incomplete crossmatch
advertisement
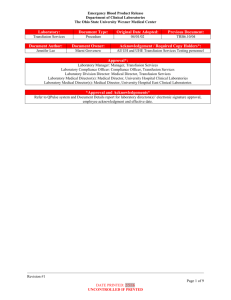
By Ahmad Nabil Hamdy Intended Learning Outcomes (ILOs) Compatibility Testing Approaches Requiring Less Than a Complete Crossmatch Is the Crossmatch Really Needed? What can be given in an emergency transfusion? Compatibility testing is done to avoid a hemolytic transfusion reaction If the Host or Recipient recognizes the donor RBC surface antigens as foreign, the host will mount an immune response to the donor RBC’s ABO ABO blood group antigens present on red blood cells and IgM antibodies present in the serum Rhesus 47 Antigens make up the Rhesus Blood Group The most significant is the D antigen What is compatibility testing? Also called pretransfusion testing Purpose: To select blood components that will not cause harm to the recipient and will have acceptable survival when transfused If properly performed, compatibility tests will confirm ABO compatibility between the component and the recipient and will detect the most clinically significant unexpected antibodies Compatibility testing Can be divided into 3 categories: Preanalytical procedures Serological testing Postanalytical procedures Patient Identification Must confirm recipient’s ID from bracelet ON the patient Full patient name and hospital number Name of physician http://www.usatoday.com/tech/news/techinnovations/2006-07-17-chips-everywhere_x.htm Sample Identification The sample should also have the full patient name, hospital number, and physician Date and time of collection, phlebotomist’s initials All of this should be on the request form and the sample Specimen Tubes Pink Top - EDTA Red Top – no additives Serological Testing 3 tests: ABO/Rh Antibody detection/identification Crossmatch ABO/Rh Typing In the ABO typing, the forward and reverse MUST match In the Rh typing, the control must be negative Both of these will indicate what type of blood should be given Anti A Anti B A Anti B Anti A Anti B B Anti A AB Anti A Anti B O Antibody screen Also called the indirect Coombs test or the indirect antiglobulin test The antibody screen will detect the presence of any unexpected antibodies in patient serum If antibodies are detected, identification should be performed using panel cells (with an autocontrol) IS 37° (LISS) AHG Crossmatching Purpose: Prevent transfusion reactions Increase in vivo survival of red cells Double checks for ABO errors Another method of detecting antibodies Crossmatches According to the AABB Standards: The crossmatch “shall use methods that demonstrate ABO incompatibility and clinically significant antibodies to red cell antigens and shall include an antiglobulin phase” Crossmatch No agglutination ~ compatible Agglutination ~ incompatible Donor RBCs (washed) Patient serum The procedure Donor cells are taken from segments that are attached to the unit itself Segments are a sampling of the blood and eliminate having to open the actual unit Crossmatch Procedure if antibodies are NOT detected: Only immediate spin (IS) is performed using patient serum and donor blood suspension This fulfills the AABB standard for ABO incompatibility This is an INCOMPLETE CROSSMATCH If antibodies ARE detected: Antigen negative units found and X-matched All phases are tested: IS, 37°, AHG This is a COMPLETE CROSSMATCH Crossmatches… Will Verify donor cell ABO compatibility Detect most antibodies against donor cells Will Not Guarantee normal survival of RBCs Prevent patient from developing an antibody Detect all antibodies Prevent delayed transfusion reactions Approaches Requiring Less Than a Complete Crossmatch Type and Screen Determines the ABO-Rh of the patient and the presence of the most commonly found unexpected antibodies(elimination of the crossmatch ). Type and Screen If an emergency transfusion is required after type and screen alone, an immediate-phase crossmatch is performed. Blood given in this manner is more than 99% effective in preventing incompatible transfusion reactions due to unexpected antibodies. Is the Crossmatch Really Needed? If the correct ABO and Rh blood type is given, the possibility of transfusing incompatible blood is less than 1 chance in 1000. ABO-Rh typing alone results in a 99.8% chance of a compatible transfusion, The addition of an antibody screen increases the safety to 99.94%, and A crossmatch increases this to 99.95%. Physician responsibility in ordering uncrossmatched blood In an emergency (ER or OR), there may not be enough time to test the recipient’s sample It is your judgment that the risk of the patient dying from from anemia is greater than the risk of transfusing the patient without pre-transfusion testing What can be given in an emergency? Type-Specific, Partially Crossmatched Blood An ABO-Rh typing and an immediate-phase crossmatch An abbreviated format Macroscopic agglutination. This takes 1 to 5 minutes What can be given in an emergency? Type-Specific, Uncrossmatched Blood The ABO-Rh type Most ABO type-specific transfusions are successful. Caution should be used for patients who have previously received transfusions or have had pregnancies. What can be given in an emergency? Type O Rh-Negative (Universal Donor), Uncrossmatched Blood Type O blood lacks the A and B antigens Type O Rh-negative, uncrossmatched packed RBCs should be used in preference to type O Rh-negative whole blood. More than two units of type O Rh-negative, uncrossmatched whole blood, the patient probably cannot be switched to his or her blood type . Specific Recommended Protocol Infuse crystalloids or colloids. 2. Draw a blood sample for typing and crossmatching. 3. If crossmatched blood is not ready to give, use typespecific or type O Rh-negative cells or type O Rhpositive cells for males or postmenopausal females without a history of transfusions. 1. Summary The crossmatch “shall use methods that demonstrate ABO incompatibility and clinically significant antibodies to red cell antigens If an emergency transfusion is required after type and screen alone, an immediate-phase crossmatch is performed before transfusion (an abbreviated format ) If crossmatched blood is not ready to give, use type-specific or type O Rh-negative cells