Zeller_Upper Extremity Pain and OMM in Adolescent
advertisement

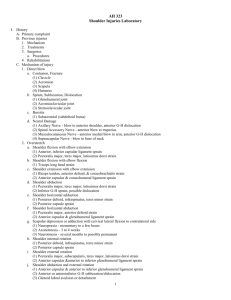
Anne Marie C Zeller, MSc, DO Family Medicine Resident: Year 2 Undergraduate Osteopathic Manipulative Medicine Fellow- Graduated Chief Faculty: Michael P. Rowane, DO, MS, FAAFP, FAAO Discuss common causes and diagnoses in regards to adolescent shoulder and elbow pain Discuss basic tenets of examination of shoulder, elbow, and wrist High-yield and efficient osteopathic manipulative medicine treatments for shoulder, elbow, and wrist Practice , Practice, Practice! MUST consider the maturation of the physis or growth plates Weakness at the physis and decreased resistance to shear and tensile forces compared to the surrounding ligaments, tendons, and muscles, PREDISPOSE this population to injury. • Repetitive micro trauma or overuse mechanisms: 1. Acceleration: Athletes uses optimum load to generate force • Example: racquet and pitching sports 2. Dynamic force: arm is moving against sustained resistance • Example: swimming 3. Static force: action of the shoulder muscles when then are held in a constant position with isometric contraction • Example: dancer or gymnast • Worst position: abducted to 90⁰, externally rotated, and extended. – MOST tension on anterior articular capsule and anterior glenohumeral ligament – Rotator Cuff and deltoid active – Subscapularis is compromised • Accerate forward: pectoralis and subscapularis are required to quickly internally rotate the humerus – ANOTHER bad biomechanical position for shoulder 1) 2) 3) Glenohumeral Joint Sternoclavicular and Acromioclavicular Joints Scapulothoracic Joint Remember: Shoulder Pain is NOT JUST Rotator Cuff! Shoulder involves Ribs, Thoracics, Lumbars, Cervicals, Cranial bones Innominates, and Sacrum Epidemiology, Pathology and OMM treatment • • • Traumatic events makes up 86% of Glenohumeral instability in adolescent athletes 16 and older. Skeletally mature athletes with GH instability = surgery due to 80-90% recurrence rate Skeletally immature athletes = EXTREMELY careful in evaluating because of the high chance of fracture of proximal humerus. 90% of traumatic dislocation Mechanism of Injury: high energy injury of a fall on an outstretched hand while shoulder in abduction and external rotation • S/S: “dead arm”- transient loss of sensation or numbness in involved extremity (axillary nerve), obvious deformity, pt hold arm internally rotated, + anterior apprehension test • Diagnosis: Pt history, physical exam, x-rays • Treatment: Primary- closed reduction of dislocation, Secondary- surgery due to recurrence 8 rate with conservative treatment . • • Hill-Sachs Fracture and Bankart Lesion Hill-Sachs (Blue Arrow): compression fracture at the posterolateral head of the humerus due to impingement against anterior rim of glenoid fossa when the humeral head dislocates. Bankart Lesion (Red arrow): avulsion of anteroinferior glenoid labrum where the inferior glenohumeral ligament attaches • • < 5% of traumatic shoulder dislocations MOI: Fall on an outstretched hand with shoulder in adduction and internal rotation or direct anterior trauma. – Example: Offensive Linemen: forward flexed and internally rotation of shoulder for blocking • • S/S: May not have deformity, + posterior apprehension test, complain of shoulder pain and have limited external rotation with <90⁰ shoulder flexion Treatment: rotator cuff rehab is most successful after closed reduction • • Majority are bilateral, multidirectional Hypermobility (generalized joint laxity) of joints from sports that weaken rotator cuff from overhead motions – Examples: gymnastics and swimming S/S: nonspecific shoulder pain, feeling of shoulder dislocation with overhead activities, hyperextension of other joints of UE, + apprehension signs, + sulcus sign, strength deficits in rotator cuff muscles and scapular stabilizers (serratus anterior, pectoralis, and latissimus dorsi) • Treatment: conservative rehab with strengthening NOT stretching exercises • Proximal humeral epiphysiolysis MOI: repetitive strain injury to proximal humeral epiphysis from overtraining and improper biomechanics seen in over-head sports. (Example: Baseball) • Ages: 11-15 • S/S: • • – Pt has pain in superior lateral aspect of the shoulder with – – – – dynamic/resisted over-head activites palpation of proximal humeral epiphysis is tender active ROM is full and pain free resisted muscle testing in over-head position reproduces pain. X-ray is BEST visualization of pathology Rule out: Fracture and Dislocations with history, physical exam and X-rays or MRI Cautions: chronic dislocations, joint hypermobility, recent shoulder surgery Contraindications: Septic joint, acute dislocation, fracture, cancer 1. 