Just A Sprain?
advertisement

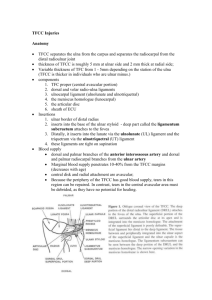
Just A Sprain? Tendonitis Finger joint injury Extrinsic ligament injury Intrinsic ligament injury TFCC injury Tendinopathy • de Quervain's Tenosynovitis • Intersection Syndrome • EPL Entrapment • Extensor Tendinitis • FCR Tendinitis de Quervain Tenosynovitis • Entrapment of APL & EPB in the 1st dorsal compartment of the wrist • Cause: Repeated thumb abduction with simultaneous wrist ulnar deviation • Symptoms: Radial wrist pain aggravated by thumb movement • 6:1 women; Age group 40-60 de Quervain's Tenosynovitis de Quervain Tenosynovitis • Splint - 30% effective • Splint + corticosteroids - 50-80% effective • Surgery - 90-99% effective • 20% textbook anatomy • Separate EPB Compartment or >1 APL slips de Quervain Tenosynovitis Post-op • Thumb Spica Splint for 14 days • Localized soreness for 4-6 weeks Intersection Syndrome • Tendon entrapment in 2nd dorsal compartment • Cause: Repetitive Wrist Motion • Common in athletes • Weightlifting, Rowing, Racquet sports • Symptoms: Pain & Swelling 4 cm proximal to wrist joint at intersection of APL, EPB, and wrist extensors. Possible crepitus Intersection Syndrome Intersection Syndrome • Modification/cessation of aggravating activity • NSAIDs • Wrist splint in 15 degrees extension • Corticosteroid injection • 2nd dorsal compartment release Intersection Syndrome Post-op • Wrist splint 10-14 days • Strengthening after 5-6 weeks EPL Tendinitis • Entrapment of EPL in 3rd compartment • Cause: Watershed area disrupted by undisplaced distal radius fracture or rheumatoid arthritis • Symptoms: Tenderness, swelling, & crepitus at Lister's tubercle EPL Tendon Entrapment EPL Tendinitis • EPL tendon transposition after 3rd compartment release EPL Tendinitis Post-op • Splinting not needed • Use as tolerated ECU Tendinitis • Entrapment of ECU tendon in 6th compartment • Cause: Twisting wrist injury or excessive ulnar deviation • Symptoms: Ulnar wrist pain & swelling with extension & ulnar deviation; Nocturnal pain • Differentiate from TFCC disruption ECU Tendinitis Diagnosis • MRI - Differentiates: • ECU Subluxation • peritendinous synovitis • longitudinal splitting of tendon • shallow ECU groove • anomolous tendon anatomy • Confirmed with Lidocaine injection into ECU sheath ECU Tendinitis • Wrist splint, NSAID, ice • Corticosteroid injection • 6th dorsal compartment release • Excise septum • Repair retinaculum ECU Tendinitis ECU Tendinitis Post-op • Ulnar gutter splint 2-4 weeks • Progressive use as tolerated FCR Tendinitis • Entrapment of FCR in tight fibrosseous tunnel • Occupies 90% of cross-sectional area • Cause: Most cases insidious/neighboring degenerative process • Repetitive flexion/extension or trauma rare • Symptoms: Pain at scaphoid tubercle aggravated by resisted wrist flexion/radial deviation FCR Tendinitis • Wrist splint, NSAID, ice for 4 weeks • Corticosteroid injection • FCR sheath release • Excise frayed fibers • Debride trapezial groove spurs FCR Tendinitis Post-op • Wrist splint for 2 weeks • Gradually increasing activity after 14 days Finger Joint Injury • Skier's Thumb • Thumb Radial Collateral Ligament Injury • Finger Collateral Ligament Injury Skier's Thumb • Acute Ulnar Collateral lLigament injury at the thumb MP joint • 10x more common than RCL injury • Cause: Sudden forced radial thumb deviation • Symptoms: Ulnar thumb MP joint tenderness, ecchymosis, and swelling • Signs: Ulnar thumb MP joint tenderness with radial deviation Skier's Thumb • Complete tear • Radial deviation > 30 degrees in extension or in 40 degrees flexion • Radial deviation > 15 degrees greater than other thumb • Stener Lesion • Associated proximal phalanx ulnar base avulsion fracture possible • Distal tear more common