NC Public Health Nurse
Mentoring Orientation materials
Background
Retention problems exist in all of nursing but are
particularly problematic in public health
Nurses entering governmental public health nursing
positions appear to have knowledge deficiencies in areas
such as:
• Population focus
• Epidemiology
• Health education
• Advocacy
• Case management
Background
• Challenges exist attracting, recruiting and retaining
public health nurses
• Public health nursing workforce is aging
• The cost of turnover in one position is @ 75% of
the annual salary of that position.
COPE (Committee on Practice and
Education) of NC Association of PHN
Administrators has been looking at
recruitment and retention issues
affecting the specialty field of Public
Health Nursing. Mentoring has been
identified as an effective tool in
assuring the successful transition of
nurses to public health.
What is Mentoring?
Mentoring is a deliberate pairing of a more skilled or
more experienced person with a less skilled or
less experienced one, with the mutually agreed
goal of having the less skilled person grow and
develop specific competencies.
(Murray, 2001)
What is Mentoring?
Mentoring is a personalized one-on-one approach to
learning grounded in a personal and professional
relationship between a mentee (the learner) and
the mentor (the teacher).
(Goldman & Schmalz, 2001)
Definition of Mentoring
• A teacher and educator
• “be available to help
learn a new topic or
area”
• Support
• “support person…in a
nutshell”
• A guide and leader
• “coaching-building on big
picture”
• Experienced
• “someone to show you
the ropes”
• Role model
• A resource
“go to person”
• “ someone you trust and
respect”
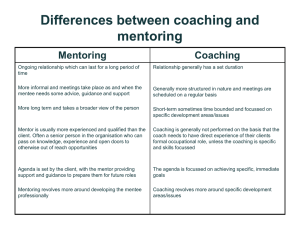
They Are Different!
• Mentoring
• Precepting
Preceptor vs. Mentor
Preceptor
Mentor
View of Intern
Views intern as a prospective
co-worker
Views intern as a colleague
Conceptual focus
Focuses on practice based
learning
Focuses on personal development
Prior knowledge
Assumes intern has necessary content knowledge
Theory/Practice
Demonstrates the
incorporation of theory in
practice
Identifies unwritten work-place
policies and practices
Learning experiences
Suggests useful learning
experiences to help intern
achieve learning objectives
Encourages intern to determine
learning experiences to achieve
objectives
Ethical concerns
Identifies actual ethical concerns
Strengths/ weaknesses
Helps intern become aware of strengths and weaknesses
Progress evaluation
Provides intern with an evaluation of professional progress
Intern self-evaluation
Identifies usefulness of selfevaluations
Strongly encourages intern to
participate in self-evaluation
Role model
Views oneself as a
professional role model
Views oneself as a personal role
model
Duration of relationship
Recognizes relationship with
intern is limited
Views the relationship with the
intern as indefinite
Benefits of Mentoring
To Mentor
• Shares their successes and achievements with the mentee
• Practices interpersonal and management skills
• Expands horizons
• Gains insight from mentee’s background
• Reenergizes own career
• Enlists an ally in promoting the organization’s well-being
• Increases network of colleagues
• Recognizes and increases skills in leadership & coaching
• May reduce turnover and additional work
Benefits of Mentoring
To Mentee
• Gains an active listening ear
• Receives valuable direction
• Learns a different perspective
• Gains from mentor’s expertise
• Receives critical feedback in key areas
• Develops sharper focus
• Learns specific skills and knowledge
• Gains knowledge about the organization’s culture &
unspoken rules
• May reduce turnover and additional work
Responsibilities
Mentor
• Introduces population-based nursing concepts
• Ensures two-way open communication
• Assists in establishing parameters of partnership
• Provides as much career path information as possible
• Shares information about career opportunities and
resources
• Shares information about own job and resources
• Provides encouragement
Responsibilities
Mentor - cont’d
• Monitors and provides sensitive feedback and
guidance
• Follows through on commitments
• Acts as a role model
• Respects confidentiality of information shared by
mentee
Responsibilities
Mentee
• Is willing to learn and grow
• Accepts advice and provides mentor with feedback
• Takes on new challenges
• Remains available and open
• Is proactive in relationship
• Identifies goals
• Accepts responsibility for own development
• Demonstrates commitment to the relationship
Key Considerations
Mentors
• Is willing to spend a minimum of two hours/month with mentee
• Is committed to attending mentor training and yearly updates of
training
• Exhibits characteristics such as:
Coaching
Motivating
Leadership
Listening
Sharing
Advising
Encouraging
Proficiency in practice Willing to share knowledge & expertise
• Is committed to the mentoring process
• Has the ability to create a learning environment
Key Considerations Mentees
• Is a new employee, where new is defined as a nurse who is
new to working in a public health agency or a nurse who is in
a new role in a public health agency
• Has a working knowledge of career goals and objectives
• Is willing to set aside time to meet with mentor
• Is committed to participating
• Is open to suggestions and feedback from the mentor
A Few Concepts About
Public Health Nursing
What is Public Health Nursing?
