Combination HIV Prevention:
Crafting a New Standard for the
Long-term Response to HIV
Carlos F. Cáceres, Cayetano Heredia University/IESSDEH, Peru
Barbara de Zalduondo, UNAIDS, Switzerland
Timothy Hallett, Imperial College London, UK
Carlos Avila, UNAIDS, Switzerland
Michaela Clayton, AIDS Rights Alliance for Southern Africa, Namibia
“A sensible way to go…”
• “Combination Prevention”
highlighted in discussions in 2008
Conference
– See The Lancet Series 2008
• Increasingly regarded as the
‘sensible’ way to go
– 2008 Global Prevention Working
Group,
– 2009 UNAIDS Outcome Framework;
– 2009 Implementers Meeting;
– Global Fund Board 2009
recommendation;
– UNAIDS Prevention Reference
Group (PRG), 2009; etc
…but not a guiding principle yet!
• Yet still not a guiding principle applied systematically
in HIV programming
• Some doubts remain – is it anything new? Is it
necessary?
• Our goal today:
– Clarify concepts around Combination
Prevention
– Argue that structural interventions, including
human rights strategies, are core business of
HIV prevention
– Discuss how and why it can provide a
standard for a longer-term response to HIV.
What is Wrong with Prevention Now
Risk Groups
Risk
Practices
Vulnerability
Cultural
context
What is Wrong with Prevention Now
Most-at-risk
populations
Vulnerability
Individual
Cultural
context
Risk
Practices
…what is wrong? (2)
• Inconsistent application of
standards
– “Know Your Epidemic and
Response;” Know and engage
with key audiences; allocate
resources to suit Modes of
Transmission, etc.
– Lack of consensus on
approaches
• Fragmentation and
scatter
(see Bertozzi et al, The Lancet, 2008)
…what is wrong? (3)
• Focus on short-term results
– Research and programme evaluations with 6-36 month
follow-up
– Low-hanging fruit - preference for solving bite-sized
problems, neglecting the underlying causes of risk and
vulnerability (aids2031 Social Drivers Workgroup)
• Limited evaluation and cumulation of learning from
country programmes
– Limited investment in prevention evaluation research
– Confused language describing prevention aims and actions:
goal, activity, audience, setting, proximity of effect
Percent Spending in Programs focusing on Most-at-risk
Populations
(as a Percentage of Total Prevention Spending)
8.00%
7%
7.00%
6.00%
5.00%
Harm reduction programs for IDUs
Programs for MSM
Programs for sex workers and their clients
4.00%
3.00%
2.00%
1.00%
0.00%
Low level
Concentrated
Generalized
Source: UNAIDS HIV Expenditure Studies
Individuals
National/
Societal
Group/ Community/
Organizations
(women, girls,
children, men,
boys, transgender)
Relationships
Family/Partner
Individuals
(women, girls,
children, men,
boys, transgender)
What is Combination Prevention?
• Recapitulating: Analogy to combination treatment
Cited by Coates et al., 2008
Combining what?
• Type 1 – Common tactic combining two or more
intervention strategies
– E.g.. IDU: Needle & syringe programs + opiate substitution.
– E.g. US NIH “MP3” (methods for prevention packages program)
• Type 2 - Combining diverse strategies to fit the needs of
diverse sub-groups in the population
– E.g. strategies for MSM, trans, IDU, FSW, PMTCT, discordant couples
• Type 3 – Strategic combinations of biomedical, behavioral
and structural approaches to address key causes of HIV
risk and vulnerability for a particular population
– E.g. Synergistic interventions for interrelated sub-groups
– E.g. MSM: BCC, STI Tx, decriminalization, mobilization
– E.g. IDU: NSP, OSP, decriminalization, mobilization
UNAIDS Prevention Reference
Group Definition
• “The strategic, simultaneous use of different
classes of prevention activities (biomedical,
behavioral, social/ structural) that operate on
multiple levels (individual, relationship,
community, societal), to respond to the specific
needs of particular audiences and modes of HIV
transmission, and to make efficient use of
resources through prioritizing, partnership and
engagement of affected communities”
What Kind of Evidence is Needed?
Human Rights
Epidemiological
• e.g. Data from Modes
patterns and trends
of Transmission
Studies
Main drivers of
those epidemic
trends
Effective
Interventions to
address epidemic
patterns and their
drivers
• e.g. Specific forms of
social exclusion (class,
gender, sexuality) and
their confluence
• e.g. Effective
behavioral, biomedical,
structural interventions
Case et al., AIDS International Conference, 2010
Potential Effects Bringing Proven
Prevention Programmes to Scale
Status Quo
25M infections could be averted!
