test after counselling. • Urinary tract infection (UTI) should be excluded before PSA testing. If there is a proven UTI, the PSA test should be postponed for at least 1 month ( ideally 6-8 weeks)after treatment of the infection. Urgent referral should be made: • If a hard, irregular prostate is felt on DRE. PSA should be measured and the results sent with the referral letter. Urgent referral is not indicated if the prostate is enlarged and the PSA is normal. • If the prostate is normal on DRE, but the agespecific PSA is raised or rising. • In symptomatic men with high PSA levels. If there is doubt about whether to refer an asymptomatic man with borderline level of PSA, PSA test should be repeated after 1 to 3 months. If the second test indicates that the PSA level is rising, an urgent referral should be made. • The age-specific cut-off PSA measurements recommended by the Prostate Cancer Risk Management Programme are as follows: • 50–59 years of age >= 3.0 nanograms/mL; • 60–69 years of age >= 4.0 nanograms/mL; • 70 years of age and older >= 5.0 nanograms/mL. (there are no age-specific reference ranges for men over 80 years of age. Prostate cancer only needs to be diagnosed in this age group if it is likely to need palliative treatment, i.e grossly abnormal DRE, suspicion of advanced disease, PSA >20. • Good performance status, life expectancy 10 years. • Screening in patients over 75 is discouraged. SUSPECTED CANCER-RENAL AND BLADDER/Haematuria clinic • Any adult patient with visible haematuriacheck for UTI-haematuria clinic. Men 50-75 with no UTI : PSA. • Over 40’s with persistent non visible haematuria-haematuria clinic • Patients under 40 with persistent non visible haematuria-check creatinine and proteinuria, if abnormal, refer to Nephrology, if normal, non urgent referral to Urology Haematuria Clinic • 2 stop clinic • Radiology (USS + KUB in all non visible haematuria and younger patients, CTIVU in over 40’s with visible haematuria)performed first stop • Flexible cystoscopy 2nd stop • Report sent to GP’s from clinic. • Please perform eGFR Shared Care Prostate Cancer Introduction • Patient with diagnosis of prostate cancer • On A/M, hormonal manipulation or post radical treatment (surgery or radiotherapy). • Care closer to home • Reduce number of hospital appointments • No compromise in patient care • Financial implications • Hospital Doctors/Patients/GP’s have to agree. Will require written response by GP’s. • Clear treatment plans • General guidelines + individual patients letters • Review compliance to be monitored by CCG. Ca.Prostate. Shared care discharge guidelines Patient type Discharge criteria Discharge after Hormone Therapy Stable * 1 year Watchful wait No sign of disease progressions and stable* 1 year Active surveillance (suitable for radical treatments) No sign of disease progressions and stable* 2 years ( only when no longer suitable for radical treatment) Active surveillance (not suitable for radical treatments) Stable* 1 year Low risk post radical surgery Undetectable PSA, stable LUTS and DRE* 2 years High risk post radical surgery Undetectable PSA, stable LUTS and DRE* 5 years Low risk post radiotherapy Stable* 2 years following completion of hormones High risk post radiotherapy Stable* 5 years *STABLE = No increase in LUTS, No changes in DRE & stable PSA Shared care-follow up • Patients on hormonal manipulation: PSA alone, DRE if changes on PSA or LUTS that need further assessment. Check liver function twice a year, testosterone if PSA ↑, to assure castrate levels. • Patients post radical radiotherapy: : PSA alone, DRE if changes on PSA or LUTS that need further assessment. • Patients post radical prostatectomy: PSA alone, no role for DRE. • Patients on active monitoring: PSA and yearly DRE. When to refer back-following radical treatment. • After radical prostatectomy: a confirmed PSA value >0.2 (two consecutive measurements) • After radiotherapy: a confirmed PSA value 2ng/ml above nadir value • If patients have significant urological side effects following therapy. When to refer back-patients on active monitoring • Letter generated on each patient with recommendation • Most patients who are discharged will be not suitable for radical treatment (in view of age, comorbidities, etc) • For most patients will be signs of significant disease progression (3 significant PSA rises, PSA doubling time <6months, PSA>20, or symptoms of advanced disease). Patients with elevated PSA and negative prostate biopsy • Patients will be discharged after investigated • Physicians satisfied that significant prostate cancer unlikely (repeat biopsies/MRI will be performed if indicated). • Currently no national guideline by NICE-issue under review • Decision aid tools being developed Shared care-delivery improvement • Pilot with a handful of Practices to send current forms via NHS Mail instead of post. • Working with CBC to pilot use of EMISWeb to track current Shared Care patients including a reminder system that will flag when patients are due a review appointment. Will look to run as part of EMIS QOF Template pilot being run by CBC with Practices in the Bureau. Erectile dysfunction As per Newcastle, North of Tyne and Gateshead guidelines for management of erectile dysfunction on adults > 18 years. Assessment History – medical, sexual and psychosocial. Smoking drugs and alcohol. Determine type of ED. Examination – BP and BMI. Secondary sexual characteristics abdominal and genitalia, Lower limb pulses Bloods Calculate CV risk IIEF questionnaire. Erectile Dysfunction Referral to secondary care as per CCG Guidelines for management of erectile dysfunction Trial of treatment in primary care . Lifestyle change Manage any underlying cause Treatment if no contra-indications If appropriate – instruct patient in use, possible side effects First line PDE5i is SILDENAFIL 50 – 100mgs trial of no less than 8 tablets. Second line - Tadalafil 20 mgs if no response to Sildenafil – no less than 8 tablets. Vardenafil 10 -20mgs (private prescription only not on formulary) Daily Tadalafil 5mgs (private prescription only not on formulary): consider in men with LUTS due to BPE Refer to secondary care if above treatment fails. Patients will be seen in secondary care until patient is established on successful treatment, then GP to continue prescribing/review. Prescribing as per schedule 2. Referrals that do not meet the CCG guidelines will be rejected. Lower urinary tract symptoms LUTS • Follow NICE guidance before referral • Initial assessment/management in community-if no evidence of this happening, referrals could be rejected or treated as advice and guidance. • Normal PSA patients discharged once stable on treatment • Patients with LUTS and raised PSA discharged after successful treatment for LUTS and biopsies dealt with. LUTS-initial assessment • History-general and urological. • Physical examination guided by symptoms and other medical conditions, an examination of the abdomen and external genitalia, and a digital rectal examination (DRE). • urine dipstick test. • Frequency volume chart and IPSS. • Discuss PSA if indicated. LUTS-initial management • Storage symptoms (OAB): lifestyle changes, fluid intake advice (caffeine, alcohol), bladder training. • Voiding symptoms: likely bladder outflow obstruction. If mild active surveillance. If moderate or severe consider drug therapy. LUTS-drug therapy options LUTS-when to refer • Patient with uncomplicated LUTS should receive first line treatment in the community and should be referred to urology if: • LUTS not responded to conservative management or drug treatment • They have: – LUTS complicated by recurrent or persistent UTI – retention – renal impairment you suspect is caused by lower urinary tract dysfunction – suspected urological cancer – stress urinary incontinence. Advice and Guidance Service • Patients who might not need to be seen in clinic but need advice on management • Avoid “unnecessary” appointment • As much info as possible • E-mail service. Forwarded to consultant • Reply within few working days Thank you Questions/comments?