Brain Failure Matthew J. Beelen, MD Geriatric Specialists Lancaster
advertisement
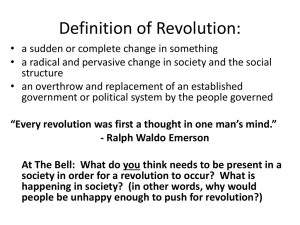
Brain Failure: Prevention, Assessment, and Management of Delirium in Older Hospitalized Individuals Matthew J. Beelen, MD Geriatric Specialists Lancaster General Health June 18, 2013 Case 79 year old man, baseline mild cognitive impairment (MCI) CABG in July 2012 Post-operative delirium “mild bouts of confusion” post op “confusion, delusions, and hallucinations” “impulsive” To rehab facility Confusion gradually improved Case, continued Returned home – since then: No longer able to manage finances No longer able to manage medications Confusing dates and appointments Failed driving test (wife does not drive) Unable to continue working part time Depressed Wife distressed about his decline, his repeating, his depression Almost 1/3 of hospitalized elderly will develop delirium Learner Objectives Articulate the significance of delirium Recognize and identify delirium promptly as it occurs Describe approaches to delirium prevention and incorporate these into Compare approaches to delirium management and incorporate these into practice. What is Delirium? A disturbance in consciousness that: Has acute onset (hours to days) and fluctuates over the course of the day Involves reduced ability to focus, sustain, or shift attention Involves a change in cognition (memory, orientation, language, etc) or perception (hallucinations) Is associated with an underlying medical etiology APA; DSM-IV, 1994 Inflammatory Model of Delirium Marcantonio ER, JAMA . 2012;308:73-81. Delirium Subtypes Hyperactive Agitation Increased vigilance Hallucinations Hypoactive Somnolent, lethargic, stupor, coma, decreased psychomotor activity Often unrecognized 75% of cases in the elderly Associated with higher mortality Delirium or Dementia? Delirium Dementia Time Pattern Acute changes and fluctuation during the day Chronic and gradual, possible changes in response to environment, fatigue (“sundowning”) Level of Consciousness Often altered Alert Attention Impaired Usually intact unless severe dementia Speech Incoherent, disorganized Ordered, anomic/aphasic Dementia and delirium often coexist What is the patient’s baseline? Identification: Confusion Assessment Method Feature 1: Acute change and fluctuating course of mental status And Feature 2: Inattention And Feature 3: Altered level of consciousness Inouye, et. al. Ann Intern Med 1990; 113:941-948.1 Or Feature 4: Disorganized thinking Confusion Assessment Method (CAM) 86-94% sensitive, 89-93% specific Validated in over 1000 patients Used in over 250 original published studies 28 page training manual… Improved accuracy with formal training Improved accuracy when using a standard cognitive screen as part of the CAM (Modified Mini-Cog) Takes about 5 minutes to perform http://hospitalelderlifeprogram.org Modified Mini-Cog Assessment Orientation 1. Time: Day, Year, day/night, last meal, how long in hospital. 2. Place: City/State, Hospital, Floor Registration 3. Name 3 objects: (apple, watch, penny) Clock-drawing Ask the patient all 3 after you have said them. Repeat until all 3 are learned 4. Draw a circle, draw numbers, and place hands at “ten past eleven” Recall 5. Ask for 3 objects in question 3 http://hospitalelderlifeprogram.org Identification in the ICU: CAM-ICU Assesses same domains as CAM Different questions/methods of assessment used Ideal for non-verbal patients Incorporates the Richmond Agitation and Sedation Scale (RASS) To decide if patient can be assessed for delirium To assess level of consciousness www.icudelirium.org; Ely EW et al, JAMA. 2001;286:2703-2710. CAM-ICU: RASS www.icudelirium.org Identification Using CAM-ICU 93-100% sensitive, 89-100% specific Validated for ventilated and non-ventilated critically ill patients 28 page training manual… Takes about 5 minutes to perform Recommended to be done every shift Evidence of benefit? www.icudelirium.org; Ely EW et al, JAMA. 2001;286:2703-2710. The Role of CAM and CAM-ICU Evidence of benefit of screening is lacking “We cannot manage delirium or decrease its complications unless we recognize it” Useful as a means to monitor