MANAGEMENT OF ANTICOAGULATION FOR ATRIAL FIBRILLATION 2014
1. CONFIRM ATRIAL FIBRILLATION/FLUTTER
2. DETERMINE STROKE RISK
3. CHOOSE ANTICOAGULANT AGENT, WITH ASSESSMENT OF BLEEDING
RISK
4. DRUG INTERACTIONS, ANTIPLATELET AGENTS.
DOCTOR JOFFE IS ON THE SPEAKER’S BUREAU FOR
BOEHRINGER-ENGELHEIM (PRADAXA)
Stroke risk was equivalent with intermittent and
sustained NVAF in SPAF trials1
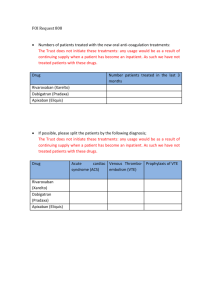
CHADS2 Risk Score and Corresponding Risk for Stroke in AF
Patients Not Treated With Anticoagulant Therapy
Points
0
Annual Stroke
Risk
95% Confidence Interval
1.9%
1.2-3.0
1
2.8%
2.0-3.8
2
4.0%
3.1-5.1
3
5.9%
4.6-7.3
4
8.5%
6.3-11.1
5
12.5%
8.2-17.5
6
18.2%
10.5-27.4
CHA2DS2-VASc
Congestive heart failure
Hypertension
Age > 75
Diabetes
Stroke/TIA/TE
Vascular disease (MI, PAD, aortic plaque)
Age 65-74
Female sex
1
1
2
1
2
1
1
1
CHA2DS2-VASc
Stroke rate %/year
0
0%
1
1.3%
2
2.2%
3
3.2%
4
4.0%
5
6.7%
6
9.8%
7
9.6%
8
6.7%
9
15.2%
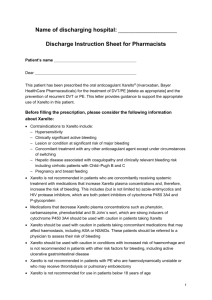
HAS-BLED
•
•
•
•
•
•
•
Hypertension=1
Abnormal renal/liver function=1
Stroke=1
Bleeding history or disposition=1
Labile INR=1
Elderly=1
Drugs/Alcohol=1
HAS-BLED
Clinically
Relevant
Bleeding
Major
Bleeding
0
7%
1%
1
8%
1%
2
11%
2%
3
16%
3%
4
15%
3%
>5
38%
8%
CHADS2
HAS-BLED
Clinically
Relevant
Bleeding
Major
Bleeding
0
7%
1%
1
8%
1%
4.6-7.3
2
11%
2%
8.5%
6.3-11.1
3
16%
3%
5
12.5%
8.2-17.5
4
15%
3%
6
18.2%
10.5-27.4
>5
38%
8%
Points
0
Annual
Stroke
Risk
1.9%
95% Confidence
Interval
1.2-3.0
1
2.8%
2.0-3.8
2
4.0%
3.1-5.1
3
5.9%
4
Score
0
Risk
Low
Anticoagulation Considerations
Aspirin (81-325 mg) daily or none
1
Moderate
Aspirin daily or warfarin (INR to
2.0-3.0) or dabigatran (Pradaxa)
or rivaroxaban (Xarelto) or
apixaban (Eliquis), depending on
factors such as patient preference
2 or greater
Moderate or High Warfarin (INR 2.0-3.0) or
dabigatran (Pradaxa) or
rivaroxaban (Xarelto) or apixaban
(Eliquis)
Pradaxa (dabigatran)
Direct, specific, competitive
thrombin inhibitor
TF/VIIa
X
IX
Half-life 12-17 hours
Uses P-gp transporter with
bowel absorption
VIIIa
Clearance :
Xa
Va
80% renal excretion
Not a substrate of CYP 450
enzymes
Oral, twice daily dosing
without need for coagulation
monitoring
IXa
II
Dabigatran
IIa
Fibrinogen
Fibrin
Adapted from Weitz et al, 2005; 2008
PRADAXA 150 mg twice daily was significant in reducing
PRADAXA= DABIGATRAN
the risk of stroke and systemic embolism an additional 35% vs warfarin
Significant risk reduction of both ischemic stroke and hemorrhagic stroke vs warfarin
Managing anticoagulant effects of PRADAXA in cases of hemorrhagic complications
Rivaroxaban (Xarelto)
TF/VIIa
Direct, specific, competitive
factor Xa inhibitor
X
IX
VIIIa
Half-life 5-13 hours
IXa
Rivaroxaban
Va
Clearance :
Xa
1/3 direct renal excretion
2/3 metabolism via CYP 450
enzymes
II
Oral, once daily dosing with