2. 3. Dr. grasps humeral shaft with both hands and fingers interlock on medial side (avoiding NV bundle) Dr. pushes with both hypothenar eminences against humeral shaft. Cause humeral head to become abducted as the humerus is adducted by pt. Pt places his ipsilateral hand on the opposite side of his chest (causing internal rotation and adduction) 4. 5. 6. 7. Pt moves elbow forward and backward (internal and external rotation) Dr. determines which direction enhances balanced tension. Pt is instructed to maintain arm in the position. Dr. fine tunes the tensions at the GH joint to achieve balanced tension. 1. 2. Pt is seated and facing Dr. Dr. places thumbs along superior portion of the clavicles, just distal to the SCM insertion Pt. drapes arms over Dr.’s and flexes head and neck. Allows fingers to sink into the supraclavicular space 3. 4. Pt breathes deeply. During inhalation, the Dr. resists the superior movement of the supraclavicular fasciae During exhalation, the pt. exaggerates flexed posture of head and neck as the Dr. follows tissues as they descend into the thoracic inlet According to Sutherland model, the claviopectoral fascia has a similar role to the interosseous membranes of the forearm and lower leg in that it guides and limits movement of the bone. Serratus anterior, rhomboid and teres major are viewed as the functional ligaments of the joint. BLT treatment presented addresses Serratus anterior, subscapularis, rhomboid, latissimus dorsi, teres major and lower trapezius muscles. 1. 2. 3. Pt seated. Dr. uses thumb as a fulcrum beneath the scapula in the axilla. Palmar surface of thumb is placed on the lateral surface of the 2nd and 3rd rib with the tip facing posteriorly. Anterior to the latissimus dorsi Dr. gently slides her thumb posteriorly along the surface of the rib until it rests between the scapula and rib. 4. 5. 6. Dorsal surface of thumb on subscapularis. Plantar surface of thumb contacts the serratus anterior. Dr. places other hand over the posterior aspect of the scapula. Base of hand at Apex and finger grasp the spine of the scapula Dr.’s posterior hand protract, retract, adduct, abduct, elevate and depress the scapula to achieve balanced tension in all tissues attached OMM Treatment of Ribs, Cranial bones, Cervical Vertebrae, Thoracic Vertebrae, Lumbar Vertebrae, Innominates, Sacrum with S/CS, ME, Indirect Myofascial, Still, or FPR. Extensive information on Throwing and other sport mechanisms in the shoulder and its contributions to shoulder injury and pain ECRL: Extensor Carpi Radialis Longus ECRB: Extensor Carpi Radialis Brevis EDC: Extensor Digitorum Communis ECU:Extensor Carpi Ulnaris CET: Common Extensor Tendon AL: Annular Ligament RCL: Radial Collateral Ligament LUCL: Lateral Ulnar Collateral Ligament 33 Precipitated by activities that require repetitive wrist extension, radial deviation and forearm supination Examples: Hammering, painting, tennis backhand 34 Patient typically reports an insidious onset but will often relate a history of overuse without trauma. Pain with gripping objects (“coffee cup sign) and shaking hands (“politician’s sign”) Numbness or tingling: Suggest radicular symptoms 35 Musculoskeletal and Neurologic Exam 1st! Tenderness with palpation at origin of Extensor Carpi Radialis Brevis (ECRB) Tenderness with resisted supination Resisted Wrist Extension Test Enhanced by: ▪ Straightening elbow ▪ Making a fist ▪ Pronating the forearm ▪ Radially deviating wrist 36 Middle Finger Test Resist the extension of the proximal interphalangeal joint of 3rd digit Stresses the extensor digitorum and ECRB Positive if pain is over the lateral epicondyle. 