Care of the Patient with an EVD or Lumbar Drain
advertisement

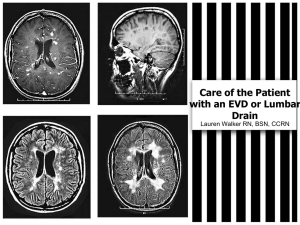
Care of the Patient with an EVD or Lumbar Drain Lauren Walker RN, BSN, CCRN Objectives • Review prerequisite nursing knowledge necessary for competent care of a Lumbar or EVD drain. • Review EVD and Lumbar equipment, monitors, patient positioning, and management. • Discuss neurologic assessment with a Lumbar Drain or EVD. • Analyze possible complications of specific drains and pressure monitoring. • Discuss procedure for sending CSF for testing. • Return-demonstration of management and care of the Lumbar drain and EVD. CSF and Ventricular System • CSF is a colorless, clear fluid produced by choroid plexus in third and fourth ventricles. – Functions as a cushion for brain and spinal cord • 500-600 ml CSF produced daily • 125-150 ml circulates in the ventricular system and subarachnoid space at one time (remainder is reabsorbed) • Brain has four CSF filled and interconnected ventricles Intracranial Pressure • Intracranial Pressure (ICP) is the pressure exerted by the brain content: – Brain Tissue (85%) – Cerebral Spinal Fluid (CSF) (10%) – Intravascular blood (2-11%) • Cerebral Autoregulation: The ability of the cerebral vessels to constrict and dilate as needed to maintain adequate cerebral perfusion – Impaired with brain injury and the cerebral blood flow becomes passively dependent on blood pressure • Monro-Kellie Hypothesis: an increase in one component must be offset by an equal decrease in one or more components otherwise an increase in ICP will result ICP Pressures Normal ICP 0-10 mmHg • Increased ICP occurs when the intracranial volume exceeds the brain’s ability to compensate for increased volume • Sustained ICP above 20 mmHg is considered a neurologic emergency • When the brain suffers an insult or injury, changes occur that affect cerebral hemodynamics, including changes in ICP, cerebral blood flow, and oxygen delivery Cerebral Perfusion Pressure • Cerebral Perfusion Pressure (CPP): Pressure at which the brain is perfused – About 15-20% of cardiac output CPP = Mean Arterial Pressure (MAP) – ICP. • Normal CPP 60-80 mmHG • CPP less than 50mmHg will result in cerebral ischemia and tissue death Causes of Increased ICP • Contusions • Hematomas • Tumors • Infarcts • Coughing • Endotrachial suctioning • Hypercarbia • Fluid overload • Hypoxia • Mechanical ventilation (PEEP) • Increased CSF Production • Valsalva maneuver • Metabolic disturbances Indications for Measuring ICP • TBI with GCS of less than or equal to 8 – with an abnormal CT scan results – Normal CT scan results with hypotension, posturing, and older than 40. • Fulminant hepatic failure with encephalopathy • Ischemic Stroke with massive edema • Meninigitis • ICH • Cysts • SAH • Hydrocephalus • Cerebral Edema • Congenital anomalies • Mass • Craniosynostisis ICP Monitoring and the EVD • Intraventricular catheters are the gold standard for measuring ICP – Placed directly in the ventricle (typically in the anterior horn of the lateral ventricle through a burr hole in the skull) – Attached to a pressure transducer • An external ventricular device (EVD) – Has ICP monitoring capabilities – Can also assist with controlling increased ICP by CSF drainage • The main disadvantage to an EVD is that it is the most invasive device because it penetrates the meninges and brain ICP Monitoring and Lumbar Drains • Lumbar drainage devices (LD) are closed sterile systems that allow the drainage of CSF from the subarachnoid space. • LD are inserted via a specialized spinal needle into the lumbar subarachnoid space at the L2–L3 level or below – avoids injury to the spinal cord • In the lumbar CSF space, the spinal catheter will be alongside the cauda equina – Consists of the ventral and dorsal spinal nerve roots that descend from the spinal cord and exit the spinal canal at lumbosacral levels Lumbar Space ← → ← → ← Dural Tube L1 pedicle Conus Medularis L2 pedicle Spinal Cord ends at L1-L2 at Conus Medularis Sacrum → Cauda Equnia LD is inserted in lumbar subarachnoid space: L2 to L3 space avoiding injury to spinal cord Indications for a Lumbar Device • Postoperative or traumatic dural fistula (CSF leak) • Treatment of shunt infections • Diagnostic evaluation of idiopathic normal pressure hydrocephalus • Reduce ICP during a craniotomy • Adjuvant therapy in the management of TBI • Thoracoabdominal AAA to improve spinal cord perfusion • Manage nontraumatic subarachnoid hemorrhage to prevent vasospasm • Manage increased ICP associated with cryptococcal meningitis Patient Care with LD • Patient positioning is crucial to prevent complications – The head of the bed, height of drainage chamber, and changes in patient positioning must be monitored closely to prevent sudden overdrainage. – Patients