Children with Neurodisability
advertisement
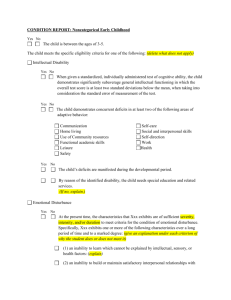
Children With Neurodisability Dr Lesley McDonald Community Paediatrician West Centre Community Child Health • 0-19 years • wide range of developmental difficulties / • • • • • disabilities holistic approach partnership with parents multidisciplinary working interagency working communication Settings • Child development centres 0-5 years • Mainstream school health • MLD schools • Complex needs schools • EBD schools Child Development Centres • West Centre (West) • Bridgeton (East) • Glenfarg (North) • Southbank (South) Referrals • ODER one door entry referral • referrals from GP, HV, RHSC, nursery, educational psychology • referral centres for specialist developmental assessment • links with other agencies – education, social work The team around the child Paediatrician specialist health visitor admin staff clinical psychology Child and family physiotherapy social work resource team occupational therapy Other CDC services dietician neurologist geneticist CDC community autism team orthoptist speech and language therapy CDC links educational psychology home visiting audiology teachers CAMHS social work area teams PACT nurseries CDC GP health visitor RHSC RHSC therapists paediatricians Children with additional needs • ex – preterm • autism • Down’s syndrome • early developmental impairment (“global developmental delay”) Ex – preterm infants • EPICure study • infants <26weeks gestation • at 2 ½ 49% no disability 24% disability not severe 24% severe disability 2% died 1% no data Ex-preterm infants • at 6 years unimpaired 20% mild disability 34% moderate disability 24% severe disability 22% boys more likely to have moderate or severe disability cognitive impairment most common of the domains assessed Neonatal follow up • until 2 years corrected • referral to CDC at any time if concerns • if not, review at 3, 5, 7 • important for primary care to refer to secondary level services if concerned Autism • SIGN guidelines • multidisciplinary specialist assessment • Community Autism Team in Glasgow • ICD 10 criteria General “warning signs” - preschool • delay or absence of spoken language • lack of awareness of / responsiveness to others, unable • • • • • • • to share pleasure lack of pretend imaginative play qualitative impairment in non-verbal communication lack of pointing lack of gaze monitoring lack of initiation of activity or social play unusual or repetitive hand and finger mannerisms unusual reaction to sensory stimuli General “warning signs” – school age • communication impairments – – – – – – abnormalities in language development odd intonation, pitch etc persistent echolalia reference to self as “you” “she/he” beyond 3 unusual vocabulary limited use of language for communication and / or tendency to talk only about specific topics General “warning signs” – school age • social impairments – inability to join play, or inappropriate attempts – lack of awareness of classroom “norms” – easily overwhelmed by social and other stimulation – failure to relate normally to adults – extreme reactions to invasion of personal space General “warning signs” – school age • impairments of interests, activities, behaviours – lack of flexible cooperative imaginative play / creativity – inability to cope with change or unstructured situations – odd behaviours including unusual responses to sensory stimuli Down’s syndrome • recommended schedule of health checks • developmental progress slower than other children 1. Heart Disease • by 6 weeks – examination and echo – or examination, CXR and ECG at birth and 6 weeks 2. Thyroid • 10-20% affected, any age, diagnosis difficult • low threshold for testing • preventable impairment if untreated • Guthrie at birth • T4 TSH thyroid antibodies at 1 year – normal: repeat 2 yearly – increased TSH or Ab’s: repeat 6-12 monthly 3. Eyes • increased squint, cataract • check carefully in first year, refer if concerns • second year: full assessment, orthoptic, refractory, fundoscopy – abnormal: close follow up by ophthalmology – normal: full review at 4 including vision, 2 yearly thereafter 4. ENT • • • • • • • • conductive hearing loss 60-80% SNHL 20% by age 20 partial upper airway obstruction sleep apnoea catarrh neonatal hearing screening audiology annually until age 5 2 yearly thereafter 5. Growth • short stature part of syndrome • 0-2 years: check wt, ht, OFC frequently • >2 years: check annually • use both Downs and standard growth charts • red book should have Downs insert 6. Others • atlantoaxial instability – no screening procedure – do not bar from sports – at risk: GA, RTA – refer • neck pain / pain behind ear • abnormal head position • deteriorating head position • loss of bladder / bowel control Early developmental impairment (EDI) • formerly known as global developmental delay • unhelpful term, implies difficulties temporary and will “catch up” • EDI a more appropriate diagnostic term, proposed at international consensus conference in 2008 EDI definition • persistent significant limitations in two or more developmental domains – motor – communication – cognitive skills – social skills – emotional regulation / behavioural skills – self care skills • onset before age 5 • not better explained by another established developmental disorder • reassess by school age or before age 9 to review diagnosis Assessment • history • examination • developmental assessment • investigations as appropriate • multidisciplinary working • follow up over time • exciting advances in genetics and neuroimaging Summary • wide range of disabilities which may be encountered in general practice • awareness of services available • if in doubt, phone to discuss Contact Numbers • West 207 7100 • Bridgeton 531 6550 • Glenfarg 531 6191 • Southbank 201 0923