largest meal without need for
coagulation monitoring
IIa
Fibrinogen
Fibrin
Adapted from Weitz et al, 2005; 2008
Primary Efficacy Outcome
Stroke and non-CNS Embolism
Cumulative event rate (%)
6
5
Event
Rate
Rivaroxaban
Warfarin
1.71
2.16
Warfarin
4
Rivaroxaban
3
HR (95% CI): 0.79 (0.66, 0.96)
2
P-value Non-Inferiority: <0.001
1
0
0
No. at risk:
Rivaroxaban 6958
Warfarin
7004
120
240
360
480
600
720
840
960
Days from Randomization
6211
6327
5786
5911
5468
5542
Event Rates are per 100 patient-years
Based on Protocol Compliant on Treatment Population
4406
4461
3407
3478
2472
2539
1496
1538
634
655
Primary Safety Outcomes
Rivaroxaban
Warfarin
Event Rate
Event Rate
HR
(95% CI)
Pvalue
14.91
14.52
1.03 (0.96, 1.11)
0.442
Major
3.60
3.45
1.04 (0.90, 1.20)
0.576
Non-major Clinically
Relevant
11.80
11.37
1.04 (0.96, 1.13)
0.345
Major and non-major
Clinically Relevant
Event Rates are per 100 patient-years
Based on Safety on Treatment Population
Bleeding Sites
CrCl ≥50 ml/min
CrCl 30–49 ml/min
Riva 15 mg Warfarin
P-
Riva 20 mg Warfarin
(N = 1474) (N=1476) value (N=5637) (N=5640)
Pvalue
GI (upper, lower, and
rectal)
2.88
1.77
0.02
1.79
1.12
0.0002
Intracranial
0.71
0.88
0.54
0.44
0.71
0.02
Macroscopic
haematuria
0.05
0.18
0.22
0.28
0.19
0.21
Bleeding associated
with non-cardiac
surgery
0.24
0.42
0.31
0.15
0.19
0.61
Intra-articular
0.00
0.23
0.99
0.18
0.17
0.98
Epistaxis
0.19
0.09
0.40
0.10
0.13
0.53
*Major bleeding per 100 pt-yrs of follow-up
Key Secondary Efficacy Outcomes
Rivaroxaban
Warfarin
Event Rate
Event Rate
HR (95% CI)
P-value
4.51
4.81
0.94 (0.84, 1.05)
0.265
Stroke Type
Hemorrhagic
Ischemic
Unknown Type
0.26
1.62
0.15
0.44
1.64
0.14
0.58 (0.38, 0.89)
0.99 (0.82, 1.20
1.05 (0.55, 2.01)
0.012
0.916
0.871
Non-CNS Embolism
0.16
0.21
0.74 (0.42, 1.32
0.308
Myocardial Infarction
1.02
1.11
0.91 (0.72, 1.16)
0.464
All Cause Mortality
Vascular
Non-vascular
Unknown Cause
4.52
2.91
1.15
0.46
4.91
3.11
1.22
0.57
0.92 (0.82, 1.03)
0.94 (0.81, 1.08)
0.94 (0.75, 1.18)
0.80 (0.57, 1.12)
0.152
0.350
0.611
0.195
Vascular Death,
Stroke, Embolism
Event Rates are per 100 patient-years
Based on Intention-to-Treat Population
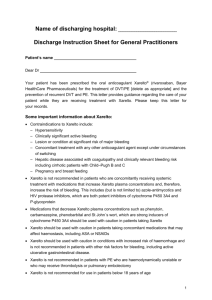
XARELTO® (rivaroxaban) Is Administered
With Once-daily Dosing
CrCl (mL/min)
Recommended
Once-daily Dose of XARELTO®
>50
20 mg
15 to 50
15 mg*
<15
Avoid use
♦ XARELTO® should be taken once daily with the evening meal
– Coadministration of XARELTO® 15 mg and 20 mg with food
increases its bioavailability to approximately 100%
♦ If a dose of XARELTO® is not taken at the scheduled time,
administer the dose as soon as possible on the same day
*Patients with CrCl 15 to 30 mL/min were not studied, but administration of XARELTO® 15 mg once daily is
also expected to result in serum concentrations of XARELTO® similar to those in patients with normal renal function.