may turn from side to side without significant impact on drainage unless the catheter is found to be positional. – Nursing staff should monitor which positions result in variances in drainage rate from the LD and plan patient care • Perform a complete motor and sensory exam with neuro exam – Assess for s/s of meningeal irritation • Photophobia, neck stiffness, N/V, HA, bowel and bladder function Expected Outcomes of ICP Monitoring and CSF Drainage • Avoid secondary injury • Patient will maintain CPP of approximately 60-70 mmHG • WBC will be within expected limits • CSF cell count, protein, glucose and culture will be within expected limits • Patient/family will receive information and reinforcement regarding ICP monitoring and CSF drainage • Visitors will verbalize understanding of limiting movement of patient Patients who require an EVD or LD should be closely monitored by nurses trained and competent in assessment and management of both the drain and the neuroscience patient population Nursing Management and Assessment Maintain optimal cerebral tissue perfusion • Perform and document neuro assessment every hour and PRN and note trends. Notify physician for changes in neuro status and CPP less than 60mm Hg for more than 5 minutes. • Monitor Hourly: – Vital Signs: BP, pulse, respiration and temperature. – Pupil size and reaction – Glasgow coma scale – ICP – MAP – CPP = MAP – ICP Nursing Management and Assessment Monitor the patient every hour and as necessary for symptoms of increasing ICP • Change in level of consciousness: – Headache – Restlessness/agitation – Nausea/Vomiting – Seizure activity – Visual changes – Changes in LOC – Changes in pupillary responses – Labored respirations and/or pattern – Changes in motor strength – Cushing’s Triad: Increasing BP with a widening pulse pressure, decreased HR, irregular respirations Nursing Management and Assessment Assessment of the EVD/Lumbar Drain hourly • Inspecting EVD from insertion site along the entire drainage system – Check for cracks in the system or fluid leaking from the insertion site – Dressing is intact • Hourly assessment of CSF drainage amount, color, and clarity. • Ensure the system is appropriately clamped or open depending on order. • Check patient position to ensure transducer is at the ordered reference level. – If the patient is very active and moving around in bed, it is imperative to frequently assess that the drain is leveled appropriately to prevent over- or under-drainage. Nursing Management and Assessment Facilitate venous return: • Patient’s head may be elevated according to the discretion of the attending and neurosurgeon. • The head position must remain neutral, may use soft cervical collar or sandbags, if necessary. • Prevent hip flexion greater than 90 degrees. • Instruct family members regarding the plan of care and the need to limit stimulation of patient r/t head injury. Nursing Management and Assessment • Identify activities that alter intracranial pressure – lights, noise, repositioning • Arrange nursing care to minimize elevation in ICP (cluster care) • Assess ICP waveform continuously • Body temperature should remain below 38 C. • Assure prescribed seizure prophylaxis is instituted if indicated. Nursing Management and Assessment • Monitor labs, as ordered. – Maintain HCT greater than 25%. – If patient is receiving Mannitol, obtain Serum Osmolarity every 6 hours. (Notify MD prior to administering if serum osmo > than 310). • Record I/O every hour. – If urine output is greater than 200 mL for 2 hours and specific gravity is less than 1.005, not associated with Mannitol dosing, notify neurosurgeon Managing Complications • If the ICP is greater than 15 mmHg, rises abruptly or is greater than parameters determined by the MD and/or the CPP is less than 60 mmHg for more than 5 minutes and notify MD: – Remove any stimulus from the patient. – Reposition head to neutral position. – Confirm adequate volume status (CVP 7-13). If low, obtain order for volume replacement or follow Traumatic Brain Injury Protocol as ordered. – Medicate with medications as ordered after assessing patient LOC. EVD Complications • An absence of an ICP waveform – May be the result of air bubbles, clots, or debris within the drainage tubing or across the transducer. – A malfunctioning pressure cable, module, or transducer may also result in the loss of the ICP waveform • Infections – Manipulation and accessing of drainage tubing can be a source of contamination – Drainage tubing accidentally becomes disconnected: every effort should be made to maintain the sterility of the ventricular catheter. • New sterile EVD tubing should be obtained and connected – An occlusive dressing is placed to cover both incisions EVD Complications • CSF Overdrainage – EVD: Maintain the drip