Stener's Lesion Skier's Thumb • Partial Rupture • Hand-based thumb spica splint for 6 weeks • AROM last 2 weeks • Resisted thumb activity after 3 months • Aching pain can last > 6 months Skier's Thumb • Complete Rupture • Operative Repair • Hand -based thumb spica splint for 6 weeks • MRI or Ultrasound to rule out Stener lesion Skier's Thumb Post-op • Hand-based thumb spica splint for 6 weeks • Controlled AROM 4x daily last 2 weeks • UCL stress (pinch, grasp) avoided for 12 weeks • Vague aching expected up to 1 year Thumb Radial Collateral Ligament Injury • Cause: Forced adduction of flexed MP joint • Proximal & distal tears equally • Symptoms: Symptoms: Radial thumb MP joint tenderness, ecchymosis, and swelling • Signs: Radial thumb MP joint tenderness with ulnar deviation Thumb Radial Collateral Ligament Injury • Complete tear • Ulnar deviation > 30 degrees in extension or in 40 degrees flexion • Ulnar deviation > 15 degrees greater than other thumb • Associated proximal phalanx radial base avulsion fracture possible • Proximal and distal tears equally common • MP joint volar subluxation more common Thumb Radial Collateral Ligament Injury • Partial Rupture • Hand-based thumb spica splint for 6 weeks • AROM last 2 weeks • Resisted thumb activity after 3 months • Aching pain can last > 6 months • Complete Rupture • Operative Repair Thumb Radial Collateral Ligament Injury Post-op • Hand-based thumb spica splint for 7 weeks • Controlled AROM 4x daily last 2 weeks • RCL stress avoided for 12 weeks • Vague aching expected up to 1 year Finger Collateral Ligament Injury • Classified by stability • Grade I: Pain, no laxity • Grade II: Laxity, firm endpoint, stable arc of motion • MP tested in 60 degrees flexion • Grade III: Grossly unstable, no firm endpoint Finger Collateral Ligament Injury • Grade I & II • Buddy taping, early ROM • MP: 30 degree flexion splint 3 weeks, then buddy tape • Grade III • Surgical repair • MP: 45 degree flexion splint 6 weeks, then buddy tape • PIP: Extension splint 6 weeks, then buddy tape Extrinsic Ligament Injuries • Palmar radiocarpal • Palmar ulnocarpal • Dorsal radiocarpal Intrinsic Ligament Injury • Scapholunate Interosseous Ligament • Dorsal component stronger • Lunotriquetral Interosseous Ligament • Volar component stronger • Dorsal Intercarpal Ligament TFCC Injury • Radioulnar ligaments stabilize DRUJ • Articular disk supports carpus and absorbs compressive forces TFCC Injury • Cause: Axial load on wrist with pronation (fall on outstretched hand or forceful rotational injury) • Symptoms: Ulnar wrist pain (with/without clicking) exacerbated by ulnar deviation or forceful rotation • Signs: Tenderness at ulnar wrist between FCU and ECU • Piano key sign TFCC Injury Palmer's Classifications of Triangular Fibrocartilage Complex Lesions Class 1: Traumatic A: Central perforation B: Ulnar avulsion With styloid fracture Without styloid fracture C: Distal avulsion (from carpus) D: Radial avulsion With sigmoid notch fracture Without sigmoid notch fracture Class 2: Degenerative (Ulnar Impaction Syndrome) A: TFCC wear B: TFCC wear Plus lunate or ulnar head chondromalacia C: TFCC perforation Plus lunate or ulnar head chondromalacia D: TFCC perforation Plus lunate or ulnar head chondromalacia TFCC Injury • Immobilization 4 to 6 weeks • Long arm if peripheral tear • Arthroscopy if not improved after 3 months • Arthroscopy • Repair if peripheral • Debride if central • Add wafer resection or ulnar shortening for ulnar positive variance • Open repair TFCC Injury Post-op • Ulnar gutter splint with early motion exercises following debridement • Long arm splint/cast for 4 weeks following repair followed by short arm splint for 2 weeks • PROM and gentle strengthening • Full activities at 12 weeks TFCC Injury