for delirium as part of QI process Delirium is Common 100% 90% 80% 70% 60% Maximum Minimum 50% 40% 30% 20% 10% 0% ED Admission Gen Med Post Op ICU DC to ECF Prevalence of Delirium at Various Points of Hospitalization Delirium Has Significant Impacts For patients while in the hospital For patients after they leave the hospital For society Population management Impact in the Hospital physical function nutrition post-op complications (2-5x risk) self-extubation or removal of lines death: 22-76% mortality rate (10-fold risk) Inouye SK. N Engl J Med 2006;354:1157-65 Marcantonio ER. JAMA 2012;308:73-81 pneumonia falls pressure ulcers exposure to physical and chemical restraints family distress burden on nurses and patient care staff Impact Post-Hospitalization 3-fold increased risk of institutional placement at discharge 2-fold risk of 30-day readmission from ECF Death 3 fold risk of death at 6 months Every day an ICU patient spends in delirium increases risk of death at 6 months by 10% 1 year mortality rate is 35-40% Risk of higher mortality persists for up to 2 years Inouye SK. N Engl J Med 2006;354:1157-65 Marcantonio ER. JAMA 2012;308:73-81 Ely EW et al. JAMA 2004;291:1753-1762 Marcantonio ER et al. J Am Geriatri Soc 2005;53:963-969 Impact Post-Hospitalization Worsening cognition in those with pre-existing cognitive impairment Patients with Alzheimer’s who develop delirium: Rate of cognitive decline is doubled in the year after delirium compared to those without delirium More rapid rate of decline persists for 5 years Gross AL et al. Arch Int Med 2012;172:1324-1331 Fong TG et al. Ann Int Med 2012;156:848-856 Fong TG et al. Neurology 2009;72:1570-1575 Delirium and Cognitive Decline Saczynski JS et al. N Engl J Med 2012;367:30-39 Impact Post-hospitalization New cognitive impairment: Greater then 10-fold increase risk in new development of dementia over the next 4 years Cognitive reserve theory Witlox J et al. JAMA 2010;304:443-451. Cognitive Reserve and Delirium delirium Impact on Society Increased length of stay 2-5 days longer than those without delirium Increased ICU and ventilator days Increased costs of care $60,000 incremental costs over the following year $6.9 billion annual cost to Medicare to treat delirium Impact on caregiver burden Assistance with activities of daily living Emotional impact Marcantonio ER. JAMA 2012;308:73-81. O’Mahony R et al. Ann Intern Med 2011;154:746-751. Delirium - Cost to Society Monthly Health Care Costs After Discharge from Hospital Leslie DL. Arch Int Med 2008;168:27-32 Approach to Delirium Prevention Recognize Risk Reduce Risk Prevention of Delirium “At least 30-40% of cases may be preventable. Prevention is the most effective strategy for reducing delirium frequency and complications.” (Inouye, 2006) “We should not wait for delirium to happen but must work to implement proven interventions that prevent delirium” (Ely, 2012) “Effective strategies that prevent delirium should be a high priority for health care systems.” (O’Mahony, 2011) Risk Factors for Delirium Inouye SK. J Geriatr Psychiatry Neurol 1998;11:118-125. Predisposing Factors Baseline cognitive impairment*** Vision Impairment Hearing Impairment Older age Low educational level ADL impairment From ECF Depression Alcohol abuse Multiple significant chronic conditions High numbers of home medications Use of opioids or benzodiazepines prior to admission Predisposing Factors Dehydration Bun/Cr > 18 Severe Illness on Admission Sepsis/SIRS/infection Acute organ failure Electrolyte/metabolic Acute cardiac event Stroke/seizures Malnutrition Surgical patient Hip fracture Fracture/trauma Prior stroke Parkinson’s Prior delirium* Predictive Value of Risk Factors 4 predisposing risk factors (low vision, cognitive impairment, dehydration, severe illness) Initial Initial Validation Validation # of RFs Risk Group Rate (%) RR Rate (%) RR 0 Low 9 1.0 3 1.0 1-2 Intermediate 23 2.5 16 4.7 3-4 High 9.2 32 9.5 83 “Primary prevention of delirium should address important delirium risk factors and target patients at intermediate to high risk for delirium at admission.” Inouye SK. J Geriatr Psychiatry Neurol 1998;11:118-125 Precipitating Factors