LVADs_in_the_Emergency_Department
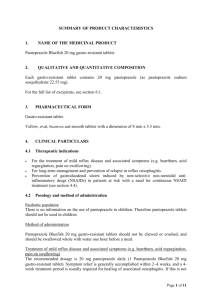
advertisement

LVADS IN THE EMERGENCY DEPARTMENT ZAK CERMINARA PHARMD UW MEDICINE RESIDENT SEPTEMBER 4, 2014 CONTENT • • • • • • Background Pharmacotherapy Infections GI Bleeds Arrhythmias/Codes Miscellaneous PATIENT PRESENTATION • • • • MJM 64 y/o male ICM s/p LVAD 6/2014 Hx of 2 recent admits for GI bleeds Presented to the ED on 8/21 with solid, black stools since 1200 that day with mild fatigue PMH • • • • • • • • • Coronary artery disease Hx of complete heart block HeartMate II LVAD in place Chronic anticoagulation Hx of acute renal failure Acute blood loss anemia Protein calorie malnutrition Situational depression Insomnia HISTORIES • Allergies: • NKDA • Family History: • Father: CVA • Brothers: DM • Social History: • EtOH: Occasional • Tobacco: Smoked for 40-45y, quit • IVDU: Denies HOME MEDICATION LIST Indication Medication Heart History ASA 81 mg PO Daily Metoprolol Succinate 25 mg PO BID Pravastatin 20 mg PO daily Warfarin 1.5 mg PO Qmonday Warfarin 2 mg PO QTuWThFSaSu GERD/GI Bleed Hx Pantoprazole 40 mg PO daily Pain APAP 650 mg PO Q6H PRN Oxycodone 5 mg PO Q6H PRN Constipation Docusate 200 mg PO daily PRN Supplements Multivitamin PO daily Vitamin D 1000 IU PO daily Magnesium Oxide 400 mg PO BID VITALS • Admission to ED • • • • • • Weight: 86.5 kg Height: 6’ 1” BMI: 25.2 BP=MAP: 61 Temp: 36.7 RR: 20 LABS: CBC 8/21 WBC RBC Hgb Hct MCV Plt 5.82 2.39 7.2 22 94 279 LABS: BMP Na 8/21 K 140 4.2 Cl CO2 111 24 Anion Gap SCr BUN Ca Corrected Ca 5 1.12 24 8.2 9.32 LABS: LFTS 8/21 AST ALT Alk Phos Bili Albumin 25 25 56 0.7 2.6 LABS: COAGULATION 8/21 PT INR aPTT 27.4 2.6 37 BACKGROUND Heart failure (HF) is increasing in prevalence 5.7 million currently have diagnosis 670,000 are newly diagnosed yearly 1 year mortality rate is 20% Less than 15% survive 8-12 years Pharmacotherapy can be used to manage HF in the earlier stages • Transplant is the preferred therapy for end-stage HF • Left ventricular assist devices (LVADs) have become increasingly more popular • • • • • • Circulation. 2012 Jan 3;125(1):e2-e220. BACKGROUND CONT. • LVADs decrease symptoms by decreasing the work of the heart • LVADs: • Reverse HF • Bridge to transplant • Destination therapy Circulation. 2012 Jan 3;125(1):e2-e220. Int J Cardiol. 2013 Oct 15;168(6):5143-8. PHARMACOTHERAPY • • • • • • • • Angiotensin-converting enzyme inhibitors (ACEIs) Angiotensin II receptor blockers (ARBs) Aldosterone Antagonists Digoxin Beta blockers Diuretics Hydralazine (+/- nitrates) Warfarin Int J Cardiol. 2013 Oct 15;168(6):5143-8. INFECTIONS INFECTIONS • Infection rates have been shown to be 25-80% • VAD-related infections should be treated aggressively • Common VAD-related infections • • • • Driveline Pocket Mediastinitis Pump endocarditis Int J Cardiol. 2013 Oct 15;168(6):5143-8. J Heart Lung Transplant. 2011 Apr;30(4):375-84. INFECTIONS CONT. • Goal of therapy is to keep infection confined to prevent progression • Device related infections do not prevent transplant • Non-VAD related infections require aggressive treatment Int J Cardiol. 2013 Oct 15;168(6):5143-8. INFECTIONS CONT. • Retrospective study by Nienaber et al. • They identified 101 episodes of LVAD infections in 78 of 247 patients (32%) • Most common infection: Drive line infections (47%) • Followed by VAD and non-VAD related BSIs (24% and 22%) • Pathogens: • Gram-positive cocci, staphylococci (45%) • Gram-negative bacilli, nosocomial (27%) • Chronic suppressive antimicrobial therapy: 42% • Intraoperative debridement: 14% • VAD removal: 3 patients Int J Cardiol. 2013 Oct 15;168(6):5143-8. BLEEDING BLEEDING • Bleeding is the most common adverse event associated with VAD therapy • Common bleeding issues: • • • • • Epistaxis Gastrointestinal bleeding Vaginal bleeding Cuts or other trauma Complications after outpatient procedures • Bleeding may be related to: • Systemic anticoagulation • Operation • Acquired von Willebrand disease Int J Cardiol. 2013 Oct 15;168(6):5143-8. POSTOPERATIVE BLEEDING • Immediate postoperative bleeding may be related to: • Adhesions • Cannulation sites • Coagulopathy • In many causes can be controlled using: • • • • Blood products Hemostatic agents (aminocaproic acid) Desmopressin acetate Protamine sulfate Int J Cardiol. 