Leishmania
Leishmania
introduction
.
protozoal disease of mammals, a zoonotic disease.
. 23 + pathogenic species.
.
transmitted by sandflies (Phlebotomus species).
.
in the human host, Leishmania infect the mononuclear phagocytes.
Leishmania
Species pathogenic in humans:
☆ leishmania donovani
(complex)
☆ leishmania tropica
☆ leishmania major
☆ leishmania mexicana
(complex)
☆ leishmania brazilliensis
(complex)
☆ leishmania aethiopica
Leishmaniasis
introduction
To be categorized into 3 types, as follows:
. Visceral leishmaniasis (VL), also known as kala azar, is caused by L. donovani, is the most severe form of the disease, which, if untreated, has a mortality rate of above 90%.
.
Cutaneous leishmaniasis (CL) can produce large numbers of skin ulcers. It is caused by L. tropica and L. mexicana.
. Mucocutaneous leishmaniasis (MCL), or espundia, is caused by L. braziliensis, produces lesions of mucous membranes of the nose, mouth and throat cavities
.
leishmania donovani
Morphology
1. Amastigote
2. Promastigote
(Leishman-Donovan body ) living in the reticuloendothelial system
(mononuclear cell / macrophage) of man and reservoir mammals.
(liver, spleen, lymph node, bone marrow, skin)
Morphology
1. Amastigote
The ultrastructure of amastigote
Morphology
1. Amastigote
2. Promastigote in the sand fly and in cultures
Morphology
. Amastigote . Promastigote
.Mammalian stage .insect (sandfly)
.Non-motile .motile
.Intracellular .midgut
(macrophages)
The vector----- sandfly
.Adult sandflies are only 1.5-
4 mm long, and yellow in color.
.Hairy bodies.
.Wings are held erect over the body.
.Belonging to the genera
Phlebotomus and Lutzomyia .
.Of 500 known phlebotomine species, only about 30 of them have been positively identified as vectors of the disease.
Life cycle binary fission amastigote the female sandfly sucks blood of human or mammalian host promastigote migrate to the pharynx and buccal cavity promastigote
Enter the mid gut amastigote binary fission
Macrophage rupture, invade fresh cells amastigote the female sandfly bite human or mammalian host
Life cycle of Leishmania
the female sandfly sucks blood buccal cavity the female sandfly bite
Summary:
1. Infect stage: the promastigote form
2. The vector: sandfly
3. Methods of transmission : the bite of sandfly
4. Host: humans , dogs, wild rodents ,
the female sandfly sucks blood buccal cavity the female sandfly bite
Summary:
5. Parasite spread: macrophage lysis→amastigote release.
via blood spead lymphatic spread
6. Reside site: the cells of the reticuloendothelial system
(skin, liver, spleen, lymph node, bone marrow)
Pathogenesis
① Amastigote forms destroy macrophages
→hyperplasia → lead to hepatosplenomegaly.
② Bone marrow turns hyperplastic, and parasitized macrophages replace the normal hemopoietic tissue.
pancytopenia .
Oligocythemia of red blood cells,
Leucopenia, Normal value
Thrombocytopenia
RBC : 3.5-5.0
╳
10 12 /L, 4.0-5.5
╳
10 12 /L
WBC : 4,0-10
╳
10 9 /L
Blood platelets : 100-300
╳
10 9 /L
Pathogenesis A ) normal value
: 40-50g/L
Globulin( G ) normal value
: 20-30g/L
① Amastigote forms destroy macrophages →hyperplasia → lead to hepatosplenomegaly.
A/G normal value
: 1.5 -- 2.5:1
② Bone marrow turns hyperplastic, and parasitized macrophages replace
A/G reversal : pancytopenia .
③ leishmanial antigens stimulate immune system an overproduction of both specific immunoglobulins and nonspecific immunoglobulins also occurs a reversal of the albumin-globulin ratio.
Clinical features
1. Visceral leishmaniasis ( Kala-azar )
① is caused by L. donovani.
② The incubation period: 3-6 months (months or years).
③ Main symptoms :
.
An insidious onset with irregular lowgrade fever.
. Hepatosplenomegaly.
. Lymphadenopathy.
. Anemia.
. The hemorrhagic tendency.
. The skin on the hands, feet, abdomen and face may become darkened.
. Pancytopenia.
.A reversal of the albumin-globulin ratio.
★ Post–kala azar dermal leishmaniasis
.Follows the treatment of visceral leishmaniasis, normally develops < 2 years after recovery.
. Restricted to skin..
. Dermal lesions are categorized into 3 types, as follows:
. Depigmented macules
. Erythematous patches
. Yellowish pink nodules
Clinical
1. Visceral leishmaniasis ( Kala-azar )
① is caused by L. donovani.
② The incubation period: 3-6 months (months or years).
③ Main symptoms :
④ Complications:
Bacterial pneumonia, septicemia, dysentery, tuberculosis, cancrum oris, and uncontrolled hemorrhage or its sequelae can occur as complications of leishmaniasis.
⑤ Prognosis:
If untreated, death occurs within 2 years.
Clinical
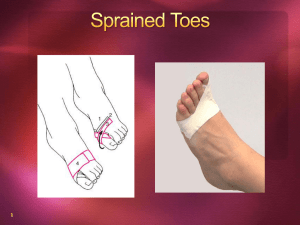
2. Cutaneous leishmaniasis
. caused by mainly in 2 forms, L. tropica and L. mexicana. L. tropica has two subspecies L. tropica and
L. major.
. the amastigote form resides in the large mononuclear cells of the skin.
