Biomedical Waste - India HIV/AIDS Resource Centre
advertisement

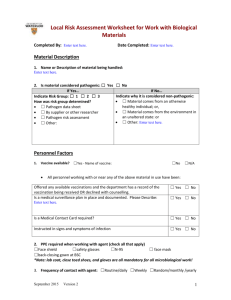
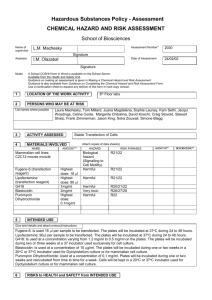
BIOSAFETY IN BTS Learning Objectives • Identify Biosafety Issues in the BTS work areas • List the key requirements for the safe disposal of biological and chemical waste Definition • The use of lab practices and procedures and equipments for safety when working with potentially infectious microorganisms. Why Biosafety Practices? Protection of• Workers • Products • Co workers • Lab support personnel • Environment • Regulatory requirements Risk of occupational transmission of infection depends on • Prevalence of infected individuals in the population • The frequency of exposure to contaminated medical instruments • The relative infectivity and concentration of the virus • If there is an exposure to a large quantity of blood Risk of occupational transmission of infection depends on ( Contd..) • Deep needle stick injury • Injury with hollow bore needles • Patient samples positive for TTIS Infectious risk to HCWs From Percutaneous Exposure Rule of 3’ HIV HCV HBV - 0.05 to 0.3% 3.0 to 10% 10 to 30% Others at Risk Municipal workers Ragpickers Community Viral Load in Circulation • HIV – 10 to 100 viral particles/ml • HCV- 10,000 to 100,000 viral particles/ml • HBV- 10,000,000 viral particles/ml Modes of Exposure to Blood Pathogens in the Laboratory Lab procedure HCW at risk Source of transmission Collection of blood/body fluids Doctors/Laboratory technician/Nursing staff Needle stick injury, broken specimen container, blood contamination of hand with skin lesion/breach Transfer of specimen /blood unit Laboratory technician and transport worker Contaminated exterior of the container/ requisition slip Processing of specimen /blood unit Laboratory personnel Puncture of skin or contamination of skin/mucous membrane from Contaminated work surface Spill/splash of specimen container Faulty techniques Modes of Exposure to Blood Pathogens in the Laboratory, contd Lab procedure HCW at risk Source of transmission Cleaning /washing Support staff Disposal of waste Laboratory Contact with infectious personnel support waste specially sharps staff Transport to Transport/postal distant staff laboratory/hosp ital Puncture/contamination of skin from Contaminated glassware Sharps Contaminated work surface Broken/leaking container Interruption of Transmission • Barriers • Disinfection • Vaccination • Post exposure prophylaxis • Safe biohazardous waste disposal Good Lab Practices • General rule - all samples be treated as potentially infectious Universal precautions are those consistently used by all HCW • Universal precautions are to be consistently used by all HCW General Lab Hygiene • Cleaning of work surfaces and equipment with suitable disinfectant • Restricted entry to work areas. • Avoid eating, drinking in the labs. • Avoid mouth pipetting. • Use laminar air flow hoods where necessary. Universal Precautions • BARRIER PROTECTION • HAND WASHING • SAFE TECHNIQUES • SAFE HANDLING OF SHARP ITEMS • SAFE HANDLING OF SPECIMEN (blood etc.) UNIVERSAL PRECAUTIONS (contd.) • SAFE HANDLING OF SPILLS OF BLOOD/BODY FLUID • USE OF DISPOSABLE/ STERILE ITEMS • SAFE TECHNIQUES -MECHANICAL PIPETTING DEVICE • IMMUNISATION WITH HEPATITIS B VACCINE BARRIER PROTECTION • • • • Gloves Plastic aprons/ Lab gowns Masks Occlusive bandages Gloves • Wear well fitting disposable vinyl gloves • Change gloves if torn or visibly contaminated with blood • remove gloves before handling door knobs, telephones, pens, leaving the lab Laboratory gowns • Should be worn when in the lab. and should be removed before leaving. • Use plastic aprons while cleaning re-usables and disposing waste. Facial protection • Cheap deflector masks or protective glasses should be used if splashing of sample is expected. Occlusive bandage • Cover all cuts and breaks with wash proof bandage before patient care. HAND WASHING • • • • • WASH THROUGHLY WITH WATER AND SOAP IMMEDIATELY - AFTER CONTAMINATION WITH BLOOD/BODY FLUIDS. AFTER REMOVING GOWN/GLOVES. BEFORE EATING, DRINKING & LEAVING THE LAB. LABS SHOULD BE PROVIDED WITH LIQUID SOAP DISPENSERS. USE MOISTURISING HAND CREAM AFTER EVERY HAND WASH. GLOVES ARE NOT A SUBSITUTE FOR HAND WASHING Safe Handling Techniques in Lab • Centrifuge tubes with safety caps should be used SHARPS: • Do not bend/ break/ recap/ manipulate or remove needles from disposable syringe. • Extreme care should be taken to avoid auto-innoculation. • Chipped/broken glassware should be disposed off in appropriate containers. • Don’t use hands to pick up broken glass. SAFE HANDLING OF SPECIMEN • Collect samples in sterile screw cap plastic containers. • Seal properly to prevent spill/leakage. • Use sterile disposable syringes and needles/vacutainers. Cover cuts with waterproof