Please see the full Prescribing Information, including Boxed WARNINGS, available at this event.
2828
XARELTO (rivaroxaban):
Drug-Drug Interaction Profile
Drugs (examples)
PK/PD Effects
Recommendation
Combined P-gp and strong CYP3A4 inhibitors
Ketoconazole, itraconazole,
lopinavir/ritonavir, ritonavir,
indinavir/ritonavir, conivaptan
Concomitant use increases XARELTO exposure and PD
effects; significant increases in rivaroxaban exposure
may increase bleeding risk
Avoid concomitant use
Combined P-gp and strong CYP3A4 inducers
Carbamazepine, phenytoin,
rifampin, St. John’s wort
Concomitant use decreases XARELTO exposure and
PD effects, which may decrease efficacy of XARELTO
Avoid concomitant use
if these drugs must be
coadministered
Combined P-gp and weak or moderate CYP3A4 inhibitors in the presence of renal impairment
(CrCl 15 to 50 mL/min)
Amiodarone, diltiazem,
verapamil, quinidine,
ranolazine, dronedarone,
felodipine, erythromycin,
azithromycin, cimetidine,
chloramphenicol
Based on simulated PK data, patients with renal
impairment receiving XARELTO concomitantly with
combined P-gp and weak or moderate CYP3A4 inhibitors
may have significant increases in exposure compared with
patients with normal renal function. Although increases in
exposure can be expected, results from ROCKET AF,
which allowed concomitant use of combined P-gp and
weak or moderate CYP3A4 inhibitors, did not show an
increase in bleeding in patients with CrCl 30 to <50 mL/min
Use only if potential
benefit justifies risk
Abbreviations: CYP = cytochrome P450; PK/PD = pharmacokinetic/pharmacodynamic.
Please see the full Prescribing Information, including Boxed WARNINGS, available at this event.
29
Interrupting rivaroxaban
Prior to Surgery or Intervention
♦ If anticoagulation must be discontinued to reduce the risk of
bleeding with surgery, then XARELTO® should be stopped at least
24 hours before the procedure
♦ In deciding whether a procedure should be delayed until 24 hours
after the last dose of XARELTO®, the increased risk of bleeding
should be weighed against the urgency of intervention
♦ XARELTO® should be restarted after the surgical or other
procedures as soon as adequate hemostasis has been
established
– If oral medication cannot be taken after surgical intervention,
consider a parenteral anticoagulant
– Wait at least 18 hours after last dose before removal of
epidural catheter, and do not restart until at least 6 hours
after removal.
Please see the full Prescribing Information, including Boxed WARNINGS, available at this event.
30
Considerations for Managing Bleeding in
Patients Receiving XARELTO® (rivaroxaban)
♦ A specific antidote for XARELTO® is not available
– XARELTO® is not expected to be dialyzable due to high
plasma-protein binding
– Protamine sulfate and vitamin K are not expected to affect the
anticoagulant activity of XARELTO®
– Use of procoagulant reversal agents, eg, PCC, APCC, or rFVIIa may
be considered, but has not been evaluated in clinical trials
♦ There is no experience with antifibrinolytic agents in individuals
receiving XARELTO®
♦ There is neither scientific rationale for benefit nor experience with
systemic hemostatics in individuals receiving XARELTO®
Abbreviations: APCC = activated prothrombin complex concentrate; PCC = prothrombin complex concentrate; rFVIIa = recombinant factor VIIa.
Please see the full Prescribing Information, including Boxed WARNINGS, available at this event.
31
Apixaban (ELIQUIS)
Direct, specific, competitive
factor Xa inhibitor
TF/VIIa
X
IX
Half-life 12 hours
VIIIa
Clearance :
27% direct renal excretion
Biliary and direct intestinal
excretion
P-gp transport
Oral, twice daily dosing
without need for coagulation
monitoring: 5mg bid. 2.5mg
bid with at least 2 of: 80 or
older, weight <60kg,
creatinine >1.5
IXa
Apixaban
Va
Xa
II
IIa
Fibrinogen
Fibrin
Kaplan–Meier Curves for the Primary Efficacy and Safety Outcomes.
