quality assurance – paho/who – ops/oms
advertisement
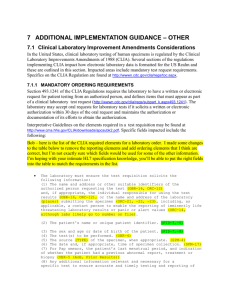
QUALITY ASSURANCE Shree Baboolal 12th February, 2005 Quality Assurance in Healthcare All management systems are now focused on getting the job done. All promise more efficient and effective management Some have been effective in making larger profits while others have been effective in providing a better service to the client Total Quality Management (TQM First introduced by Dr. W. Deming - 1988 Used statistics to analyze production processes and discover the source of product flaws Workers actively participate in decisions to improve production – team effort Total involvement from all levels Quality improvement reduces waste and leads to improved productivity Quality Improvement (QI) Now part of accreditation requirements for all types of healthcare facilities and found in every aspect of healthcare including phlebotomy procedures. One way to improve quality is through the use of national standards and regulations. National Standard and Regulatory Agencies Joint Commission on Accreditation of Healthcare Organizations (JCAHO) College of American Pathologists (CAP) Clinical Laboratory Improvement Amendments of 1988 (CLIA ’88) National Committee for Clinical Laboratory Standards (NCCLS) National Accrediting Agency for Clinical Laboratory Sciences (NAACLS) National Standard and Regulatory Agencies Joint Commission on Accreditation of Healthcare Organizations (JCAHO) – – – – Voluntary, non-governmental agency Establish standards for the operation of healthcare facilities 1994, JCAHO required all healthcare facility to have a TQM/CQI plan in place Ongoing evaluation of customer satisfaction Current standards from JCAHO Healthcare facility must be directly accountable to their customer Must evaluate and track complaints about quality of care Created an office to monitor complaints – Office of Quality Monitoring Quality Incident form JCAHO reviews reports and depending on the nature of the report will do the following: JCAHO will Request from the organization a written response to the reported concern Conduct an onsite assessment of the report Incorporate the concern on their database to see trends or patterns in performance Review the reported concern at the next accreditation survey College of American Pathologists Outgrowth of the American Society of Clinical Pathologists Membership – board certified pathologists Offers proficiency testing Laboratory inspection – team made up of pathologists and lab managers Clinical Laboratory Improvement Amendments of 1988 These are federal regulations passed by congress Establish standards that apply to all health facilities including laboratories Aim is to ensure accuracy, reliability and timeliness of patient test results Standard address quality assurance, quality control, proficiency testing, laboratory records and personnel qualifications CLIA continued Certificate is obtained based on the complexity of testing Three categories of testing are recognised – – – Waived complexity Moderate complexity High complexity Complexity of testing is based on the difficulty in performing the test and the degree of harm to a patient if the test is performed inaccurately CLIA continued CLIA requirements are more stringent for moderate and high complexity testing These facilities are subject to routine inspections Specimen collection is an important part of CLIA inspection Required to have written protocols for all procedures National Committee for Clinical laboratory Standards International, non-profit educational organization Has representation from the profession, industry and government Use a consensus process to develop voluntary guidelines and standards for laboratories Phlebotomy and certification examination questions are based on these guidelines and standards National Accrediting Agency for Clinical Laboratory Sciences Recognised by the United States Department of education as an authority on educational quality Non-profit organization Provides either accreditation or approval for clinical laboratory educational programs Approves process for phlebotomy programs to ensure competencies are met Quality Assurance in Phlebotomy Laboratory testing is an important part of patient diagnosis A major part of patient care Doctors rely on validity of test results Pre-analytical factors such as patient preparation, specimen collection procedures and specimen handling can affect the validity of test results Quality Assurance in Phlebotomy All the procedures should be based on specific guidelines Phlebotomists should adhere strictly to these guidelines Established policies and procedures fall under an overall process called Quality Assurance (QA) QA defined QA is defined as a program that guarantees quality patient care by tracking outcomes through scheduled reviews Guidelines are developed for all the processes and when formally adopted becomes the QA program QA Indicators Tool to monitor and evaluate all processes Must be measurable, well defined, specific, objective and clearly related to an important aspect of care Indicators can measure quality, adequacy, accuracy, timeliness, effectiveness, customer satisfaction etc. Thresholds and Data Threshold values must be established for all clinical indicators Threshold value – level of acceptable practice If levels of care is unacceptable – corrective plan is established Monitor and evaluate continuously to ensure quality improvement Process and Outcomes To change outcome we must look at process Follow process from start to finish to see where there might be obstacles – or where the problem lie To ensure that the same process is always followed, there must be controls and checks along the way The use of controls in a process is known as Quality Control QC defined Component of a QA program Procedure control QC process in phlebotomy involves checking all the operational procedures to make certain they are performed correctly QA is overseen by the supervisor in the Phlebotomy department The phlebotomist must ensure that they meet standards at all times Areas of Phlebotomy subject to QC Patient preparation procedures Specimen collection procedures – – Identification Equipment puncture device evacuated tubes Labeling Technique Collection priorities Delta checks Documentation Major component of QA program QA documents have been developed to: standardize procedure, inform nursing personnel on importance of patient preparation and record problems Can be used for legal purposes as well Can provide information for QA purposes Patient medical records User manual Example of QA documentation Chart or type form Contains information on minimum amount of specimens required, special handling desired, reference values, TAT etc. Procedure Manual Standardization purposes Must be updated annually Written in a special format – NCCLS States laboratory policy and procedures that apply to each test in the lab Information found in a Procedure Manual Purpose of the procedure Specimen type and collection method Equipment and supplies required Detailed step-by-step procedure Limitations and variables of the method Corrective actions Method validation Normal values and references QA Forms Accreditation standards for agencies require the facility to show documents on all quality control checks and other QA activities QA forms include equipment check forms and incident/occurrence report forms Equipment check forms Special forms for recording checks on tube additives, vacuum strengths and expiration dates – verification of new lot numbers Refrigeration temperatures – recorded daily Control checks on centrifuge – tachometer readings and maintenance performed Incident reports Must be filled out when a problem occurs Identifies the problem, state the consequence, and describe the corrective action Should not be used to place blame Should be used to ensure that the event does not reoccur