Week9
advertisement

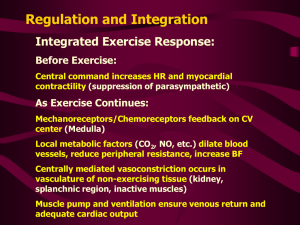
How do we measure heart performance? Cardiac Output = Blood Volume per Minute! Cardiac Output = heart rate x stroke volume Heart rate = # of beats per minute; can measure by taking pulse; normally ~ 75 b/min Stroke Volume = volume of blood ejected by L. Ventricle in one cardiac cycle Stroke volume = end DIASTOLIC volume – end SYSTOLIC volume Stroke Volume = 135 mL – 65 mL = 70 mL per beat Cardiac Output = 75 beat/min x 70 mL/beat = 5250 mL/min = 5.2 L/min Normal Cardiac Output Total Blood Volume = ~ 5 liters CO @ Rest: 5 L/min All blood in body is completely circulated every minute at rest! CO @ Exercise: 30-35 L/Min How does your body alter Cardiac Output to meet metabolic demands? How does your body Alter Cardiac Output? Cardiac Output = heart rate x stroke volume 1) Autonomic Nervous System 2) Endocrine (Hormonal) Control 3) Mechanically (Stroke Volume only) Somatic vs. Autonomic Somatic motor output is consciously controlled Autonomic motor output is NOT consciously controlled Functional subdivisions of ANS: Parasympathetic vs. Sympathetic Parasympathetic = Cranio-Sacral Division SLOWING, RELAXING effect Sympathetic = Thoraco-Lumbar Division SPEED-UP, EXCITE, FIGHT Autonomics are everywhere Autonomics are Reflex Arcs Autonomic Nervous System: General Anatomy 5 Parts: 1) 2) 3) 4) 5) Origin of neural signal Preganglionic neuron Autonomic ganglion Postganglionic neuron Target organ Main Differences: Postganglionic neuron Cholinergic vs Adrenergic Target tissue receptor Muscarinic vs α-adrenergic β-adrenergic Adrenal Medulla releases Epinephrine Epi = Adrenaline Epi Produces a Sympathetic-like Effect How does your body Alter Cardiac Output? Cardiac Output = heart rate x stroke volume Altering Cardiac Output: Heart Rate Heart rate is controlled by AUTONOMIC NERVOUS SYSTEM & Hormones! 2) Parasympathetic ANS decreases HR 3) Symapthetic ANS increases HR 4) Sympathetic stimulates Adrenal Gland Epinephrine (hormone) released to blood increases HR Remember: Heart electrical signals are initiated by Pacemaker cells (Autorhymicity) Their rate of depolarization is altered by ANS & Hormones Cardiac Output = heart rate x stroke volume Mechanisms of Altered Stroke Volume Stroke Volume (EDV – ESV) Stroke Volume is directly related to contraction force What effects the FORCE of Myocardial Contraction? Force of Ventricular Contraction Mechanisms of Altered Stroke Volume Stroke Volume is directly related to contraction force 1) Myocardium Muscle Fiber Length More STRETCH = longer fibers = greater contraction force = more blood expelled Frank-Starling Law of the Heart EDV determines STRETCH What determines EDV? Venous Return: amount of blood entering R. Atrium Increase Venous Return by: 1) Skeletal Muscle Pump Return MORE Blood from Muscle Veins 2) Constriction of Veins via Sympathetic ANS Forces Blood in Veins Back to RA Compression Tights What determines EDV? Venous Return: amount of blood entering R. Atrium Increase Venous Return by: 3) Respiratory Pump Lower Pressure is created in Inf. Vena Cava & Right Atrium during inspiration Bulk Flow pushes more blood towards RA Cardiac Output = heart rate x stroke volume 1) Venous Return > EDV > Fiber Length > Contractile Force Mechanisms of Altered Stroke Volume Stroke Volume is directly related to contraction force 1) Myocardium Muscle Fiber Length 2) Contractility Controlled by Autonomics (Neurotransmitters) & Endocrine (Hormones) Norepinephrine (Neuro) Epinephrine (Hormone) Acetylcholine (Neuro) Mechanism: Altered Calcium Concentrations in Myocardium Acetylcholine Summary: Altering Heart Performance Homeostasis and Heart Function Cardiac Output is altered in response to: Blood Pressure, pH, and/or CO2 1) O2, CO2 and pressure receptors carry sensory info to Brain Stem 2) Parasympathetic ANS decreases HR venous return contractility 3) Symapthetic ANS increases HR venous return contractility 4) Sympathetic stimulates Adrenal Gland Epinephrine (hormone) released to blood increases HR contractility Cardiovascular Physiology 1) Blood 2) Heart 3) Peripheral Circulation - tubes The primary function of the Cardiovascular system is to 1) deliver nutrients/oxygen and 2)remove wastes/CO2 from the cells in your body Basic Anatomy of Circulation Systemic Circuit Pulmonary Circuit Heart Artery SYSTOLE Heart Artery DIASTOLE MEAN ARTERIAL PRESSURE (MAP) :is responsible for bulk flow of blood :is measured on ARTERIES Cardiac Output = generates MAP Arteriole Resistance Controls Flow & Impacts MAP HIGH R = narrow arteriole = low flow LOW R = wide arteriole = high flow MAP = CO x R R = Arteriole Resistance to Flow More Cardiac Output = larger MAP Less Cardiac Output = smaller MAP More Resistance = smaller arteriole = greater MAP but slower flow Less Resistance = larger arteriole = lower MAP but greater flow Vascular Anatomy effects Resistance Arteries have more smooth muscle & elastic material than veins! Smooth Muscle Contraction varies with chemical input and varies widely! Neurotransmitters from ANS Hormones from Endocrine Glands Vasoactive Chemicals from Blood Vessels & Tissues Control of Vascular Resistance & Flow via smooth muscle 1) Chemical Control 2) Neural Control 3) Endocrine Control Local Control SHUNTS blood to different parts of body Note: Cardiac output = the total flow to all organs Shunting just redistributes the flow! Local Control of Blood Flow: Meta-Arterioles feeding into capillaries Metabolically ACTIVE tissue Results in: Resting tissue Results in: Low levels in O2, Glucose INCREASE in O2, Glucose High Levels in CO2, Lactic Acid, ADP DECREASE in CO2, Lactic Acid, ADP Leading to VASODILATION Leads to VASOCONSTRICTION 2) Neural control of Blood Flow: Widespread Blood Vessels ONLY have SYMPATHETIC INNERVATION! MAP = CO x R Alpha receptors are located on most of the vasculature Endocrine Control of Blood Flow: Epinephrine, Widespread Epinephrine enters circulation and binds β2-receptors β2-receptors are ONLY located Heart, Liver, Skeletal Muscles Epi on β2-receptors lead to VASODILATION Epi MAP = CO x R β2-receptors are not innervated by ANS!!!!! Not located elsewhere! Local Control = Precapillary sphincters - local, chemical control Widespread = vascular Smooth Muscle – sympathetic, adrenal MAP drives blood flow….. So the body carefully monitors and maintains MAP 1) Short Term maintenance of MAP – Cardiovascular Regulation 2) Long Term maintenance of MAP – Kidney & Hormonal Regulation MAP = CO x R Short & long term mechanisms will alter cardiac output & vascular resistance Short-Term Mechanisms for MAP homeostasis: ANS/ADRENAL via BARORECEPTOR REFLEX 1) Baroreceptors in Carotid Body & Aorta 2) Signal processed in Brainstem 3) IF High MAP Stimulates Parasym. Decrease in HR, Stroke Vol. MAP = CO x R 4&5) IF Low MAP Stimulates Sympathetics & Adrenal Gland Increase in HR, Stroke Volume Peripheral Vasoconstriction Vasodilatation at Heart, Skel. Musc. Liver MAP = CO x R Long-Term Mechanisms for MAP homeostasis 1) Renin-Angiotensin-Aldosterone 2) Vasopressin (Anti-diuretic Hormone) 3) Atrial-Natriuretic Hormone We will discuss these AFTER kidney physiology……because they all involve the kidney! Pathological MAP: Hypertension 180 Systolic > 130 Blood Pressure (mm Hg) 160 Diastolic > 100 Hypertensive, MAP > 130 mm Hg 140 120 Normal, MAP = 100 mm Hg Normal = 120/80 100 80 60 Time Increase Length Main Causes Hardening Increase in R Decrease Diameter (clogging, thrombi, Atheroscelrosis) LOSS of Elasticity Main Consequences: Heart Failure/Attack, Emboli (broken off blood clots) Poor Vision, Cerebral Hemorrhage Fluid Volume Blood: Functions 1) Transport of nutrients, gases, wastes 2) Transport of processed molecules (Vitamin precursors, recycled products) 3) Transport of hormones & enzymes 4) Buffer for pH and Fluid/Ion Balance 5) Body Temperature Homeostatis 6) Immune Response Blood: Composition We will talk RBC, Gases, Globulins with Respiratory physiology! Clotting: dealing with extensive damage Injury: Cut, Wound, etc. Activation of Clotting Cascade, Tissue Factors, Platelets + feedback loop Blood Clot Dissolves Atherosclerosis Damage to Endothelium = initiation of disease process Chemically: LDL, toxins Mechanically: Hypertension Normal Moderate Atherosclerosis Severe Atherosclerosis Inflammatory-Immune-Clotting Ruptured Atheroscelortic Plaque Initiates Clot (Thrombus) Formation Too much clotting results in Thrombus and/or Embolus! Thrombus breaks free = Embolus Emboli are a major cause of heart attack & stroke! Can originate from anywhere….e.g. varicose veins! Emboli can get lodged in any small artery Results in ISCHEMIA >>> Infarct >>>> Cell Necrosis Anti-Coagulants: Clot Inhibitors Aspirin: blocks thromboxane synthesis Platelet Factors = ADP & Thromboxane W/out Thromboxane fewer platelets are attracted to injury Fewer clots form; existing clots shrink Clot Intiation tPA- Tissue Plasminogen Activator Thrombolytic: Clot BUSTER Cardiovascular Physiology: Summary 1) Blood – carries nutrients 2) Heart – creates pressure gradient – blood flow 3) Peripheral Circulation – carries blood to tissues The primary function of the Cardiovascular system is to 1) deliver nutrients/oxygen and 2)remove wastes/CO2 from the cells in your body