. skin lesions mainly on the face, arms, and legs.
. often self-healing but can create serious disability and permanent scars.
Clinical
2. Cutaneous leishmaniasis
① caused by L. tropica
. The disease is also known as
“oriental sore”.
. An ulcer of 1-3cm develops with a surrounding zone of inflammation
(crater-like).
. Healing occurs in a few months and there is a lasting immunity.
After treatment
Typical lesions of cutaneous leishmaniasis caused by L. tropica
After treatment
Typical lesions of cutaneous leishmaniasis caused by L. tropica
Typical lesions of cutaneous leishmaniasis caused by L. major
Typical lesions of cutaneous leishmaniasis caused by L. major
Typical lesions of cutaneous leishmaniasis caused by L. major
After treatment
Typical lesions of cutaneous leishmaniasis caused by L. major
Clinical
2. Cutaneous leishmaniasis
② caused by L. mexicana
. The initial lesion in humans ulcerates and becomes crater-like and inflamed (like oriental sore).
. But it can cause “chiclero’s ulcer” which can involve almost total destruction of the external ear.
Clinical
2. Cutaneous leishmaniasis
▲ Diffuse cutaneous leishmaniasis
.associated with a deficient cell-mediated immunity .
.enables the parasite to disseminate in the subcutaneous tissues.
. non-healing, life long non-ulcerative infection
Clinical
3. Mucocutaneous leishmaniasis
. also called “espundia”.
. caused by L. braziliensis .
. it destroys the mucous membranes of the nose, mouth, throat and even soft palate.
Clinical
1. Visceral leishmaniasis ( Kala-azar )
2. Cutaneous leishmaniasis
3. Mucocutaneous leishmaniasis
Differential diagnosis:
Laboratory Studies
1. Direct evidence of infection:
① . Bone marrow aspiration:
Positivity rates ranging from
3. Supportive tests
② . Splenic aspiration:
Up to 98% positive results
③ . Lymph node aspiration or biopsy:
Positivity rates ranging from 54-86%
④ . Culture:
⑤ . Animal inoculation:
⑥ . cutaneous tissue biopsy or aspiration:
Laboratory Studies
1. Direct evidence of infection:
2. Indirect evidence of infection
①
. Detection of hypergammaglobinemia:
.the aldehyde test
.the antimony test
② . Immunological tests:
③
. Nonspecific tests:
. the direct agglutination test
. immunofluorescent antibody test
.complement fixation
.counterimmunoelectrophoresis
. Leishmanin skin test (Montenegro test)
. Polymerase chain reaction (PCR)
Laboratory Studies
1. Direct evidence of infection:
2. Indirect evidence of infection
3. Supportive tests
① . a normochromic normocytic anemia
② . leukopenia
③ . neutropenia
④ . thrombocytopenia
⑤ . elevated gamma globulins
⑥ . a reversal of the albumin-globulin ratio
Epidemiology
Geographical distribution
Epidemiology
Geographical distribution
.
Leishmaniases are considered to be endemic in 88 countries (16 developed countries, 72 developing countries) on 5 continents of Africa,
Asia, Europe, North America, and South America.
Epidemiology
The number of cases
.
Today, an estimated
12 million
cases of leishmaniasis exist worldwide. A total of 350 million people are at risk.
.
an estimated
1.5 -2 million new cases
occurring annually
.
Epidemiology
Today the number of cases of leishmaniasis is increasing, Why?
.
man-made environmental changes that increase human exposure to the sandfly vector.
.
the movement of susceptible populations into endemic areas, including large-scale migration of populations for economic reasons.
.
The immune deficiency has lead to increased susceptibility to infections, coexistence of leishmaniasis with HIV adds a serious dimension .
Prevention
.
Treatment of active cases.
.
Reservoir control.
.
Sandfly control.
.
Personal protection using repellants and nets is an important aspect.
.
Education regarding preventing the bite of sandfly.
Treatment
1. Visceral leishmaniasis ( Kala-azar ) sodium antimony gluconate----upto 25% resistance
Resistance to stibogluconate :
.should be treated with alternate agents, such as liposomal amphotericin, Pentamidine, aminosidine
. combination of stibogluconate with drugs, such as aminosidine and interferon gamma,
Treatment
2. Cutaneous leishmaniasis treatment essentially remains the same. sodium antimony gluconate and pentamidine are the drugs of choice.
3. Mucocutaneous leishmaniasis this responds to a 20-day course of sodium antimony gluconate, with resistant cases being treated with amphotericin.
Treatment
. Drug treatment
. Good nursing and diet
Summary1
Leishmania Species pathogenic in humans:
☆ leishmania donovani
(complex)
☆ leishmania tropica
☆ leishmania major
☆ leishmania mexicana
(complex)
☆ leishmania brazilliensis
(complex)
☆ leishmania aethiopica
Summary2 the female sandfly sucks blood buccal cavity the female sandfly bite
1.Infect stage: the promastigote form
2.The vector: sandfly
3.Methods of transmission : the bite of sandfly
4.Host: humans , dogs, wild rodents ,
5. Parasite spread: macrophage lysis→amastigote release.
via blood spead lymphatic spread
6. Reside site: the cells of the reticuloendothelial system
(skin, liver, spleen, lymph node, bone marrow)
Summary3
1. Visceral leishmaniasis ( Kala-azar ) caused by L. donovani.
2. Cutaneous leishmaniasis caused by mainly in 2 forms, L. tropica and L. mexicana.
3. Mucocutaneous leishmaniasis caused by L. braziliensis .