2013 Oct 15;168(6):5143-8. VON WILLEBRAND SYNDROME • In a study of 26 patients with LVADs • All subjects developed von Willebrand syndrome • It was reversible on explant • A different prospective study examined the characteristics of von Willebrand syndrome related to LVADs • All patients developed von Willebrand syndrome • The cause is unknown • It may be due to the stress of the continuous flow VAD leading to proteolysis of the multimers Int J Cardiol. 2013 Oct 15;168(6):5143-8. HEMOLYTIC ANEMIA • Hemolysis occurs when RBCs lyse as they pass through the VAD • Related to platelet activation • Patients may develop symptoms: • Fatigue • Dark tea-colored urine • Icterus • Management includes: • Close monitoring • Possible addition of dipyridamole • May occur at a rate of 1.2% to 3% Int J Cardiol. 2013 Oct 15;168(6):5143-8. ARRHYTHMIAS/CODING ARRHYTHMIAS • Arrhythmias occur in approximately 27% to 38% of VAD patients • Treatment options include: • Fluid boluses • Antiarrhythmic agents (amiodarone, beta-blockers +/mexilitene) • Normalization of serum electrolyte • Weaning pressors • Direct current cardioversion/Defibrillation • Always continue preoperative antiarrhythmics after LVAD implantation Int J Cardiol. 2013 Oct 15;168(6):5143-8. Crit Care Med. 2014 Jan;42(1):158-68. CODING • When terminal rhythms occur with power outputs indicating flow through the device use only: • Electrical cardioversion/defibrillation • Epinephrine • Atropine • When power output is low, compressions may be necessary • The major risk with chest compressions is dislodgement of: • The device • The outflow cannula • This is mainly of concern with the larger devices • Alternative is abdominal compressions, given 1–2 inches left of midline Int J Cardiol. 2013 Oct 15;168(6):5143-8. Resuscitation. 2014;85(5):702-4. doi: 10.1016. ABDOMINAL COMPRESSIONS • One case study of performed abdominal resuscitation in an LVAD patient successfully • Abdominal compressions can maintain a coronary perfusion pressure of 15 mm Hg • At ROSC, care should be taken to support the ischemic RV J Cardiothorac Surg 2011; 6:91. MISCELLANEOUS MISCELLANEOUS • Neurologic • Turbulent flow leads to thrombus formation and stroke • Newer pumps decrease this risk • RV Failure • An imbalance can develop between the ventricles • Incidence ranges from 11.8% to 14.8% • Can lead to pulmonary hypertension • Multiple Organ Failure • Device Malfunction Int J Cardiol. 2013 Oct 15;168(6):5143-8. BACK TO MJM • Medications given in the ED: • Pantoprazole 80 mg bolus • Pantoprazole 8 mg/hr drip • Medications in the ICU: • Pantoprazole 8 mg/hr drip for total 24 hrs • Pantoprazole 40 mg PO BID through 8/27 • All home medications • Warfarin was held REFERENCES 1. 2. 3. 4. 5. 6. Roger VL, Go AS, Lloyd-Jones DM et al. Heart disease and stroke statistics 2012 update: a report from the American Heart Association. Circulation. 2012 Jan 3;125(1):e2-e220. Pistono M, Corrà U, Gnemmi M et al. How to face emergencies in heart failure patients with ventricular assist device. Int J Cardiol. 2013 Oct 15;168(6):5143-8. Nienaber JJ, Kusne S, Riaz T et al. Clinical manifestations and management of left ventricular assist device-associated infections. Mayo Cardiovascular Infections Study Group. Clin Infect Dis. 2013;57(10):1438-48. Hannan MM, Husain S, Mattner F et al. Working formulation for the standardization of definitions of infections in patients using ventricular assist devices. International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2011;30(4):375-84. Pratt AK, Shah NS, and Boyce SW. Left Ventricular Assist Device Management in the ICU. Crit Care Med. 2014 Jan;42(1):158-68. Rottenberg EM, Heard J, Hamlin R et al. Abdominal only CPR during cardiac arrest for a patient with an LVAD during resternotomy: A case report. J Cardiothorac Surg 2011; 6:91. Shinara Z, Bellezzoa J, Stahovich M et al. Chest compressions may be safe in arresting patients with left ventricular assist devices (LVADs). Resuscitation. 2014;85(5):702-4. doi: 10.1016.