Public Health Nursing is the practice of
promoting and protecting the health of
populations using knowledge from nursing,
social and public health sciences.
(APHA, Public Health Nursing Section, 1996.)
Cornerstones of Public Health Nursing
Public Health
• Population based
• Grounded in social justice
• Focus on greater good
• Focus on health promotion and
prevention
• Does what others cannot or will not
• Driven by the science of epidemiology
• Organizes community resources
• Long-term commitment to the
community
Nursing
• Relationship based
• Grounded in an ethic of
caring
• Sensitivity to diversity
• Holistic focus
• Respect for the worth of all
• Independent action
Cornerstones of PH Nursing, Minnesota Department of Health , revised 2007
Population-based care vs.
Individual Medical care:
Population-based Care
•
Goal is an overall healthy population
•
Might involve health-improvement goals for a
community or sub-set of a community that are
many years (even a generation) away
•
Primary intervention strategies are provision of
information, education, and communication.
•
•
•
Individual Medical Care
•
•
Goal is a healthy person
Primarily focuses on current patient
conditions, and prevention of onset of new
conditions in a particular person
•
Collaborates with other community groups to
advocate for policies that will allow and
encourage healthy behaviors
Primary strategies are biological (medication,
surgery, for example), with information and
education as a supplement
•
Uses community health data to plan strategies,
based on the specific demographics, strengths,
and weaknesses of a particular community
Advocates for services for specific patients,
and for exceptions or adaptations to policies
to accommodate those patients
•
Uses medical research to determine the most
appropriate care for a particular patient
•
Recognizes the impact of environment on
specific patients with specific conditions. This
might include presence of respiratory triggers
for patients with lung diseases, or availability
of appropriate food for diabetics.
Has a broad awareness of the environment’s
impact on health. This includes such things as
safe food and water, sidewalks in good repair,
availability of transportation, housing quality,
etc.
Population Focus
• Individuals present in clinic with communicable
disease—treat individual
• Identify population needs for disease
– Preventing transmission
– Communicating to your population
– Providing treatment
• Example: Ringworm
Vulnerable Populations
Health Disparities
Health Literacy
Definition of Vulnerable Populations
• Greater risk for poor health status and/or
problems with access to health care
• Higher probability of illness and worse
health outcomes than others.
• Multiple risk factors interact to limit
resiliency.
Vulnerability is Multidimensional
Resource limitations
• Economic (poverty and link to hazardous
environments and in adequate nutrition)
• Educational (ability to understand health
information and make informed choices)
• Social (support system)
• Health status (physical, biological, psychological)
• Health risk (lifestyle, environmental)
Health Disparities
Differences in quality of care and health outcomes by
age, gender, race, ethnicity, education, income,
disability, sexual orientation or geography due to:
• Patient level factors (e.g., biology, behaviors)
• Provider-level factors (e.g., stereotyping)
• System factors (e.g., lack of insurance)
• Social and political factors
Vulnerable population groups are most likely to
experience health disparities in access to
care, quality of care and health outcomes.
Connecting the Terms
Health Literacy
"The degree to which individuals have the
capacity to obtain, process, and understand
basic health information and services needed
to make appropriate health decisions".
• From Healthy People 2010
Institute of Medicine
A Prescription to End Confusion
“Ninety million people in the United States,
nearly half the population, have
difficulty understanding and using
health information”
How can nurses make a difference?
