Hepatic insufficiency
Wang Jing-jing
Department of
Pathophysiology
Shandong University
Introduction
Concept
Etiology and classification
The functional and metabolic changes
Hepatic encephalopathy
2
Introduction
1. Blood Supply:
Portal vein: 3/4 of the
blood flow (which drains
the stomach, intestine,
spleen, and pancreas)
Hepatic artery: 1/4 of
the blood flow
3
2. Internal Structure: Liver lobule
A central vein (coalesce into
hepatic veins, which empty
into the vena cava)
4-6 portal triad (branches of
hepatic artery, hepatic portal
vein and bile duct)
Rows of liver cells (Hepatocytes, hepatic stellate cells,
sinusoidal endothelial cells, Kupffer cells and liverassociated lymphocytes which are in close contact
with blood-filled sinusoids
Hepatic cirrhosis: pseudolobule
肝细胞变性坏死、纤维组织
增生及肝细胞结节状再生这
三种改变反复交替进行
3. Functions
Excretion: bile (help the absorption of vitamin K)
Clearing: the blood of particles and infections
including bacteria
Synthesis: albumin, lipoproteins, coagulation
factors, as well as protein C, S and antithrombin.
Metabolism: protein, lipid, carbohydrate
Neutralizing and destroying drugs and toxins
Manufacturing, breaking down and regulating:
numerous hormones including sex hormones
Concept
of Hepatic insufficiency
Severe damage in liver cells result in
degeneration, necrosis, fibrosis and cirrhosis,
manifesting as jaundice, bleeding, infection,
renal dysfunction or encephalopathy, termed
all together the syndrome of Hepatic
insufficiency
8
Etiology
1. Infections : hepatitis virus (HBV), bacteria, parasites
我国乙
肝感染
者9300
万 !丙肝
感染者
1000万!
9
HBV →入侵肝细胞→受染细胞表达 HbsAg 、 HbeAg 、
HBcAg → T 细胞识别、致敏→杀伤受染肝细胞:清除病毒
肝细胞损伤
10
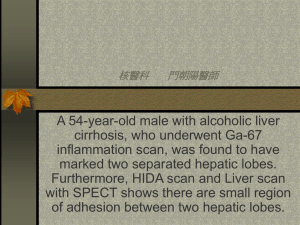
Cirrhosis
HBV multiplies, spreads and
eventually leads to scarring,
liver damage, cirrhosis and
cancer.
11
Some bacteria, such as Escherichia coli ( E. coli )
or staphylococcus (staph), tubercle bacillus
or amoeba caused Liver abscesses
13
市民吃生鱼虾致体内藏千条肝吸虫!
14
15
2. Medicines : Industrial toxins, drugs are modified or
degraded in the liver
Hepatic cytotoxicity: Degeneration and necrosis of
hepatic cells or synthesis of some proteins. 如:异烟
.肼,氟烷,醋氨酚,四环素、甲氨喋呤
Cholestasis: inhibit Na+-K+ ATP, fluidity of cell
membrane 如:氯丙嗪
16
17
3. Alcohol:
18
Normal liver
Alcoholic Fatty Liver
19
20
4. Nutritional causes
everything we eat must be refined and detoxified
by the liver
liver disease are always found among starving
populations.
good nutrition - a balanced diet can actually help
the damaged liver to regenerate new liver cells.
.
21
5. Inherited conditions
Wilson's disease:
a rare inherited
condition.
inability to excrete
copper into bile.
resulting in the toxic
accumulation of copper in
the liver and nervous
system.
22
6. Immunosuppression:
SLE, rheumatoid arthritis, Crohn's disease,
Systemic infections, such as tuberculosis, may
spread to the liver.
