Autonomic Nervous System
advertisement

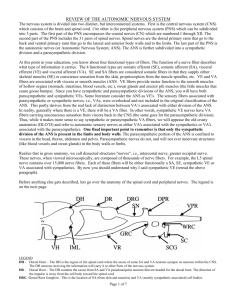
AUTONOMIC NERVOUS SYSTEM Dr. Ayisha Qureshi Assistant Professor, MBBS, MPhil DIVISIONS OF THE PERIPHERAL NERVOUS SYSTEM DIFFERENTIATING BETWEEN THE SOMATIC & AUTONOMIC NERVOUS SYSTEM SOMATIC NERVOUS SYSTEM AUTONOMIC NERVOUS SYSTEM Somatic senses & special senses Mostly interoceptors; some somatic senses & special senses CONTROL OF cortex, basal ganglia, MOTOR OUTPUT cerebellum, spinal cord. Voluntary control; cerebral Involuntary control; hypothalamus, limbic system, brainstem. Limited control from cerebral cortex. MOTOR NEURON One-neuron pathway, PATHWAY Two-neuron pathway. SENSORY INPUT NEUROTRANSMI All Somatic neurons secrete Ach. All preganglionic fibers release Ach. Postganglionic fibers release TTERS & different NT in case of Sym. & Paras. HORMONES EFFECTORS Skeletal muscles. Smooth muscles, cardiac muscles, and glands. RESPONSES Contraction of skeletal muscle. Contraction or relaxation of smooth muscle; Increased or decreased strength of contraction of cardiac muscle; increased or decreased secretion of the glands. Type of nerve fibers α-motor neuron is large diameter, & rapidly conducting Preganglionic fibers: B fibers Postganglionic fibers: C fibers Somatic & Autonomic nervous system The autonomic nervous system is the part of the peripheral nervous system that is responsible for regulating involuntary body functions, such as heartbeat, blood flow, breathing and digestion. AUTONOMIC NERVOUS SYSTEM Divisions of ANS SYMPATHETIC NERVOUS SYSTEM/ Thoracolumbar Division • Fight, flight or Fright. • Activated during exercise, excitement and emergencies. PARASYMPATHETIC NERVOUS SYSTEM/ Craniosacral Division • Rest and Digest. • Concerned with conserving energy. ANS Sympathetic Nervous System Preganglionic Fibers Postganglionic Fibers Parasympathetic Nervous System Preganglionic Fibers Postganglionic Fibers Characteristics of ANS • Nerve fibers: Both divisions have pre- & postganglionic fibers. - Preganglionic neuron is myelinated. - Postganglionic neuron is unmyelinated. (In contrast to the large diameter and rapidly conducting α -motor neurons, preganglionic axons are small-diameter, myelinated, relatively slowly conducting B fibers.) (The axons of the postganglionic neurons are mostly unmyelinated C fibers and terminate on the visceral effectors.) • Neurotransmitters: Autonomic nerves release NT that may be excitatory or inhibitory. • Divergence: Preganglionic fibers branch to synapse with an average of 8-9 postganglionic neurons. • Convergence: Postganglionic neuron receives synaptic input from a large number of preganglionic fibers. Divisions of the ANS • Fight or Flight Response • Thoracolumbar Division • Shows mass activation THE SYMPATHETIC SYSTEM The Sympathetic System Outflow Sympathetic Chain Ganglion Paravertebral Ganglia Prevertebral Ganglia • Most of the sympathetic ganglia lie close to the spinal cord and form the two chains of ganglia, linked by short nerves —one on each side of the cord—known as the Sympathetic Trunks. • Because the ganglia lie close to the spinal cord, thus, the preganglionic neurons are short while the postganglionic neurons reaching the target organs are very long. • Joined to ventral rami by white and gray rami communicans. • In contrast, the parasympathetic ganglia lie within or very close to the organs innervated and ,thus, have very short preganglionic and long postganglionic neurons. • Also called the Collateral ganglia. • Unpaired, not segmentally arranged. • Occur only in abdomen and pelvis, closer to the innervated organ. • Lie anterior to the vertebral column. • Main ganglia: See Next slide for figure – Celiac, superior mesenteric, inferior mesenteric, inferior hypogastric ganglia. See Next slide for figure The Sympathetic System Outflow Myelinated preganglionic fibers