Derangements in Normal Functions: Fluid intake Bladder Acid/base emptying Electrolyte Nutrition intake Bowel New Acute Conditions: Metabolic movements Glucose Oxygen intake CO2 release Sleep/wake cycle Mobility Anemia Infection/fever CNS event/condition Cardiac event/condition Hypotension/shock Precipitating Factors Extrinsic Factors Procedures / Surgery Ventilators / ICU Tubes, lines, catheters, restraints, devices Environment change Other Symptoms Pain Emotional Distress Medications >3 added the previous day “polypharmacy” Benzodiazepines Anticholinergics ETOH or drug withdrawal Opioids (+/-) Prevention Strategies Prevention should focus on those at intermediate to high risk Effective prevention must address the complex array of precipitating risk factors Limited evidence of benefit for isolated interventions Prevention requires cooperative interdisciplinary effort Multi-Component Interventions Methods and specific interventions vary widely Reston JT and Schoelles KM. Ann Intern Med. 2013;158:375-380. Hospital Elder Life Program (HELP) Age ≥ 70 on a general medicine unit, ≥1 risk factor (impaired cognition, elevated BUN/Cr ratio, vision impairment, severe illness) = medium to high risk Additional risks assessed in the first 48 hours: Sleep deprivation: interview and nurse input Immobility: ADL assessment scale Hearing impairment: Whisper test Initial and daily assessment for delirium: CAM Inouye SK et al. N Engl J Med 1999;340:669-676 The HELP Team Elder Life Nurse Specialist – Masters level with geriatric training and experience Elder Life Specialist/Volunteer Coordinator Performs screening, develops care plans, oversees and coordinates volunteers, training, data collection Masters level with experience with human services or healthcare, geriatrics, supervisory experience Geriatrician Program Director (may be one of the above) Volunteers (3-4 hours, 1-2 times per week) Inouye SK et al. N Engl J Med 1999;340:669-676 HELP - Intervention What did the HELP Team do? Performed initial and ongoing assessments Administered a set of care protocols for at-risk patients Targeted Provided 6 risk factors for delirium ongoing staff education Led interdisciplinary meetings and rounds Led ongoing CQI process HELP Interventions for 6 Risk Factors Targeted Risk Factor Cognitive impairment Sleep deprivation Immobility Visual impairment* Hearing impairment* Dehydration* Standardized Intervention Orientation & therapeutic activity protocol (discuss current events, word games, reorient, etc) Sleep enhancement & nonpharm sleep protocol (noise reduction, back massages, schedule adjustment) Early mobilization protocol (active ROM, reduce restraint use, ambulation, remove catheters) Vision protocol (glasses, adaptive equipment, reinforce use) Hearing protocol (amplification devices, hearing aids, earwax disimpaction) Dehydration protocol (early recognition of dehydration & volume repletion) HELP Outcomes – Original Study 852 patients Delirium incidence 9.9% intervention 15% controls Inouye SK et al. N Engl J Med 1999;340:669-676 Decrease in total number of days of delirium Subsequent HELP Outcomes Disseminated to sites worldwide Less functional and cognitive decline, falls, and pressure ulcers during hospitalization Little impact on delirium severity once it occurred* Cost effectiveness has been demonstrated Cost savings to hospitals has been demonstrated Improves geriatric education within the hospital Volunteer use benefits the community Implementation support is available Inouye SK et al. J Am Geriatr Soc 2000;48 Rubin FH et al. J Am Geriatr Soc 2011;59:359-365. General Prevention Recommendations Early risk assessment and develop plan to address risk factors Plan carried out by competent interdisciplinary team Minimize staff and location changes Orienting interventions Familiar visitors O’Mahony R et al. Ann Intern Med 2011;154:746-751. Treat pain Minimize infection risk Optimize: hydration and nutrition bowel/bladder function oxygenation activity and mobility medications sensory input sleep Prevention - Interdisciplinary Team The Health System Nurses Pharmacist Physicians Patient Physical Therapist Balas MC et al. Crit Care Nurse 