UK Fungal Burden Poster
advertisement

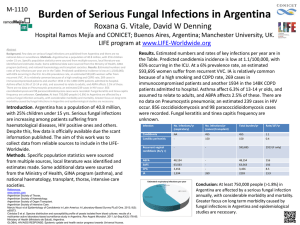
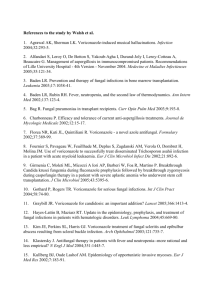
The burden of invasive and serious fungal disease in the UK 1 DW , 2 M, 2,3 W Denning Pegorie Welfare 24th European Congress of Clinical Microbiology and Infectious Diseases in Barcelona, Spain, May 2014 1 National Aspergillosis Centre, University Hospital of South Manchester and The University of Manchester, Manchester 2 Greater Manchester Health Protection Team, Public Health England 3 Manchester Academic Health Sciences Centre, University of Manchester INTRODUCTION Invasive fungal disease is thought to be increasing in frequency in the UK due to a variety of factors including increased survival time from previously lethal illnesses and an increase in prevalence of conditions and treatments leading to immunosuppression. Understanding of the overall burden of invasive fungal disease in the UK is limited as there is no formal systematic or mandatory surveillance programme specific to fungal infections, although active surveillance networks exist for candidaemias (voluntary laboratory reporting1) and specifically for candidaemias in neonates (voluntary reporting2). In addition, several debilitating chronic and allergic fungal diseases, amenable to antifungal therapy have come to greater prominence. In 2008, the UK health Protection Agency issued a report entitled “Fungal Diseases in the UK: The current provision of support for diagnosis and treatment: assessment and proposed network solution”. A rough annual burden estimate of many fungal diseases was made in this report, but not subsequently published. Given this, we have attempted to quantify this burden with improved tools and an expanded range of serious fungal infections. METHODS We estimated the annual incidence of the following invasive fungal infections: cryptococcal meningitis, Pneumocystis pneumonia, invasive aspergillosis, candidaemia and Candida peritonitis, as well as oesophageal candidiasis. In addition, we have estimated the prevalence of chronic pulmonary aspergillosis, allergic bronchopulmonary aspergillosis (ABPA) and severe asthma with fungal sensitisation (SAFS). Information on incidence, prevalence and total burden of these conditions in England is limited. Where such information was available, we included it in the study. One example is data from the voluntary surveillance of candidaemia in England, Wales and Northern Ireland1. Where the information was not available we used a pragmatic approach for each fungal condition: 1. We considered which populations were most at risk of the condition 2. We sought published estimates for incidence or prevalence measures for the condition in these specific risk populations. 3. We applied these rates to published estimates of size of these high risk populations in the UK Where multiple estimates were published, we considered both internal validity (quality of the study, sample size etc.) and external validity (how similar the study population is to UK population, how recent the study is etc.) of the studies in deciding on which estimate to use. RESULTS The UK population in 2011 was 62,417,000 with 17% under the age of 15 and 23% over the age of 60 years. The following burden estimates were calculated: invasive candidiasis (IC) 4,700; Candida peritonitis complicating CAPD 88 and the remainder captured under IC; Pneumocystis pneumonia 587 cases, invasive aspergillosis (IA), excluding critical care patients 818 to 882, and IA in critical care 359 to 8,120 patients, utilizing different external assumptions, < 100 cryptococcal meningitis cases. With respect to allergic aspergillosis, 178,000 (50,000–250,000) ABPA cases in asthma and 873 adults and 278 children with cystic fibrosis. Chronic pulmonary aspergillosis is estimated to affect 3,600 patients, based on burden estimates post TB and in sarcoidosis. Infection Oesophageal candidiasis Invasive candidiasis Candida peritonitis ABPA Chronic pulmonary aspergillosis Invasive aspergillosis Cryptococcal meningitis Pneumocystis pneumonia Total burden estimated Number of infections per underlying disorder per year None HIV/AIDS Respiratory Cancer/Tx ICU - 62 - - - - - - - - - - 179,151 - - 3,600 62 0.1 4,703 7.5 88 88 0.14 - - 179,151 287 - - 3,600 5.77 8.15 - - 850 4,239 5,089 - - - - - <100 0.16 - - - - 587 0.94 850 4,327 193,380 310 62 182,751 CONCLUSIONS Estimating the burden of invasive fungal infection accurately is challenging due to the lack of a dedicated mandatory systematic surveillance system, and the wide range of incidence estimates for one of the largest high-risk population (patients in ICU). This is likely to be compounded by the limited sensitivity of traditional diagnostic tests used for invasive fungal illness, making it difficult to obtain laboratory confirmation for a significant number of cases. There is a high degree of uncertainty around the total estimate of burden due to: diagnostic limitations, the lack of a systematic national surveillance system, the limited number of studies published on the topic and the methodological limitations of calculating the burden. It was encouraging to note that for some conditions, our pragmatic approach resulted in a total estimate not too dissimilar to estimates calculated from recently published burden studies. This was the case for Pneumocystis pneumonia, where our pragmatic approach yielded an estimate of 522 cases, compared to an estimate of 587 cases derived from the published burden study3: a variation of approximately 10%. - - DISCUSSION There is a significant level of inaccuracy as our estimation methods have relied on limited published information, and there is a wide range of estimates for some of the published incidence rates. - Rate Total burden /100K To our knowledge, this is the first attempt at a comprehensive estimation of burden of invasive fungal infection in the UK. Further studies will likely need to combine methods (pragmatic and surveillance-based), take into account any new published information on specific incidence rates, and consider using alternative data sources such as the Hospital Episodes System (HES). An accurate estimate of total burden will ultimately rely on improved diagnostic testing and laboratory reporting. ACKNOWLEDGEMENTS LIFE: Leading International Fungal Infection. http://www.lifeworldwide.org/ REFERENCES 1. Public Health England (PHE). Voluntary surveillance of candidaemia in England, Wales and Northern Ireland: 2012. HPA, 2013. 2. http://www.neonin.org.uk/index 3. Maini R, Henderson KL, Sheridan EA, Lamagni T, Nichols G, Delpech V, et al. Increasing Pneumocystis pneumonia, England, UK, 2000–2010. Emerg Infect Dis , 2013.http://dx.doi.org/10.3201/eid1903.121151