•
•
•
•
•
•
Identification (outreach and case finding)
Linking to health services (case manager)
Developing or revising programs to meet their needs
Educating them on how to promote health
Providing direct care
Advocating for programs and services to meet their needs
CULTURAL DIVERSITY:
Gabriela Zabala
Office of Minority Health and Health Disparities
NC Department of Health and Human Services
Forest Toms, PhD
Training Research & Development, Inc. , Hickory, NC
Goal
To build the foundation for culturally
appropriate health services
capable of serving an increasingly
diverse population.
“When we think…
of Culture, we think of mainstream
America; but when we think
of Diversity the tendency is to think of
minority groups.”
“American Culture”
• White middle-class values
• Dominant culture
• Mainstream culture
• European – American (Anglo)
ASSUMPTIONS & APPROACHES TO
DIVERSITY
•
•
•
•
•
•
DIVISIVE/PANDORA’S BOX
ONLY BLACK/WHITE
NOT AN ISSUE
SHOULD TREAT EVERYONE THE SAME
RESOURCES
ALREADY DEALT WITH
“Why” of Diversity
What’s In a Name?
• African American – Black, Africans, Carribeans
• Hispanic/Latino – Mexican, Puerto Rican, Cuban,
Salvadorian, Ecuadorian, Argentinan, Honduran,
Dominican, etc
• European/Anglo – White
• American Indian – Native American,
Alaska Native, Aleutian
• Asian – Chinese, Filipino, Korean,
Japanese, Vietnamese, Cambodian,
Laotian, Hmong, Pacific Islander
(Polynesian, Melanesian, Micronesian)
US Population Composition 1990 - 2050
American Indian
0.9
8.2
Asian/Pacific Island
Hispanic
24.5
Black
2050
13.6
52.8
White
American Indian
0.8
6.7
Asian/Pacific Island
Hispanic
18.9
Black
2030
13.1
White
60.5
American Indian
0.7
Asian/Pacific Island
Hispanic
2.8
9.1
Black
1990
11.8
White
75.6
0
Source: U.S. Census Bureau
10
20
30
40
50
Percentage of US Population
60
70
80
“What” of
Diversity
Dimensions of Diversity
• Primary
– Largely unchangeable human differences
– Inborn
– Influence our early socialization
• Secondary
– Can be changed
– Differences we acquire, discard and modify
throughout our lives
Primary Dimensions of Diversity
Age
Ethnicity
Gender
Unchangeable
Differences
Race
Physical
Abilities/Qualities
Sexual/Affectional
Orientation
TRD,Inc. All Rights Reserved
Secondary Dimensions of Diversity
Educational
Background
Work Experience
Geographic
Location
Household
Composition
Marital Status
Military
Experience
Income
Religious
Beliefs
TRD,Inc. All Rights Reserved
Culture
• Behavior patterns, arts, beliefs, institutions, and
all other products of human work and thought
American Heritage Dictionary, 1991
• A view of the world and a means of adapting to
the world
Bilingual Health Initiative Task Force, 1994
• Is reflected in, and influences beliefs and values,
communication styles, health beliefs and
practices
Culture Helps Us…
Organizes Our Physical
And Social Interaction
Forms Our
Identity
Shapes Our Understanding
And Perceptions
Culture Defines
Family Roles
Family Structure
Attitudes
And
Practices
Family Relationships
Styles Of
Communication
Beliefs
Beliefs and Values
•
•
•
•
•
•
What we are used to thinking and doing
What we feel or know is right, good, important
Complex concepts with many dimensions
Influence all other area of life and activity
Affect how people think, feel, act
Can cause conflict if people’s
beliefs and values are not
incorporated in health
recommendations
Overview of Beliefs
Comparison of Common Values
Anglo-Americans
– Mastery over nature
– Personal control over the
environment
– Doing-activity
– Time dominates
– Human equality
– Individualism/privacy
– Youth
– Self-help
– Competition
– Future orientation
– Informality
– Directness/openness/honesty
– Practicality/efficiency
– Materialism
Other Ethnocultural Groups
–
–
–
–
–
–
–
–
–
–
–
–
–
–
Harmony with nature
Fate
Being
Personal interaction dominates
Hierarchy/rank/status
Group welfare
Elders
Birthright inheritance
Cooperation
Past or present orientation
Formality
Indirectness/ritual/”face”
Idealism
Spiritualism
Culture and Healthcare
Patients
Health Status – Minority Groups
High risk for :
– Heart disease, diabetes, cancer,
homicides, infant mortality –
African Americans
– Stroke/diabetes, MVA, infant
mortality American Indian
– Diabetes, MVA, homicide Hispanics
– Diabetes - Asians/Pacific
Islanders
• Teen pregnancy
– African Americans
– American Indians
– Hispanics
Barriers to Health Services
•
•
•
•
•
•
•
•
•
High rates of poverty
Unemployment
Cost of care
Lack of insurance
Location and hours of
services
Lack of transportation
Lack of information
Language
Cultural differences
between providers and
clients
Visions of a Culturally Competent
Healthcare System
Definition of Cultural Competence
• The process is ongoing and continuous.