23
Classification
of hepatic insufficiency
Acute: short course of onset→ acute extensive necrosis
chronic: long course → late-staged chronic liver disease
Hepatic encephalopathy
Hepatorenal syndrome
Hepatic failure
24
1. Substance metabolism
(1) Carbohydrate Metabolism:
Glycogenolysis, Glycogenesis, Gluconeogenesis
Hypoglycemia, abnormal glucose tolerance
(2) Fat metabolism: synthesises lipoproteins,
cholesterol, phospholipids, lipogenesis and lipolysis
脂肪泻,厌油腻,脂肪肝,高胆固醇血症
(3) Protein metabolism: CRP, urea ,albumin ↓
腹水,出血倾向,防御功能下降
(4) Vitamine metabolism:
Absorption of liposoluble vitamine ↓
Storage of Vit A, Vit D, Vit E, Vit K ↓
Synthesis of vitamine ↓
夜盲,出血倾向,骨质疏松
(5) Energy metabolism:ATP ↓
27
Ecchymosis of skin
28
2. Disorders of bile and hormone
(1) Hyperbilirubinemia
Elimination of bilirubin ↓ →serum bilirubin↑ 黄疸
(2) Intrahepatic cholestasis
Production of bile salts ↓
→fat and fat –soluble vitamins ↓
→ Endotoxemia
(3) Elimination of hormone ↓ → estrogen ↑
aldosterone ↑, ADH ↑
29
Jaundice : yellow discoloration of the skin and whites of the eyes
30
the liver plays important roles in hormonal
modification and inactivation. Estrogen↑→ body feminization
Spider angioma
31
5. Disorders of blood coagulation
(1) Production of Blood coagulation factors ↓
(2) Anticoagulin↓
(3) Fibrinolytic system ↑
(4) Plt ↓
6. Function of detoxication ↓
7. Immunological function ↓
32
8.metabolic disorders of water and electrolytes
(1)Hepatic ascites: accumulation of fluid that fills and
distends the abdomen.
33
34
Cirrhosis, scar tissue, thrombosis in the portal vein
→Obstruction blocks the flow of blood through the
liver→Portal hypertension ↑ →capillary pressure↑
Obstruction of lymph →capillary pressure↑
Liver insufficient →synthesis of albumin↓→
osmotic pressure↓
Hepatic failure →aldosterone ↑ADH ↑
Renal failure → Water and salt rentention
35
(2) Hyponatremia :
Intake↓
Lose ↑: ADH, Diuresis, ascites
(3) Hypokalemia:
Intake↓
Lose ↑: aldosterone
(4) Alkalosis:
PaO2 ↓ anemia, Hyperammonemia
9. Disorders of organs: HE, hepatorenal syndrome
36
Hepatic encephalopathy
General Concept
Classification
Clinical Features
Pathogenesis
Precipitating Factors
Principles of Treatment
37
Ⅰ. General Concept, Classification
Clinical Features
A complex disturbance in central nervous system
that occurs as a consequence of severe liver
diseases.
hepatic coma; portal systemic encephalopathy
(PSE); HE
Hepatic coma refers only to a terminal stage of HE
38
Endogenous HE “spontaneous ”
No apparent
pricipitating factor, the final consequence of extensive
liver cell destruction.
Exogenous HE
Have apparent pricipitating factor,
(the development of portal-systemic shunts,
electrolyte ,acid-base imbalances, bleeding ,ingestion of
large amounts of dietary protein, etc)
39
Portal-systemic shunts
1. Portal hypertension →collateral circulation
40
1.
At the lower end of the esophagus
41
2. At rectal venous plexus
3. At periumbilical venous rete
4. Portal-retroperitoneal anastomosis
42
2. Transjugular Intrahepatic Portosystemic Shunt
43
门-奇静脉断流术
经颈静脉肝内门腔分流术
(TIPS)
44
远端脾-肾静脉分流术
45
Clinical features of HE generally
divided into 4 stages
slight altered mood
or behavior
including reversed
sleep pattern
Coma, no
response to
painful stimuli
Coma but
arousable
slurred speech
Drowsiness,
personality changes
intermittent
flapping tremor
46
Flapping
tremor
47
Precipitating factors in HE
1.Nitrogenous overload: a frequent cause of HE.
2. GI bleeding: The presence of blood in the
upper gastrointestinal tract results in increased
ammonia and nitrogen absorption from the gut.
Bleeding may predispose to kidney
hypoperfusion and impaired renal function.
48
3. Infection: Infection may predispose to impaired
renal function and to increased tissue catabolism,
both of which increase blood ammonia levels.
4. Constipation: Constipation increases intestinal
production and absorption of ammonia.
5. Renal failure: Renal failure leads to decreased
clearance of urea, ammonia, and other nitrogenous
compounds
49
6. Medications: Drugs that act upon the central
nervous system, such as opiates, benzodiazepines,
antidepressants, and antipsychotic agents, may
worsen HE.
7.Diuretic therapy: Decreased serum potassium
levels and alkalosis may facilitate the conversion of
NH4+ to NH3.
50
Ⅱ. Pathogenesis of HE
Ammonia intoxication hypothesis
False neurotransmission hypothesis
Amino acid imbalance hypothesis
GABA hypothesis
51
1. Ammonia intoxication hypothesis
(1) History
1877
Eck, Russian physiologist who created
portal-systemic shunts in healthy dogs
The beginning of the surgical treatment of portal
hypertension
the first vascular anastomosis
Ivan Pavlov “Eck-Pavlov fistula”
In 1893: Observed that these dogs promptly
became comatose after eating meat.