chamber at the prescribed zero reference and pressure levels – Family and Pt education!! • changing the bed position is to be performed only with assistance. • Raising the level of the bed with an can result in a large increase in CSF drainage. – Clamp the device any time there is a patient response or procedure that may cause CSF Overdrainage – Clamp for coughing, vomiting, suctioning, or repositioning. Lumbar Drain Complications • Overdrainage – Movement and repositioning of the patient – Not frequently observing the amount draining • Infection at insertion site – Manipulation of catheter and tube could be a source of contamination – Non-occlusive dressing • Tube Dislodgement • Lower extremity weakness • Changes in bowel and bladder patterns – Could indicate a nicked nerve • Tracking in tubing – Bleeding in spinal cord Management of the EVD and Lumbar Drain Zeroing the Transducer EVD • Raise or lower the system measured to the tragus of the ear • Lower the Buretrol to the “zero point” on the system by pinching the tabs together above the buretrol and lowering into alignment with zero on the device • Turn the stopcock “off” to the patient (open to the Buretrol/transducer) • Do Not open the transducer to air (the transducer will be opened to air automatically through the vent on top of the Buretrol). • Highlight the ICP box on the GE monitor screen and select “zero ICP” on the drop down menu choices. Wait for a “0” to appear on the monitor for the ICP reading. • Replace the Buretrol to the position on the pole mount that has been ordered by the physician. • Zero the ICP every 12 hours Leveling EVD • The transducer on the set-up is leveled to the patient’s external auditory meatus. • The “pressure level” indicator (located on the drip chamber of the collection system) is aligned to the ordered cm H2O above the external auditory meatus. • If continuously draining CSF, turn the drain off to the patient momentarily to obtain the ICP reading. Level to Tragus of Ear for EVD Leveling EVD Obtaining an ICP Tracing • Turn stopcock “off” to the drain and “open” to the transducer to obtain an accurate ICP numerical value and waveform. • The ICP numerical value and waveform should be obtained every hour. – If there is an increase in intracranial pressure, then the value should be obtained more often (i.e., Q15 minutes). Draining CSF • For Continuous ICP Measurements: – Keep the EVD stopcock “off” to drain and “open” to the transducer for continuous ICP monitoring. – If ordered by MD, when the ICP reaches a specified pressure, “open” the stopcock to drain CSF for a short time period. • Continuous CSF Drainage/Intermittent ICP Monitoring – The EVD stopcock is “off” to transducer – The amount of CSF drainage is controlled by raising the pressure level on the graduated burette above the Foramen of Monro, which is the zero reference level. The EVD device does not allow practitioner’s to drain CSF and monitor ICP simultaneously. Lumbar Drain Zeroing • There is no such thing • We are not measuring ICP with a Lumbar Drain • No transducer on system • No need for zeroing! (One less thing for you to do!) LD Leveling • The transducer on the set-up is leveled to the patient’s shoulder or iliac crest (per MD order) • The “pressure level” indicator (located on the drip chamber of the collection system) is aligned to the level at which it drains the order volume Iliac Crest ↓ LD Drainage • 1. Draining to a specific volume: MD orders a specific amount of CSF to be drained at a particular time period – Manipulation of the drain to achieve specific amount • 2. Draining at a specific level: MD orders level of the pt’s body – Continuous drainage (ICU monitoring) • 3. Draining at a specific pressure: MD orders a specific pressure for draining – System drains only when the pressure exceeds the pressure pressure – Usually for shunt infections/malfunction – ICU Monitoring Emptying the Buretrol • Measure and record amount of drainage in the Buretrol every hour. • Turn the stopcock at the transducer “off” to patient. • Open the stopcock between Buretrol and the collection bag, fluid should flow from Buretrol into collection bag. • Turn the stopcock between the Buretrol and the collection bag “off” toward Buretrol. • Open the transducer stopcock to patient to obtain readings. Changing the Drainage Bag • The collection bag is changed when about three quarters full. • Wear sterile gloves and a mask. • Cleanse the stopcock below Buretrol with Betadine (Scrub connection for 30 seconds). • Assure the stopcock between the Buretrol and the collection bag is “off” toward Buretrol. • Using sterile handling technique, disconnect the drainage collection bag from the Buretrol stopcock and detach bag from the system panel. (Handing the full bag off to a second person is