37 Posterior interosseous nerve entrapment (radial tunnel syndrome) Osteoarthritis Cervical radiculopathy Musculocutaneous nerve entrapment Radiocapitellum Osteochondritis dissecans lesions Lateral collateral ligament strain Stress Fracture Humeral Fracture Synovitis of the radiohumeral joint 38 PL: Planaris Longus PT: Pronator Teres FCR: Flexor Carpi Radialis FDS: Flexor Digitorum Superficialis FCU: Flexor Carpi Ulnaris AL: Annular Ligament MCL: Medial Collateral Ligament 39 Forceful and/or continuous flexion and pronation at the wrist Activities requiring a large amount of stabilization applied by the wrist Common Activities Examples: Racquet sports Swimming Swinging a Golf Club Throwing Computer Keyboard Playing Piano Certain occupations Examples ▪ Carpenters ▪ Plumbers ▪ Meat cutter 40 Pain and tenderness along medial elbow extending into forearm Difficulty gripping without pain Decreased wrist strength Tightness/stiffness when stretching elbow and wrist 41 Testing for Valgus Stability in Extension: MCL Anterior Capsule Bony articulations 42 Fracture Osteochondritis dissecans Osteoarthrosis MCL injury Little League elbow- increased valgus angle in adolescent throwing athletes Flexor-Pronator Strain Ulnar neuropathy (neuritis, entrapment) Pediatric- avulsion fracture 43 44 45 Diagnose and treat Somatic Dysfunctions in: Cervical spine, Thoracic spine, Ribs , Scapula, and Clavicle To reduce and/or correct somato-somatic reflexes and some of the myofascial pain referrals To improve the venous and lymphatic drainage OMT Techniques Presented Address: Radial Head Humero-Radial Joint Humero-Ulnar Joint Distal Radio-Ulnar Joint Carpal Joints Patient seated with elbows flexed at 900 and forearms at 00 of pronation and supination (thumbs up). Then check for supination or pronation restrictions. The radial head moves posteriorly with pronation and anteriorly with supination. Therefore a pronated forearm (with restricted supination) will have a posterior radial head somatic dysfunction. Supinated forearm (with restricted pronation) will have an anterior radial head somatic dysfunction. Example: Pt is restricted in PRONATION, Freedom of Motion is in Supination Diagnosis: Anterior Radial Head 50 Step 1 Step 2 Step 4 Step 3 *Sit next to patient as depicted to make this work * Start in full Pronation and end in full Supination 51 Step 1 Step 2 Mobilization of distal radioulnar joint – – – – isometric; to 4th barrier in pronation, repeat in supination Treat restrictions of pronation/supination (proximal or distal) *Piano key sign Free-up the interosseous membrane* Improve venous and lymphatic return • (carpal tunnel syndrome) 52 Patient is supine Right arm abducted 45 degrees Hand positioned midway between supination and pronation (thumb up towards ceiling). Both hands are placed around the elbow and motion is medial and lateral to produce the articulation of the radial head with the ulna or humerus or articulation of the humeroulnar joint. **Examine for Valgus/Varus instability before performing technique 53 •Fingers should be applying lateral traction to the thenar & hypothenar eminences and the thumbs should be applying pressure to gently separate the ulna and radius from the carpal bones •Wrist Flexion, Extension, Radial and Ulnar Deviation 54 Anterior Tender Points 55 Elbow is flexed fully. Forearm is pronated and arm is internally rotated - so back of hand approximates chest. Forces are pronation of the forearm and internal rotation of the humerus until a position of comfort is found. Hold this position for 90 seconds and then slowly return to neutral. Retest for tenderness. Coronoid TP- Same position but external rotation of the humerus 56 ALWAYS perform a musculoskeletal and neurologic exam FIRST OMT learned today for shoulder and elbow Glenohumeral Joint Sternoclavicular and Acromioclavicular joint Scapulothoraic joint Radial Head Humero-Radial Joint Humero-Ulnar Joint Distal Radio-Ulnar Joint Carpal Joints 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) Wojtys E. et al. “Sports injuries in the immature athlete.” Orthop Clin North Am 1987; 18 (4): 689-708. Ogata et al.early development and ossification of the human clavicle—an embryologic study.1990, Vol. 