“meat intoxication”
in 1904: received Nobel Prize
(3)Supporting evidence
60~80% of HE show increased plasma ammonia level
Patients with hepatocirrhosis have elevated level of
ammonia
Symptom of HE and alteration in
electroencephalogram (EEG) after high protein diet
54
(4) Contents
NH3 production
NH3 production
NH3 clearance
( urea
cycle )
Under normal condition, the production
and the clearance of NH3 is in balance
55
NH3 clearance
NH3 production
Severe hepatic dysfunction
Hyperammonemia
HE
1) NH3 production
AA deaminization: amine oxidase
Intestine: unabsorbed aa or diffused urea that are
broken down by bacterial amino acid oxidases or
ureases.
pH↑ NH3 absorbed↑
Renal tubular epithelial cells: Hydrolysis of
glutamine
Skeletal muscles: Deamination of other amino
acids
2) NH3 clearance
Liver: “Urea cycle”
CO2 + 2HN3 + 3ATP + 3H2O = H2N-CO-NH2 +
2ADP + 4Pi +AMP
Brain and muscle: Formation of glutamine by
glutamine synthetase
ammonia+glutaminic acid = glutamine
3) Why does the NH3 increase in HE?
① NH3 production ↑
Portal hypertension: Capillary blood presure ↑ →
Congestion and edema of gastrointestinal tract →
AA digested and absorbed ↓
Bile ↓: Intestinal bacteria ↑ → ureases ↑ → NH3↑
Foods full of high protein or hemorrhage:
59
Severe
liver disease→renal failure→the urea
in blood defuses into intestine → NH3↑
Tic
of the muscles→ NH3↑
② NH3 clearance↓
Liver: Urea cycle ↓ → NH3 clearance↓:
ATP ↓ Function of enzyme ↓ Substrates ↓
and shunt
urea
NH3
protein
Normal
metabolism
NH3
61
Brain NH3↑
Liver
failure
Shunting
Circulation
Blood NH3↑↑
urea ×NH3
protein
NH3
62
The reasons of NH3↑
Production↑
clearance↓
GI tract
renal
muscles
urea syntheses
NH3
Portalsystmic
shunts
63
4)How does the NH3 lead to HE?
1.Decreasing energy production
In normal conditions: Because glycogen
reserves are less in the brain, brain needs much
of energy from oxidation of glucose.
Excess ammonia ultimately may cause cerebral
energy failure due to inhibition the energy
production.
64
Pyruvate
decarboxylase
Krebs cycle
65
2. Changing neurotransmitters
increasing glutamine and GABA
decreasing glutamic acid and acetylcholine
The
neurotransmitters include excitatory
transmitters (acetylcholine, glutamic acid, etc ) and
inhibitory transmitters (GABA, glutamine, etc) .
The
correct balance of neurotransmitters is critical
to the brain.
HE→NH3↑→GABA, glutamine↑, glutamic acid
and acetylcholine ↓→ disorder of CNS.
66
Krebs cycle
67
The reasons of NH3↑
Production↑
clearance↓
GI tract
renal
muscles
urea syntheses
NH3
Portalsystmic
shunts
68
Decreasing energy production
Krebs cycle
Changing neurotransmitters
Disturbing the ions transfer of the nervous cells membrane.
69
3. Ammonia disturbs the ions transfer of the
nervous cells membrane.
Na+-K+-ATPase which is located in the surface membrane
of cells is responsible for the active transport of Na+ and K+
between extracellular fluid and cytoplasm.
NH3 →ATP↓→ Na+-K+-ATPase ↓→ inhibits excitatory
postsynaptic potentials→depressing CNS function.
NH3
K+
Na+-K+-ATPase
Na+
70
However, not all data are consistent with the
ammonia toxicity theory.
Plasma levels of NH3 correlate poorly with HE
Acute NH3 intoxication may be characterized
by seizures which are unusual in either acute
or chronic HE.
NH3 does not induce the EEG changes of HE.
71
4. Astrocytic swelling:
(1) Glutamin
(2) Oxidative Stress:
(3) Permeability of mitochondrion
(4) AQP4↑
72
Ⅱ.False neurotransmission
hypothesis
73
False neurotransmission(FN) hypothesis
What is FN? And what is true
neurotransmission(TN)?
History of FN hypothesis?
Why FN is increased in hepatic insufficient
patients?
What is the mechanisms of FN in hepatic
insufficient patients?
74
1. What is FN? And what is TN ?
What is neurotransmitters?
