GI tract infections in IBD: Detection
and treatment of Clostridium difficile,
CMV and enteric pathogens:
Case studies
David G. Binion, MD
Bruce E. Sands, MD, MS
Case 2: Severe Pouch Inflammation
• 32 yo woman undergoing a 3 stage colectomy
and J pouch reconstruction for refractory
ulcerative colitis
• Diagnosed with UC at age 22, maintained on
mesalamine, then worsening of disease 3 years
ago. Escalation to immunomodulator and
infliximab with no improvement
• Colectomy for steroid dependent, poorly
controlled disease; end ileostomy (6 months
earlier).
• J pouch and diverting loop ileostomy (2 months
earlier
Case 2: Severe Pouch Inflammation
• Pt employed as dental hygienist in VA Hospital
and domicillary
• Admitted with 2 weeks of worsening rectal
discharge, pelvic and abdominal pain; fevers.
• Admitted to surgical service
• Exam
– Febrile to 101, tachycardic
– Abdomen: distended, hypoactive bowel sounds,
tender
– Stenosis at the anal cuff/pouch anastomosis
Case 2: Severe Pouch Inflammation
• What diagnostic tests on admission?
• Pouchoscopy
• CT scan of abdomen and pelvis
Endoscopic appearance of the J pouch and
proximal ileum
•
J pouch with
diverting loop
ileostomy
•
Ileum above J pouch
downstream from
diverting loop
ileostomy
Hamlin P J et al. Postgrad Med J 2004;80:233-235
Case 2: Severe Pouch Inflammation
• J pouch with diverting
loop ileostomy
(contrast passes into
the ostomy)
• Dilated bowel loops in
diverted, downstream
small bowel
• Bowel wall thickening
• Ascites
Case 2: Severe Pouch Inflammation
• Stool sample sent from pouchoscopy
• C difficile is detected
• What are data regarding C difficile infection of
small bowel and J pouch?
Case 2: Severe Pouch Inflammation
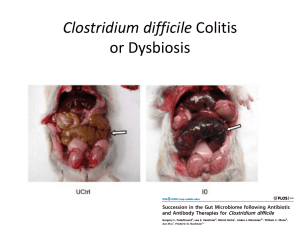
C difficile enteritis: An early complication in IBD
patients following colectomy
• Rare but associated with significant morbidity with mortality rates
ranging from 60-83%
• Institutional series of six patients (2004-2006). C difficile enteritis
manifested with high volume watery ileostomy output, ileus, fever
with leukocytosis. No mortality with prompt diagnosis and therapy
Miller, D.L et al. Arch Surg, 1989; 124: p. 1082.
Jacobs, A., et al. Medicine, 2001; 80: p. 88-101.
Hayetian, F.D., et al. Arch Surg, 2006; 141: p. 97-9.
Lundeen S et al. J Gastroentest Surg 2007; 11:138-142
Surawicz C. et al. Am J Gastroenterol 2013; 108: 478-498.
Case 2: Severe Pouch Inflammation
How can we treat diverted bowel?
•
•
•
•
•
•
Oral metronidazole
Intravenous metronidazole
Oral vancomycin
Vancomycin enema
Injection of vancomycin into loop ileostomy
Intravenous vancomycin
Lundeen S et al. J Gastroentest Surg 2007; 11:138-142
Surawicz C. et al. Am J Gastroenterol 2013; 108: 478-498.
Zuckerbraun B. et al. Ann Surgery 2011; 254: 423-7.
Case 2: Severe Pouch Inflammation
How can we treat diverted bowel?
• Metronidazole is rapidly absorbed and will enter distal GI tract after
biliary excretion (normal bowel)
• Metronidazole in bloodstream will cross into lumen of inflamed
mucosa
• Vancomycin oral delivery will not enter distal, diverted small bowel
• Vancomycin enema is effective; strictured anal cuff/pouch
anastomosis made this initially
• Injection (lavage) of vancomycin flushes into the afferent limb of loop
ileostomy
Lundeen S et al. J Gastroentest Surg 2007; 11:138-142
Surawicz C. et al. Am J Gastroenterol 2013; 108: 478-498.
Zuckerbraun B. et al. Ann Surgery 2011; 254: 423-7.
Case 2: Severe Pouch Inflammation
How can we treat diverted bowel?
• Patient responded to vancomycin flushes into the loop ileostomy
• Dilation of the anastomotic stricture allowed for vancomycin enema
therapy to be initiated
• Recurrence of C difficile after initial therapy stopped after 2 weeks.
• Prolonged vancoymcin used until time of the loop ileostomy
takedown
Lundeen S et al. J Gastroentest Surg 2007; 11:138-142
Surawicz C. et al. Am J Gastroenterol 2013; 108: 478-498.