2012;32:35-47 Respiratory Therapist Barriers to Optimal Prevention Culture change is needed – proactive vs. reactive System change is required To ensure interdisciplinary team coordination QI processes related to key components of prevention Initial assessment Development of management plan Completion of individual components of plan Monitoring for delirium for early detection and for monitoring effectiveness of program Institutional support (“buy-in” and resources) Treatment of Delirium Management of Delirium There is little rigorous evidence of benefit Non-pharmacologic measures show a trend toward: Shorter duration of delirium Decreased severity Shortened hospital LOS Medications: as of 2011 there was only one randomized placebo-controlled trial – it showed no difference in outcomes So what can we do? Flaherty JH. Med Clin N Am 2011;95:555-577. Management – Team Approach Communicate the diagnosis To team members To family In the medical record: “encephalopathy” - $$ irony Multi-factorial assessment of precipitating factors Management plan to address these factors Sound familiar? Brain Failure: serious problem, possible emergency Immediate attention is crucial Review Precipitating Factors Derangements in Normal Functions: Fluid intake Bladder Acid/base emptying Electrolyte Nutrition intake Bowel Acute Illnesses: Metabolic movements Glucose Oxygen intake CO2 release Sleep/wake cycle Mobility Anemia Infection/fever CNS event/condition Cardiac event/condition Hypotension/shock Review Precipitating Factors Extrinsic Factors Procedures / Surgery Ventilators Tubes, lines, catheters, restraints, devices Environment change Other Symptoms Pain Emotional Distress Medications >3 added the previous day “polypharmacy” Benzodiazepines Anticholinergics ETOH or drug withdrawal Opioids (+/-) Management – Focus on Safety Environment Optimize orientation, comfort, sleep/wake cycle 1:1 supervision or “sitter” Family or friend presence Is a room or unit change indicated? “Don’t neglect the hypoactive” For severe distress or risk of harm to self or others Consider medication Consider restraints – the least necessary Treatment With Medications Limited, small studies Only 1 with a blinded placebo comparison group Underlying dementia either not mentioned or was used as exclusion criteria in most studies Delirium subtypes were not accounted for No clear evidence that medications decrease severity or shorten duration No clear evidence that newer antipsychotics are more favorable than haloperidol People with delirium get better without medications… Seitz DP et al. J Clin Psychiatry 2007;68:11-21. Campbell N et al. J Gen Intern Med 2009;24:848-853. Flaherty JH et al. J Am Geriatr Soc 2011;59:S269-S276. Treatment with Medications No FDA approved medications for delirium Haloperidol 0.25-0.5mg PO Q4 hours PRN 0.5-1.0mg IM q30-60min IV doses have much shorter duration of action: q60min Atypical antipsychotics – oral Risperidone 0.25mg-0.5mg Q12-24 hours Olanzapine 2.5-5.0mg Q12-24 hours Quetiapine 12.5-25mg Q12-24 hours Treatment With Medications Antipsychotics Can prolong the QT interval (get baseline EKG) Can cause parkinson-like symptoms at high doses Can cause worsening or irreversible decline in Parkinson’s or Lewy Body dementia Quetiapine If is thought to be best choice for these conditions used – start with low end of dose range Benzodiazapines 2nd line or last resort (unless alcohol withdrawal) Can induce, worsen, or prolong delirium Final Case Nov. 2012: 87-year-old woman admitted to hospital from nursing home with mental status change, tachycardia, tachypnea, fever. Baseline MCI. 3 day hospital stay E coli UTI New onset Atrial fibrillation, fluid overload / CHF NSTEMI Confused, lethargic, “encephalopathy” Discharged to nursing home “comfort care, hospice consult, NPO” Now – back to baseline! Summary Delirium has significant impacts, especially after discharge Watch for the hypoactive subtype We may be able to prevent 1/3 of cases Prevention is the best treatment Effective prevention and treatment requires a careful assessment for risk factors and a plan to minimize them – culture and system change Medications: limited role Questions?