Information is moved around the brain, from
nerve cell to nerve cell, by means of chemical
substances, called neurotransmitters
75
1.A message travels along the nerve
The roles of NT
and when it approaches the nerve
ending a neurotransmitter is released.
2.The neurotransmitter is received by
the next neuron
3. some of the neurotransmitter gets
reabsorbed
4.When enough neurotransmitter is
received by the next nerve cell the
message moves forward.
76
1. What is FN? And what is TN ?
Excitatory neurotransmitter:
Neuro-
transmitters
Ach, Aspartic acid
Inhibitory neurotransmitter:
GABA, Glutamine
77
The structure of FN and TN
TN
FNT
78
Excitation of
secondary
neuron
Excitation of
secondary
neuron
↑
True NT
synapse
Normal
FNT compete
receptor
Hepatic failure
Mode shown replacement of TN to
FN in HE
79
2. False neurotransmitter (FN) hypothesis
Supporting evidence
FN accumulates in liver failure.
In the corpus striatum of rats with encephalopathy,
concentrations of noradrenaline(NA) and
dopamine(DA) decreased, octopamine increased.
80
In 1970, Parkes first reported bendopa treat HE succesfully.
Fischer et al proposed FN hepothesis:
In the pateint with hepatic failure, FN
(phenylethanolamine and octopamine) is accumulated in
the synapse of the ascending reticular activating structure
(ARAS) in the brain stem.
The FN can compete with true Neurotransmitter (TN):
noradrenaline (NE) and dopamine (DA) because their
chemical structure is similar to the TN.
When FN replaces TN in RAS of brain stem, disorders of
CNS occur.
81
82
3. Why FN is increased in HE patients?
Congestion and edema of gastrointestinal
tract→disorders of the function (motion, secretion,
absorption, digestion) → inadequate digestion of
protein→Phe (phenylethylamine)
and Tyr (tyramine) ↑
Tyr and phe can’t be cleared by the process of
enzymatic degradation in liver.
Potal-systemic shunt make Tyr and phe flow in blood
directly.
83
Brain Tyr and phe↑
Liver
failure
↑ ↑
Blood Tyr and phe
Shunting
Circulation
× Tyr and phe
protein
Tyr and phe
84
4. How does the FN compete with TN?
85
Ⅲ. Plasma amino acid imbalance hypothesis
1.What is branched chain amino acids (BCAA) and
aromatic amino acids (AAA)?
2.What is the contents of Plasma amino acid imbalance
hypothesis?
3.Why plasma amino acids are imbalance in HE patients?
4. What is the mechanisms?
86
1.What is BCAA and AAA?
BCAA:
AAA:
87
Plasma
Phe
Tyr
Phe
Tyr
Try
BBB
Brain
HPEA
Hydroxylase
PEA
tyramine
Try
hydroxylase
decarboxylase
decarboxylase
hydroxylase
5-HTA
5-HT
88
2.What is the contents of Plasma amino acid
imbalance hypothesis?
In
HE patients, blood BCAA is decreased, AAA is
increased, so, AAA enters in to the brain more and form
FN.
Decreased
ratio of BCAA/AAA relates to HE due to FN
formation in CNS.
So,
this
hypothesis
is
an
extension
of
False
Neurotransmitter Hypothesis.
89
3.Why plasma amino acids are imbalance in HE patients?
BCAA↓:
Hepatic dysfunction→degradation of glucagon↓
Portal systemic shunts→ glucagon enter into blood
directly
→ glucagon ↑→ BCAA is excessive used by skeletal
muscle
90
AAA↑:
Brain Tyr and phe↑
Liver
failure
↑ ↑
Blood Tyr and phe
Shunting
Circulation
× Tyr and phe
protein
Tyr and phe
91
Phe
Plasma
Try
Tyr
BBB
Brain
NAA
Tyr
hydroxylase
Dopa
FNT, NAA,5-HT
Dopamine
FNT
Hydroxylase
PEA
tyramine
Try
hydroxylase
FNT, Phe, Try
decarboxylase
decarboxylase
Phe
5-HTA
NA
HPEA
5-HT
AAA/BCAA↑→AAA enter into brain↑→TN↓→FNT↑
92
4. The mechanisms of Plasma amino acid imbalance
The decrease in BCAA is caused predominantly by their
excessive use by skeletal muscle.
The increase in AAA is caused predominantly by failure of
hepatic failure or shunt.
BCAA/AAA↓in
CNS
may
interfere
with
normal
neurotransmission by competitively inhibiting TN (DA,
NA)
and
favoring
formation
of
FN
(octopamine,
phenylethanolamine)
93
Ⅳ GABA hypothesis
In the 1980s, Basile and Jones promoted:
gamma-aminobutyric acid (GABA), the major inhibitory
neurotransmitter in the CNS, as a cause of HE.