Zuckerbraun B. et al. Ann Surgery 2011; 254: 423-7.
Case 2: Severe Pouch Inflammation
Long-term results after takedown of diverting
ileostomy
Case 3: Is this C difficile?
• 38 yo woman with 10 year history of Crohn’s colitis on
azathioprine and adalimumab therapy in durable
remission becomes sick with first colitis flare in 4 years. C
difficile infection at time of diagnosis.
• Patient contacts office with complaint of 10 loose bowel
movements per day, nocturnal bowel movements,
abdominal pain
• Patient was visiting elderly relative in hospital and longterm care facility over the past month
• It is Friday afternoon. Stool testing cannot be brought to
lab until Monday
• What should we do?
Case 3: Is this C difficile?
• Oral vancomycin is started – 125 mg four times
per day
• Patient improves over initial 3 days
• Stool sample is brought in while patient is on
therapy, and is negative
• How accurate is stool analysis if the patient is on
therapy?
Case 3: Diagnostic Tests for C difficile
Gene
Target Chemistry/Manufacturer
Sensitivity
Specificity
PPV
NPV
Gold standard
tcdB Prodesse (Gen-Probe
Prodesse, Waukesha,
WI, USA)
77.3
99.2
99.2
99.4
TC
tcdB BD GeneOhm (BD
Diagnostics, LaJolla,
CA, USA)
96.4
99.1
99.6
91.4
Composite
tcdB Cepheid
(Sunnyvale, CA, USA)
97.1
93.0
72.3
99.4
CCCNA
tcdB BD GeneOhm
88.5
95.4
88.5
95.4
TC
tcdB BD GeneOhm
83.6
98.2
89.5
97.1
TC
tcdC FRET
86
97
90
96
TC
tcdB SYBR green
93.3
97.4
75.7
99.4
Composite
tcdB Taqman-FAM
87.1
96.5
60.0
99.2
CCCNA
Proportion PCR positive
Time to conversion of CDI test to negative while on
therapy by treatment (vanco n=20)
Sunkesula V et al. Clin Infect Dis. 2013;57:494-500
Case 3: Is this C difficile?
• Nucleic acid testing for C difficile is a major
advance in the laboratory diagnosis of CDI, but it
cannot be the basis for withholding therapy in
situations where pre-test suspicion is high
• Once on therapy, sensitivity of PCR based
detection of C difficile decreases rapidly
• Once initiated, commit to treatment. No rationale
for retesting for C difficile during initial treatment
time period
Surawicz C. et al. Am J Gastroenterol 2013; 108: 478-498.
What’s new in treatment …
Surawicz CM, Brandt LJ, Binion DG et al. Am J Gastroenterol 2013; 108: 478-498.
Metronidazole vs. oral vancomycin for C. difficile:
Picking your first therapy:
Surawicz CM, Brandt LJ, Binion DG et al. Am J Gastroenterol 2013; 108: 478-498.
Fidaxomicin and vancomycin for initial
C. difficile infection: 30 day recurrence
Louie et al. N Engl J Med 364 (5):422-431, 2011.
Recurrent C difficile in IBD
• Prolonged antibiotic therapy (oral vancomycin)
• Fecal microbiome transplant (FMT)
– Associated with IBD flare
– Resolution of recurrent CDI in IBD
De Leon L, Watson JB, Kelly CR. Clin Gastroenerol Hepatol 2013; 11: 1036-1038.
Zainah H, Silverman A. Case Rep Inf Dis 2012; 2012: 810943
Case 4: Bloody diarrhea in terminal
ileal Crohn’s disease
• 66 yo woman with 40 year history of Crohn’s ileitis, who
had required an ileocectomy 30 year prior is admitted to
the hospital with severe bloody diarrhea, tachycardia,
dehydration and abdominal pain.
• No prior history of Crohn’s colitis on colonoscopies. Last
colonoscopy performed 2 years prior showed healthy
anastomosis, diverticuli.
• Oral mesalamine maintenance therapy
• Visits with individuals in hospital and nursing home
regularly. Diaper changing of new granddaughter.
Case 4: Bloody diarrhea in terminal
ileal Crohn’s disease
• Physical exam obese abdomen, tender to deep palpation.
Tachycardic with HR 110
• On admission CRP 9.65 mg/dl
• WBC 20.3, 9% bands
• What is your differential diagnosis?
• Which diagnostic tests to perform?
Endoscopic appearance of the colon
• Transverse
colon
• Transverse
colon
Salmonella enteritidis
Source – peanut butter
Endoscopic appearance of C difficile infection
IBD
non-IBD
Issa M et al. Clin Gastroenterol Hepatol. 2007;5: 345-51.