exit spinal cord in ventral roots from T1 to L2 levels. They exit from the Lateral horn of the spinal cord. Most sympathetic nerve fibers separate from somatic motor fibers and synapse with postganglionic neurons within paravertebral ganglia. Ganglia within each row are interconnected, forming a chain of ganglia that parallels spinal cord to synapse with postganglionic neurons. Sympathetic System Outflow Termination of Sympathetic Preganglionic Fibers Termination of Sympathetic Postganglionic fibers 1. • Axons leave the chain ganglia and re-enter the spinal nerves via gray rami communicans to reach the: 1. Visceral targets 2. Smooth muscles 3. Sweat glands 2. 3. 4. Postganglionic fibers in the paravertebral ganglion of the same segment. Postganglionic fibers of the paravertebral ganglion of an upper or lower segment. Pass thru the paravertebral ganglion chain & end on postganglionic neurons in prevertebral ganglion close to the viscera (celiac, superior and inferior mesenteric ganglion). Adrenal Medulla. Sympathetic System Outflow To the Periphery To the Head Sympathetic System Outflow To the Thoracic regions To the Abdominal Organs The Adrenal Gland • The Adrenal gland is the major organ of the sympathetic nervous system. • When stimulated, the adrenal medulla secretes large quantities of epinephrine and a little norepinephrine directly into the blood stream. Sympathoadrenal system: • Stimulated by mass activation of the sympathetic nervous system. • Innervated by preganglionic sympathetic fibers. • Rest or Digest • Craniosacral Division • Shows stimulation of separate parasympathetic nerves THE PARASYMPATHETIC SYSTEM The Parasympathetic Division • Preganglionic fibers are located in several cranial nerve nuclei (III, VII, IX and X) and in the IML column of the sacral spinal cord (2-4 sacral segments). • Preganglionic fibers synapse in terminal ganglia located next to or within organs innervated. • Thus, the parasympathetic preganglionic fibers are longer while the parasympathetic postganglionic fibers are short. • Most parasympathetic fibers do not travel with the spinal nerves. • Do not innervate blood vessels, sweat glands, and arrector pili muscles. PARASYMPATHETIC DIVISION (Cranial Outflow) 1. Cranial Nerve III- Occulomotor Nerve 2. Cranial Nerve VII Facial Nerve 3. 4. Cranial Nerve IX Cranial Nerve X GlossoPharyngeal Nerve Vagus Neve Parasympathetic Division (continued) • 4 of the 12 pairs of cranial nerves (III, VII, X, XI) contain preganglionic parasympathetic fibers. • III, VII, XI synapse in ganglia located in the head. • X synapses in terminal ganglia located in widespread regions of the body. • Vagus (X): – Innervates heart, lungs, esophagus, stomach, pancreas, liver, small intestine and upper half of the large intestine. • Preganglionic fibers from the sacral level innervate the lower half of large intestine, the rectum, urinary and reproductive systems. There are 3 main types of neurotransmitters used extensively in ANS: 1. Acetylcholine 2. Norepinephrine 3. Epinephrine CHEMICAL TRANSMISSION AT AUTONOMIC JUNCTIONS NEUROEFFECTOR JUNCTION • The synapse between an autonomic postganglionic neuron and its target cell is called a Neuroeffector Junction. • The postganglionic axons end in nerve terminals that show swellings called “varicosities” that consist of vesicles containing the Neurotransmitters. • The diffuse release of NT means that a single postganglionic neuron can affect a large area of target tissue. • Acetylcholine is the neurotransmitter released by all neurons whose axons exit the CNS, including cranial motor neurons, α-motor neurons, γmotor neurons, preganglionic sympathetic neurons and preganglionic parasympathetic neurons. • Postganglionic parasympathetic neurons also release Ach, whereas postganglionic sympathetic neurons release either Norepinephrine or Ach. • Ach is degraded by Acetylcholinesterase. • Norepinephrine is degraded by monoamine oxidase. Neurotransmitters in ANS CHOLINERGIC RECEPTORS ADRENERGIC RECEPTORS The principal transmitter is ACETYLCHOLINE and include: 1. All preganglionic neurons. 