Of all brain nerve endings, 24-45% may be GABA ergic.
Increased GABA ergic tone is observed in patients with HE
94
Brain GABA↑
BBB↓
Blood GABA ↑↑
Shunting
Circulation
clear
×
GABA
Liver
failure
Foods full of
glumatic acid
Liver failure
bacteria in
intestine ↑
GABA
Edema, congestion → digestion↓,absorb↑
95
GABA crosses the blood-brain barrier→released by Vesicle
of excited presynaptic neuron cell → GABA receptors( in
conjunction with receptors for benzodiazepines and
barbiturates) → Cl- channel opens → Cl- influxs into the
postsynaptic neuron → membrane hyperpolarization →
inhibitory postsynaptic potential.
Cl-
BZ
BR GABAR↑
Cl-
GABA
↑
cell
Post-synapse inhibition
Liver failure
96
Treatment
1. Identification and Removal of Precipitating Factors
(1)Dietary protein should be eliminated
(2)Oral lactulose should be given
Lactulose is degraded by colonic bacteria and converted to
lactic acid and other acids, with resulting acidification of
The gut lumen. This favors conversion of NH4+ to NH3 and
The passage of NH3 from tissues into the lumen.
97
(3) Gastrointestinal bleeding must be stopped. The
intestines must be emptied of blood. Blood breaks
down into protein components that are converted to
ammonia.
(4)Treatment of infections, renal failure, and electrolyte
abnormalities (especially potassium) is important.
98
2. reducing plasma ammonia and other toxins
levodopa,
a precursor of normal
neurotransmitters
bromocriptine, a dopamine agonist
infusions
of branched chain amino acids
flumazenil, a benzodiazepine antagonist
3. Liver transplantation
99
Risk Factors
1. Risk Factos in People with Alcoholism
Only 10% of heavy drinkers develop advanced liver
disease. Not eating when drinking and consuming a variety
of alcoholic beverages are factors that increase the risk for
liver damage.
Obesity is a major factor for all stages of liver disease.
Women develop liver disease at lower quantities of alcohol
intake than men. The reason for this may be due to
women's inability to metabolize alcohol as quickly as men,
so it stays in the bloodstream longer.
Genetic factors that regulate the immune responses in the
intestine also play role in increasing the risk for liver injury
from alcoholism.
100
2. Risk Factors in People with Chronic Hepatitis
• Hepatitis C at higher risk for liver damage, especially Coinfection with hepatitis B or HIV.
• Being diabetic and overweight, particularly if fat is
distributed in the abdomen (an apple-shape). This condition
poses a higher risk for nonalcoholic fatty liver disease (NASH),
which in turn is apt to become scarred and cirrhotic.
• High exposure to toxic chemicals or environmental
contaminants.
101
Weight gain in the area of and above the waist (apple
type) is more dangerous than weight gained around
the hips and flank area (pear type). Fat cells in the
upper body have different qualities than those found
in hips and thighs.
102
3. Risk Factors for Cirrhosis in Autoimmune Liver
Diseases
4. Obesity and Other Risk Factors for Cirrhosis
obesity increased the risk of death from cirrhosis in those who
drank little or no alcohol, but not in alcoholics. Men are at
higher risk than women and African Americans have a higher
risk than Caucasians.
103
病案分析
男性,45岁。10年前患乙型肝炎,经治疗后痊愈。
近3年来常于劳累后乏力,进食后饱胀,纳差。半年
来上述症状逐渐加重,腹胀、大便不成形,每日2次
,无粘液和脓血。经常出现鼻和齿龈出血。近3天腹
泻后出现精神状态差,反应迟钝、少言、随地便溺
。2小时前始处于熟睡状态,呼之可醒,但不能正确
回答问题。
辅助检查:HBsAg和HBeAg阳性。
体格检查:体温37.5℃ 脉搏78次/分 呼吸16次/分
血压15.0/8.0 kPa,嗜睡状态,压眶反射存在。面
色灰暗黝黑,巩膜黄染。颈软,颈部、前胸有多个蜘
蛛痣,可见肝掌。心肺检查正常。腹部呈蛙腹,肝脏
右肋下未及,脾左助下4Cm,移动性浊音阳性,肠
鸣音正常。
1:根据患者的病史特点,诊断什么疾病?
2:为进一步证实诊断,还需做哪些辅助检查?
3:该患者使用利尿剂时的原则和注意事项有哪些?
106