bandages. • Transfer leaked samples to fresh container, rewrite patient information on the new container. • Reject requisition slip contaminated with blood or handle using gloves in case of emergency. Safe Handling of Spills IN CASE OF BLOOD SPILLS • COVER THE AREA WITH PAPER TOWELS OR GAUZE SPONGES TO ABSORB THE LIQUID. • Cover the spill AREA WITH DISINFECTANT SOLUTION . (0.5-1 % Sodium Hypochlorite –freshly prepared). - LEAVE IT FOR 30 MIN - With 4% hypochlorite solution leave for 10 minutes. • WASH THE AREA THROUGHLY WITH SOAP AND WATER. • CONTAMINATED MATERIAL TO BE DISPOSED OFF AS INFECTIOUS WASTE. Prompt Accident Management • Spillage • Rupture of blood bag in the centrifuge, breakage of tubes. • Leakage of blood bag in transport containers. • Needle stick injury; blood splashes Biomedical Waste • Biomedical Waste means any waste, which is generated during diagnosis, treatment or immunization of human beings or animals or in research activities pertaining thereto or in the production or testing of biologicals and including categories mentioned in Schedule I Biomedical Waste Management • Improper disposal / treatment of un-segregated and segregated medical waste is a potential hazard affecting the health of the patients, health care workers, the community as well as the environment. • A notification regarding Biomedical Waste (Management & Handling) Rules,1998 has been published by the Ministry of Environment & Forests. Safe Disposal • • • • Segregation Disinfection Storage Disposal Biomedical Waste (management and handling ) Rules, 1998 Ministry of Environment and Forests. GOI Amendment of the Rules is under process Categories of Bio-Medical Waste Option Waste category Treatment & disposal Category 1 Human anatomical waste Incineration/deep burial Category 2 Animal anatomical waste Incineration/deep burial Category 3 Microbiology & Biotechnology waste Local autoclaving/ microwaving/ Incineration Category 4 Waste sharps Disinfection (/autoclaving/ microwaving and mutilation/shredding Category 5 Discarded Medicines and Cytotoxic drugs Incineration/destruction and drugs disposal in secured landfills Category 6 Solid waste (items contaminated with blood and body fluids) Incineration autoclaving/microwaving Categories of Bio-Medical Waste Contd… Option Category of waste Treatment Category 7 Solid waste (Tubings, catheters, intravenous sets etc.) Disinfection by chemical treatment autoclaving /microwaving and mutilation/ shredding Category 8 Liquid waste Disinfection by chemical treatment and discharge into drains Category 9 Incineration Ash Disposal in municipal landfill Category 10 Chemical waste Chemical treatment and discharge into drains for liquids and secured landfill for solids Colour Coding &Type of Container for Disposal of Bio-Medical Wastes Color coding Type of container Waste category Treatment options as per schedule I Yellow Plastic bag Cat 1, Cat 2, Cat 3, Cat 6 Incineration/deep burial Red Disinfected container/plastic bag Cat 3, Cat 6, Cat 7 Autoclaving/microwavi ng/ chemical treatment Blue/white translucent Plastic bag/puncture proof container Cat 4, Cat 7 Autoclaving/microwavi ng chemical treatment and destruction/shredding Black Plastic bag Cat 5 and Cat 9 and Cat 10 (Solid) Disposal in secured landfill Disinfection • Reduction in the number of pathogenic microbes so that the material/object/surface becomes safe for handling • Advantages of Na hypochlorite – – – – Bactericidal Virucidal Easily available Affordable • Disadvantages – Corrodes metal – Deteriorates rapidly Disinfection of Glassware Blood/plasma/serum/fluids in glass containers - Sample vials - Test tubes • Discard in plastic bins containing 1% sodium hypochlorite ( 10, 000 ppm chlorine) Disinfected blood/fluids Glassware treated in chromic acid Wash down with running tap water Dry in hot air oven ( Temp 160C)Wash thoroughly Blood and Blood Products in Plastic ware – – – – – – Blood bags Autoclave Tubings of bags Microtips Plastic vials Microplates Used blood bags disposal Immerse in 1% Na Hypochlorite for 30 minutes Shredding Safe Disposal of Sharps • Dispose off your own sharps. • Discard needles in puncture -proof rigid containers after disinfection in 0.5-1% fresh sodium hypochlorite solution. • Don’t dispose in any other container. • Dispose when container is 3/4 full. Autoclave • Saturated steam under pressure is used to decontaminate infectious material. • It consists of a insulated pressure chamber in which saturated steam is used to elevate the temperature • A pressure of 15psi at 121oC for 30 minutes is required • Adequacy of disinfection to be checked with strips of B. Stearothermophilus. Issues of Concern – Regular sensitization • Adequate resources – Regular availability of supportive items • Monitoring mechanisms – Indicators To Health Care Workers and Community