2. All parasympathetic postganglionic neurons. 3. Sympathetic postganglionic neurons that innervate sweat glands. 4. Sympathetic postganglionic neurons that end on blood vessels in skeletal muscles. The Cholinergic receptors are further subdivided into: • Nicotinic Cholinergic receptors. • Muscarinic Cholinergic receptors. The principal transmitter is EPINEPHRINE & NOREPINEPHRINE and include: 1. All remaining sympathetic postganglionic neurons. 2. The adrenal medulla is essentially a sympathetic ganglion & secretes NE and Epinephrine directly into the blood stream. The Adrenergic receptors are further subdivided into: • Alpha receptors (α1 and α2) • Beta receptors (β1, β2 and β3) Responses to Cholinergic Stimulation (continued) Other Autonomic Neurotransmitters • Certain noradrenergic, norcholinergic postganglionic autonomic axons produce their effects through other NTs. These include: – Adenosine triphosphate (ATP). – Vasoactive Intestinal peptide (VIP). – Nitric Oxide (NO). – Neuropeptide Y (NPY) COMPARISON OF SYMPATHETIC & PARASYMPATHETIC NERVOUS SYSTEM RESPONSES OF EFFECTOR ORGANS TO AUTONOMIC NERVE IMPULSES Organs With Dual Innervation • Most visceral organs receive dual innervation (innervation by both sympathetic and parasympathetic fibers). • Antagonistic effects: – Sympathetic and parasympathetic fibers innervate the same cells. • Actions counteract each other. – Heart rate. • Complementary: – Sympathetic and parasympathetic stimulation produces similar effects. • Salivary gland secretion. • Cooperative: – Sympathetic and parasympathetic stimulation produce different effects that work together to produce desired effect. • Micturition. Organs Without Dual Innervation • Regulation achieved by increasing or decreasing firing rate. • Adrenal medulla, arrector pili muscle, sweat glands, and most blood vessels receive only sympathetic innervation. – Nonshivering thermogenesis. Control of the ANS by Higher Brain Centers • Sensory input transmitted to brain centers that integrate information. • Can modify activity of preganglionic autonomic neurons. • Medulla: – Most directly controls activity of autonomic system. – Location of centers for control of cardiovascular, pulmonary, urinary, reproductive and digestive systems. • Hypothalamus: – Regulates medulla. • Cerebral cortex and limbic system: – Responsible for visceral responses that are characteristic of emotional states. DISORDERS OF ANS HORNER’S SYNDROME Horner syndrome is a rare disorder resulting from interruption of preganglionic or postganglionic sympathetic innervation to the face. CAUSE: • Injury to the nerves. • Injury to the carotid artery. • A stroke • Lesion in the brain SYMPTOMS: The hallmark of Horner’s syndrome is the TRIAD of: 1. Anhidrosis (reduced sweating) 2. Ptosis (drooping eyelids) 3. Miosis (constricted pupil) Symptoms may also include Enophthalmos (sunken eyes) and vasodilation. Raynaud’s Phenomenon Raynaud’s Phenomenon refers to an episodic reduction in blood flow primarily to the fingers, often during exposure to cold or during a stressful condition. CAUSE: It is a vasospastic disorder. There can be many causes: • Exaggeration of response to cold, temperature or stress. • Secondary to another disorder as Rheumatoid arthritis, Sjogren’s syndrome, carpal tunnel syndrome, anorexia. SYMPTOMS: 1. Triphasic color change in the fingers from white to cyanotic blue to deep red. 2. When there is vasospasm, the fingers are pale and cold; then due to reduced blood flow, the color turns blue and there is intense pain; and finally, once blood flow recovers, there is tingling and swelling.