Part2LECTURE
advertisement

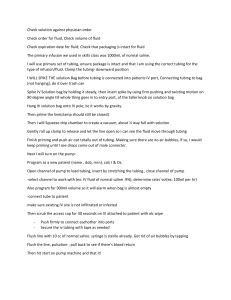
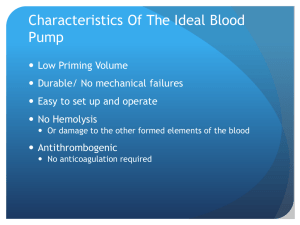
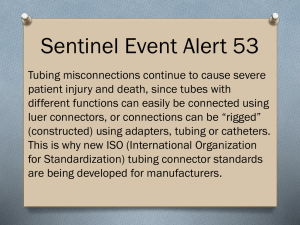
Catherine Luksic BSN, RN Primary infusion “maintenance infusion” “continuous infusion” Via gravity Via electronic pump Secondary infusion “piggyback” “IVPB” Usually via electronic pump Primary IV administration set Gravity infusion Electronic pump infusion Secondary IV administration set “piggyback tubing” Blood administration Y set Extension tubing Intermittent infusion lock HL or SL Gravity Drip Manually set, regulated w/ roller clamp Simplest method Count drops manually Macrodrip tubing - drop factor determined by manufacturer Can range from 10-20 gtts/mL (common 10gtts/mL) standard primary tubing for rapid infusions Microdrip tubing - 60gtts/mL Used for peds, elderly, slower rates Advantages: Easy Does not require power source or pump Can set-up quickly Disadvantages: Not greatly accurate No free-flow prevention Room for error Volume ordered to be infused 1000 ml or 1000 cc Drop factor of tubing being used Rate of infusion as per order 100 ml /hr (or 100 cc/hr) **refer to IV calculations worksheets Check physician orders ! Gravity drip or electronic pump ? cc/hr = ml/hr KVO (10-20 ml/hr) TKO Check IV site & IV rate at least every hour Refer to procedure Maintain sterility Remember to close the roller clamp 1st ** ?? Invert all Y-sites and tap to remove air Demonstration Practice Height of bag 36 inches above heart Position of roller clamp is it open or closed ? Patency of tubing Check for kinks Check rate - has it been changed? Check tubing - is it kinked? Check clamp(s) - are they open? Check site is cath or vein being compressed? ANY abnormality? Look for sign of infiltration Purpose Requires Deliver – improve accuracy of delivery. power source a preset fluid rate over a specified period Uses constant force Always use pump w/ TPN, central lines, titrated medications, blood products Occlusion Air-in line Infusion complete Power SINGLE CHANNEL MULTI-CHANNEL PCA (Patient controlled analgesia) AMBULATORY IV PUMPS Home care use ASSESSMENT DIAGNOSIS PLANNING IMPLEMENTATION EVALUATION FIRST STEP, AS ALWAYS chronic conditions use of long-term medications (anticoagulants) previous IV experiences/problems allergies (especially latex & antimicrobial agents) hand dominance Skin *Cultural considerations, communication barriers, level of understanding Physical exam Neurological status – AAO, ability to understand and cooperate Cardiovascular status – color, pulses, edema, appearance of veins Skin – bruising, rashes, lesions Examples: Risk for injury related to (lack of knowledge regarding equipment) Knowledge deficit related to (new IV insertion) AEB (pt verbalization …) Impaired physical mobility related to placement of peripheral IV AEB… Anxiety related to (initiation of IV therapy) AEB... Alteration in comfort: Pain Patient outcomes and goals - what do you (and the patient!) expect. Ex: Pt. will remain free of S/S of complications related to IV therapy More specific – Pt. will remain free of signs of phlebitis Nursing Care: Check site HOURLY for complications - redness, pain, edema, infiltration Instruct pt. to call nurse immediately: pain, bleeding, other concerns. Instruct pt. to call nurse if pump alarm sounds. Maintain correct infusion rate as ordered. Secure IV (to prevent accidental dislodging of catheter during movement). Change tubing according to hospital policy (usually q 72 hr.) Change IV site according to hospital policy (usually q 72 hrs.) Nursing Care: 2011 Infusion Nurse Society (recommendations) Do not change IV tubing more frequently than q 96 hrs. If IVPB tubing is detached from continuous tubing, change q 24 hrs. How will you know if the goal/outcome has been achieved? Assessment Patient record Lab values Communication