61, No. 4 , Pages 330-334 Gardner E.”The embryology of the clavicle.” Clin Orthop 1968;58:9 Carreiro, Jane D.O. Pediatric Manual Medicine. (2009). Churchill Livingstone. BRIAN L. MAHAFFEY, M.D.PATRICK A. SMITH, M.D. “Shoulder Instability in Young Athletes.” American Family Physician Lawton RL et al. “Pediatric shoulder instability: presentation, findings, treatment, and outcomes.” J Pediatric Orthop 2002.; 2252-61. Good CR et al. “Traumatic shoulder dislocation in the adolescent athlete: advances in surgical treatment.” Curr Opin Pediatr 2005; 17:25-9. Jakobsen BW et al. “Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up.” Arthroscopy 2007; 23 (2): 118-23. Krabak et al. “Shoulder and Elbow Injuries in the Adolescent Athlete.” Phys Med Rehabil Clin N Am. 19 (2008) 271-285. American Osteopathic Association. Foundations in Osteopathic Medicine. (2003) 11. 12. 13. 14. 15. 16. Young et.al (2011) “Lateral Epicondylitis.” 5-minutle Sports Medicine Consult. Lippincott Williams & Wilkins. Zeisig E. et al.(2006) Extensor origin vascularity related to pain in patients with Tennis elbow. Knee Surg Sports Traumatol Arthrosc.14(7):659. Walz D, et al (2010). Epicondylitis: Pathogenesis, Imaging, and Treatment. Radiographics. 30: 167-184. Gruchow (1979). “Epidemiologic Study of Tennis Elbow. Incidence, recurrence, and effectiveness of prevention strategies”. American Journal of Sports Medicine. 7(4): 234238. Young et.al (2011) “Medial Epicondylitis.” 5-minutle Sports Medicine Consult. Lippincott Williams & Wilkins. Smidt, N. et al (2002). “Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomized controlled trial.” Lancet. 359: 657-662. 59 17. Bisset L, et al. (2005) “A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. British Journal of Sports Medicine. 39: 411-422. 18. Grewal R. (2009) “Functional outcome of arthorscopic extensor carpi radialis brevis tendon release in chronic lateral epicondylitis.” Journal of Hand Surgery. 34: 849-857. 19. Des Moines University OMM Department. “Treatment of Elbow Somatic Dysfunctions Laboratory Handout.” Updated 2010. 20. Figueroa J. Professional collaboration with AOA Lateral and Medial Epicondylitis Lecture. 21. Lewis D. Upper Extremity IV Lab and Lecture. Spring 2011. Des Moines University. 22. Simons DG, Travell JG, Simons LS. Myofascial Pain and Dysfunction: The Trigger Point Manual. Volume 1. Upper Half of Body. 2nd Ed. Baltimore, Williams & Wilkins, 1999, pp. 485907 60 Spencer Sequence Step 1: Extension Isometric Contraction the patient is trying to flex shoulder is used to lengthen the Pectoralis Major, Pectoralis Minor and anterior deltoid Spencer Sequence Step 2: Flexion Isometric contraction of Patient extending shoulder engages latissimus dorsi, teres major and minor, posterior deltoid Spencer Sequence Step 3: Circumduction without traction Spencer Sequence Step 4: Circumduction with Traction Spencer Sequence Step 5: Abduction Isometric Contraction of patient adduction engages Pectoralis Minor, Teres Minor, and Infraspinatus Spencer Sequence Step 6: Adduction Isometric contraction of patient pushing elbow superior engages subscapularis and teres major Spencer Sequence Step 7: Internal Rotation Isometric contraction pt. pushes elbow posterior (external rotation) engages the supraspinatus and infraspinatus muscles Spencer Sequence Step 8: Abduction with Resisted Traction Structures referring to the lateral elbow Scalenes Supraspinatus Teres Minor Deltoid Triceps Subclavius Pictures of Trigger Points, Referral Patterns, and Stretches in Appendix of Powerpoint Slides Lateral and Medial Epicondylitis- Anne Marie C. Zeller 70 Structures referring to the medial elbow Latissimus Dorsi Subscapularis Triceps Sternalis Serratus Posterior Superior Pictures of Trigger Points, Referral Patterns, and Stretches in Appendix of Powerpoint Slides Lateral and Medial Epicondylitis- Anne Marie C. Zeller 71 Identify the trigger points: Taut band Tender to palpation Recognition of Pain Referral of pain (“triggers pain somewhere else”) Treat by stretching May use spray and stretch Treat by needling Dry needle or infiltrate trigger point with lidocaine Lateral and Medial Epicondylitis- Anne Marie C. Zeller 72 73 74