Scaled
Intervention
In GE: Circumcision, HTC, Treatment, Community Mobilization
In CE: Increase condom use and harm reductiong in MARPS
Biomedical, Behavioral, Structural
• Behavioral prevention
– Traditional prevention work: Behavioral change (from 11 to groups to behavioral change communication)
– Change individuals’ practices to reduce exposure and
infectivity
• Reduction of partners, condom use, use clean IDU equipment
• Biomedical prevention
–
–
–
–
Male circumcision
ARV prophylaxis (PMTCT. PEP)
Antiretroviral Treatment (ART)
Experimental: PrEP; ART-based microbicides,
vaccines
Structural Interventions
• Many definitions, many conceptual frameworks
– e.g collections in collections in AIDS 1995; AIDS, 2000; aids2031
Social Drivers Working Group.
• Focused on aspects of environment that increase people’s
vulnerability to HIV infection or decrease access.
• Body of work on Social Determinants of Health.
• Main types (from Robin Vincent, 2009):
– Changes in laws and regulations,
– Promoting changes in culture and social norms (e.g.
gender inequalities, HIV related stigma),
– Environmental enablers (e.g. increasing access),
– Community mobilization and empowerment,
– Policy dialogue and prevention diplomacy
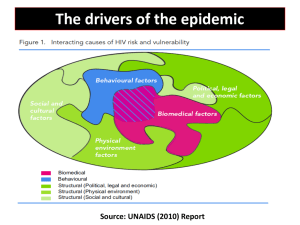
Interacting causes of HIV risk and vulnerability
Behavioural factors
Social and cultural
factors.
Biomedical
Political and
economic factors
SYNTHESIS
Gap Analysis
Biomedical factors
Physical environment
factors
17
Biomedical
Behavioural
Structural (Social and cultural, Political and economic; Physical)
Combination Prevention
Behavioural intervention
strategies:
Social and cultural
intervention strategies:
Behaviour change communication
School based HIV education;
•Community dialog and
mobilization
Peer-led advocacy and persuasion
•Advocacy and coalition building
for social justice
Influence cost of access to serviceds
Couseling
•Media and interpersonnal
communication to clarify values,
change harmful social norms;
Biomedical
•Education curriculum reform,
expansion and quality control
•Etc.
Political and
economic intervention
strategies:
•Human rights programming;
Intervention strategies
addressing physical
environment:
•Housing policy and standards
•Access to land; subsistence;
•Infracstructure development –
transportation,
communications, etc.
•Prevention diplomacy with leaders at
all levels;
•Community Microfinance/microcredit
Etc.
SYNTHESIS
•Training/advocacy with police,
judges;
GapBiomedical
Analysis intervention
•Engaging leaders
strategies:
•Stakeholder analysis & alliance
•Improved STI services; Appropriate &
building;
accessible clinical services; condoms
•Strategic advocacy;
•Opiod substitution therapy, detox;
•Regulation/deregulation;
•Male circumcision
•Etc.
•PMTCT services – ARV prophylaxis
(PEP, PrEP, Microbicides)
•ART for prevention
•Etc.
;
18
;
Biomedical
Behavioural
Structural (Social and cultural, Political and economic; Physical)
Human Rights: Beyond Rhetoric
• Ethical Principle: CP is a strategy to reach
Universal Access (Human Rights [HR]-based)
• Technical reason: Sound consideration of HR is a
necessary element of successful programs
– Lack of HR perspective may lead to program failure
• Condom use programming in Asia designed without
considering sex workers’ HR issues led to abuses and failure.
– Also need to face legal & HR-related structural barriers
– Good prevention planning starts with a HR analysis
– Insufficient to just ‘protect HR’ at implementation
• Testing promotion programs: Understand people’s needs + rights and
then design the best interventions within that framework.
– Environments protective of people’s rights unleash
community and individual motivation to avoid HIV
Ukraine: Reducing Police Violence
HIV Infections Averted By Structural Changes
1000
4 - 19%
800
600
3 - 9%
400
2 - 5%
200
0
662
343
209
Est for Odessa
Est for Makeevka
Est for Kiev
Elimination of police beatings
Strathdee, Hallett, Bobrova et al., Lancet 2010
Stigma Reduction can improve
PMTCT Outcomes
Per 100,000 women (assuming 15% prevalence at ANC)
Watts, Zimmerman, Eckhaus and Nyblade, 2010. Modelling the Impact of
Stigma on HIV and AIDS Programmes: Preliminary Projections for
Mother-to-Child Transmission. ICRW and LSHTM Working Paper.
Myths about Combination Prevention
Combination prevention
is “doing everything for
everyone”
It can’t be done
No! – that’s poorly
designed prevention!
Not so – IMAGE, Avahan, Stepping
Stones, Sonagachi
Need political courage to focus where the
need is
Need capacity to deliver to scale
HIV Prevalence Among Sex workers in Mysore
DATA
Fit with AVAHAN
intervention
removed
Estimated Impact
of intervention
“Best fit” projection
Source: Pickles, Foss, Vickerman et al., 2010
Beyrer et al, working paper
Peru: Political Courage and Community Mobilization
is Needed to Change the Epidemic’s Trajectory
Present level
100% MSM coverage
Null
Current
100% MSM interventions
Myths about Combination Prevention
It can’t be evaluated
True that it’s difficult to map and prove the
causal chain.