Granger CB et al. N Engl J Med 2011;365:981-992.
Bleeding Outcomes and Net Clinical Outcomes.
Granger CB et al. N Engl J Med 2011;365:981-992.
APIXABAN DRUG INTERACTIONS
• Strong Dual Inhibitors of CYP3A4 and P-gp:
Increase exposure to apixaban and increase the risk of
bleeding.
Decrease the dose of ELIQUIS to 2.5 mg twice daily (e.g.,
ketoconazole, itraconazole, ritonavir, or clarithromycin).
In patients already taking ELIQUIS at a dose of 2.5 mg twice daily,
avoid coadministration with strong dual inhibitors of CYP3A4 and Pgp.
• Strong Dual Inducers of CYP3A4 and P-gp:
Decrease exposure to apixaban and increase the risk of stroke.
Avoid concomitant use of ELIQUIS e.g., rifampin, carbamazepine,
phenytoin, St. John's wort.
APIXABAN
ELIQUIS should be discontinued at least 48 hours
prior to elective surgery or invasive procedures with
a moderate or high risk of unacceptable or clinically
significant bleeding.
ELIQUIS should be discontinued at least 24 hours
prior to elective surgery or invasive procedures with
a low risk of bleeding or where the bleeding would
be noncritical in location and easily controlled.
FDA POSITION FROM TRIALS
• Dabigatran significantly reduced stroke or
systemic embolism, and ischemic stroke alone,
with similar major bleeding versus warfarin.
• Rivaroxaban similar rates of stroke or
embolism and major bleeding versus warfarin.
• Apixaban: significant reductions in stroke or
systemic embolism, major bleeding and
mortality compared to warfarin.
Pradaxa
Xarelto
Eliquis
150mg bid Cr.Cl >30
75mg bid Cr.Cl 15-30
Avoid Cr.Cl <15
20mg Cr.Cl >50
15mg Cr.Cl 15-50
Avoid Cr.Cl <15
5mg bid
2.5mg bid if 2 or more:
>80, <60kg, >creat 1.5
With or without food
Largest meal
With or without food
Avoid with rifampin,
quinidine
If Cr.Cl 30-50, reduce dose
to 75mg bid with Multaq
and ketoconazole. If Cr.Cl
<30, avoid Multaq and
ketoconazole.
Verapamil may increase
levels
Avoid rifampin,
carbamazepine, phenytoin,
St. John’s wart. Avoid
ketoconazole, traconazole,
lopinavir/ritonavir, itonavir,
indinavir/ritonavir,
conivaptan.
Avoid
amiodarone,diltiazem,
verapamil, Multaq,
erythromycin, Ranexa,
azithromycin, cimetidine
if Cr.Cl 15-50
Avoid rifampin,
carbamazepine, phenytoin,
St. John’s wart. Reduce to
2.5mg bid with
ketoconazole, itraconazole,
Biaxan. If on 2.5mg bid,
stop Eliquis.
PRADAXA
XARELTO
ELIQUIS
Converting from warfarin:
start when INR<2
Converting from warfarin:
start when INR<3
Converting from warfarin:
start when INR<2
Rapid onset
No monitoring
(PTT)
Rapid onset
No monitoring
(INR, PTT, anti-factor Xa
activity)
Rapid onset
No monitoring
(INR, PTT, anti-factor Xa
activity)
1-2 day hold if Cr.Cl >50
3-5 if Cr.Cl <50
At least 24 hours
At least 24 hours low risk
At least 48 hours high risk
Baseline Cr.Cl , at least 6
monthly
Baseline Cr.Cl, at least 6
monthly
Baseline Cr.Cl, at least 6
monthly
Extreme caution with
epidural catheters
Extreme caution with
epidural catheters
Extreme caution with
epidural catheters
Cannot crush
Can crush (apple sauce)
Cannot crush
PRADAXA
XARELTO
ELIQUIS
DVT, PE, extended
DVT, PE, extended
DVT, PE, extended
Hip and knee
prophylaxis
Hip and knee
prophylaxis