recommended.) • Connect a sterile replacement collection bag to Buretrol stopcock and attach to system panel. • Cap off the open port of the full collection bag and dispose in red trash bag. Obtain CSF Sample • MD: will obtain CSF cultures from the distal stopcock and is required to use a lab label to label the specimen prior to leaving the patient’s room. • RN is requested to obtain the CSF culture: will be obtained from the specimen collection port on the Buretrol drainage collection chamber. • Equipment: – Non-sterile gloves – Betadine solution/swab/applicator – Sterile gloves – Sterile 10 mL luer-lock syringe – Sterile container (e.g., urine C&S container) – Lab label CSF Collection Cont. • A mask and sterile gloves are required during all CSF specimen collections. • Don non-sterile gloves. • Specimen port is scrubbed with Betadine for 30 seconds. Allow to air dry. • Remove nonsterile gloves and wash hands. • Set up for sterile specimen collection (open and maintain sterility of syringes, specimen container and gloves). • Don sterile gloves. • Attach luer-lock syringe to cleansed and dry needleless access port. • CAUTION: DO NOT insert a needle into the needleless sampling port. CSF Collection Cont. • Turn stopcock OFF to the drainage collection bag and withdraw equal to or greater than 1 mL (absolute minimal sample for microbiology laboratory specimen of 0.5 mL). • NOTE: The hand used to turn the stopcock is no longer sterile; do not touch syringe or specimen container with the contaminated hand. • Maintain sterile technique, remove syringe from the stopcock and expel the CSF sample into the sterile container. • Close container and assure labeling. • Discard syringe in sharps receptacle, discard used supplies. • Send specimen to the laboratory. Dressing Changes Dressings at the ventriculostomy insertion site must remain dry. • Dressings are changed routinely every 72 hours and prn if the dressing becomes damp or otherwise ordered by the physician. • Wearing a mask, cap and gloves, use sterile technique to change the dressing. Use betadine swabs to cleanse the catheter insertion site. • Re-dress the insertion site of the transduced ventricular catheter with a sterile 2x2 dressing and secure with an occlusive dressing. Patient Transport • Clamp the EVD during transport, when repositioning or with any patient movement that would cause the zero point of the EVD/LD to be lower than the reference point. • Re-zero, level and re-open the EVD/LD after patient transport or movement is completed. Waveforms • ICP waveform analysis identify patients who are at risk for increases in ICP and decreases in CPP • The ICP waveform has three components: pulse, respiratory, and “slow waves” • Pulse: consists of three peaks, decreasing in height • Pulse waves represent arterial pulsations in large cerebral vessels as they produce a fluctuation in the volume within the ventricles – P1, the first and sharpest peak, “percussive wave” and results from arterial pressure being transmitted from the choroid plexus. – P2, the second peak, referred to as the“tidal wave,” varies in amplitude with brain compliance – P3 represents the “dicrotic wave” and is caused by closure of the aortic valve Waveforms Cont. • As the ICP increases the amplitude of P1, P2, and P3 all increase – If ICP continues to rise, P2 becomes more elevated than P1 until eventually P1 may disappear within the waveform • Constriction of cerebral blood vessels (Seen with hypocapnia or vasospasm) will exhibit a decrease in the amplitude of the waveform • Patients who have undergone a craniectomy (bone flap removal) will have a dampened waveform Waveforms Waveforms Rounding of ICP waveform due to aneurysmal vasospasm References American Association of Neurosciences Nurses. (2011). Care of the patient undergoing intracranial pressure Monitoring/External ventricular drainage or lumbar drainage. AAN clinical practice guideline series. Glenview, IL: Codman and Shurleff. http://www.aann.org/pubs/content/guidelines.html. Barker, E. (Ed.). (2008). Neuroscience nursing, A spectrum of care (3rd ed.). St Louis, MO.: Mosby Elsevier. Buchbinder, D. (2012). AO Surgical Reference. Retrieved April 18, 2012, from https://www2.aofoundation.org/wps/portal/!ut/p/c0/04_SB8K8xLLM9MSSzPy8xB z9CP0os3hng7BARydDRwML1yBXAyMvYz8zEwNPQwN3A_2CbEdFAEfu4iM!/?show Page=rehabilitation&bone=CMF&segment=Cranium&classification=93Skull+base,+Temporal+bone+(lateral+skull+base)&treatment=&method=Delayed+ management+of+hearing+loss&implantstype=&approach=&redfix_url=128991291 3263. Inova Health System. (2011). Critical care standard 2.400 intracranial pressure monitoring- procedure and protocol. Unpublished manuscript. Wiegand, D. (Ed.). (2011). AANC procedure manual for critical care (6th ed.). St. Louis, MI: Elseview Saunders.