• Cultural competence is a dynamic, developmental
process and a state towards which we should strive, it
takes a long-term and consistent commitment to
achieve.
• It is not something that comes to the individual, the
agency, or the system through a one-shot, quick-fix
approach.
Cultural Competency Continuum
Cultural destructiveness -- attitudes, policies, and
practices that are harmful to cultures and hence to
individuals within the culture.
Cultural incapacity -- the system or agencies lack(s) the
capacity to help minority clients or communities.
There is much bias.
Cultural blindness -- the system and agencies
provide(s) services with the belief that they are
unbiased. The premise is that services are universally
applicable.
MOVING TOWARDS THE GOAL
• There must be a willingness and courage to confront
all the feelings and attitudes that cultural
competence and change indicate for the individual,
the agency, and society in general.
• As Pinderhughes (1989) states, the multicultural staff
engages in dialogue about their differences in
perceptions and experiences.
OUTCOMES
• Failure to provide the opportunity to understand and
process these differences among a multicultural staff can
produce two outcomes:
• staff will cover over the conflict in perceptions and
orientation and block off the confusion, frustration,
and strong feelings.
• conflict can erupt and staff will become burned out
and fatigued.
BEFORE TAKING ACTION
• Agencies should understand cultural dynamics
and the significance of cultural identify for
themselves, their clients, and their work together.
• Opportunities for sharing and dialogue must be
built into the structure of the agency or
organization seeking to become
more culturally competent.
UNDERSTANDING THE AGENCY ENVIRONMENT
As part of the agency’s commitment, it should be
recognized that cultural diversity and cultural
competence require an understanding of the
sociopolitical environment in which an agency
operates.
Nurse Mentoring Relationship
Getting Started
Keeping Momentum Going
Mentoring Agreement
Once matched, the pair should write up a formal
mentoring agreement to clarify their roles with
one another. This agreement can determine the
framework of the relationship.
Getting Started
•
•
•
•
•
•
•
•
Schedule first meeting within one week of matching
Review goals and objectives
Discuss goals and objectives and activities
Complete mentoring agreement
Exchange contact information and schedules as necessary
Maintain twice monthly contacts
Check in with contact person to share progress
“Close” the relationship after designated time
Keeping Momentum Going
• Beyond goals in contract
• Discuss networking opportunities, NC Public
Health Nursing
• Teach mentee about day-to-day LHD
operations
• Schedule visits or shadowing opportunities to
other LHD clinics and services
• Focus on work-life balance issues
Work Issues
• Plan
• Keep mentoring a priority
• Acknowledge / deal with conflicts
Overcoming Barriers
Barriers
– Time
– Other priorities
– Role tensions
– OTHERS?
Solutions
– Set a calendar
– Nurse supervisor
support
– Facilitate approaching
supervisor
– OTHERS?
Crisis Management
• Changing from individual to population focus
• Addressing health department priorities
• Problem solving
Health Department Priorities
• Require staff adjustments
– Job priorities
– Work schedules
– Implementing protocols
• Priority changers
– Communicable disease outbreak
– Weather events (hurricanes, floods)
– Influx of immigrants
Health Department Problem Solving: Exercise
• Ethical dilemmas
– Client treatment
– Work performance
• Potential dilemmas
• What are your health dept policies and
protocols on these issues?
• How should you be involved to work with
mentee?
Additional Resources
• Nurse Mentoring Manual
• Website—NC Public Health Nursing
http://www.ncpublichealthnursing.org