Easier to show effects at similar level of
proximity.
Need to better assess effects of programs that
include structural interventions.
Need Combination Evaluation!
True that measuring impact of any intervention
is difficult.
No reliable, validated, working test for HIV
incidence to compare combinations.
But – analysis of HIV prevalence can allow a
retrospective estimate of changes in incidence
in relation to programme and context.
Zimbabwe: Use of Modelling to
Assess Impact over Time
10
10
Natural decline in
incidence ~ 1990
HIVincidence
incidence(per
(per100pyar)
100pyar)
HIV
8
8
Accelerated
decline in
incidence, due
to behaviour
change: ~ 2000
6
6
4
4
2
2
0
0
1980
1980
1985
1985
1990
1990
1995
1995
Year
Year
2000
2000
Hallett, Gregson, Gonese, et al., Epidemics, 2009
2005
2005
2010
2010
Myths about Combination Prevention
It’s too expensive
Compared to what?
The missing pieces are often the structural
interventions. Contrary to common perception,
the additive costs can be quite reasonable.
Synergies.
Economies of scale
Human rights (HR) services are 1.4 % of
ART programme costs in South Africa
Source: Jones et al: Human Rights Costing of HIV for
Prevention in a Southern African Setting. Poster at aids2010.
• Charlotte watts/ICRW slide (
Watts, Zimmerman, Eckhaus and Nyblade, 2010. Modelling the Impact of
Stigma on HIV and AIDS Programmes: Preliminary Projections for Motherto-Child Transmission. ICRW and LSHTM Working Paper.
http://seofrecencaricias.blogspot.com
Structural Interventions “float all boats”
Gender
Equity
effects
Sexual
Inclusion
Effects
Poverty
Reduction
Effects
HIV
effects
Social Change Takes Time – START NOW!
Results in 1-2
years
Results in 3-5
years
Results in > 5
years
e.g. Knowledge of HIV
prevention, Awareness
of risks of Multiple
concurrent partners,
supportive professional
and workplace policies
e.g. Supportive
community
attitudes,
Enforcement of
supportive
policies
Programmes have focused on those, shortterm results for 25 years!
UNAIDS Social Change Communication Working Group, 2008.
More
Equitable
Gender
Norms
Positive Health, Dignity and Prevention
"Positive health, prevention and dignity highlights the
importance of placing the person living with HIV at the
centre of managing their health and well-being, within the
sociocultural and legal context in which they live. It also
stresses the importance of addressing prevention and
treatment simultaneously and holistically and emphasizes
the leadership of people living with HIV in responding to
policy and legal barriers and in driving the agenda
forward.“
Kevin Moody, Director and CEO, GNP+
Challenges
• Need better tools to ‘know our epidemics’
– Ascertaining incidence, size estimations
– Standardizing terminology
• Need more evidence about our responses
– Insufficient data on what works, contradictions,
how to improve conceptualization of CP
– What combinations are necessary and sufficient
in specific settings? Coverage, intensity?
Take-Home Messages
• Focus on individuals for prevention (w/biomedical
and behavioral approaches) is not sufficient
• CP is not about implementing rigid panel of
redundant/irrelevant interventions.
• Rather, CP is strategic, evidence-informed,
combination of biomedical, behavioral and
structural strategies in a HR framework.
• Investing in structural interventions is not only an
ethical obligation – it is a worthwhile investment
• Needed for a sustained, long-term response
• A flagship of a “prevention revolution”!
“The successful implementation of HIV interventions
therefore demands, first of all, that local-level barriers be
addressed and that an ‘enabling environment’ be created.
This is not difficult to achieve.
Often, what appears to be intractable resistance to
respecting the basic rights of most-at-risk groups yields to
thoughtful advocacy and bridgebuilding with local
authorities and powerbrokers.”
Commission on AIDS in Asia. 2008. Redefining AIDS in Asia: Crafting an Effective
Response. Report of the Commission on AIDS in Asia, . New Delhi, India: Oxford
University Press
Acknowledgements
•
•
•
•
•
•
•
•
•
•
B. Zalduondo, T. Hallett, C. Avila, M. Clayton
K. Daly (ICASO), K. Thomson (UNAIDS)
All authors who shared their work with us
C. Beyrer et al. (JHUSPH/WB)
Auerbach et al, 2009 (aids2031)
Social Drivers Workgroup, aids2031
Sam McPherson (International HIV Alliance)
UNAIDS Prevention Reference Group
WHO HIV Department
IESSDEH and USSDH/Cayetano Heredia University
Thanks!