Current Thinking about Family Therapy and Systemic Interventions
advertisement
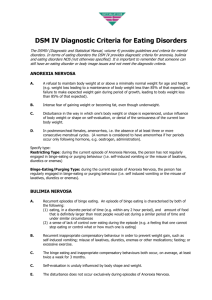
Current Thinking about Family Therapy and Systemic Interventions with Eating Disorders Facilitator: Lesley Novelle Workshop format • explore common themes across current research studies and any gaps • explore facets of multi-disciplinary working within a systemic frame • Consider from a family perspective What it is not? • The answer! • Comprehensive , looking at what families might say within the literature and the approach , Method, Technique of current studies, not looking any further afield than systemic texts (at this point) Context • Year one of a four year taught Doctorate, produce a comprehensive literature review before development of a research proposal • Family Therapy team as part of MDT approach • Providing justification for further study (or changing the focus) • Why am I interested? • Please share what interested you in coming today NICE Guidance and Junior Marsipan • Systemic invitation not just in terms of family interventions but also working together as “systems of concern”. Search Strategy • Key words: – Eating (disorder), Anorexia, Bulimia (very tight) EBSCO, Psychinfo • Only systemic journals, results from: – Journal of Family Therapy – Family Process – Australian and New Zealand Journal of Family Therapy – Journal of Marital and Family Therapy – Journal of Feminist Family Therapy – American Journal of Family Therapy – Contemporary Family Therapy Systemic Literature Some key ideas emerging from the texts: • Using families as a resource • Considering both conjoint family work and separating out different sub systems. • Multi-modal, multi-family groups • Strengthening parental position and decision making • Externalising the Eating problem • Long term and tricky 3-4 years duration Some statistics • USA (Hudson et al , 2007) Downs and Blow (2013) – 1.2% individuals experience Anorexia Nervosa – 2% experience Bulimia Nervosa – 5.5% Binge Eating Disorder – Little evidence to suggest that families “cause” eating disorders, some evidence to suggest family patterns can maintain. Eating disorders can dominate family functioning and intensify previous patterns. Quote “The impact of the illness on the family is immediately evident through the influence that the symptoms hold within the household. Just as issues around food, eating and weight dominate the sufferer’s thoughts and behaviours, food may also take a predominant role within family life and interactions” Whitney and Eisler (2005, p,577) in Downs and Blow (2013) Emerging from the development of the last 18 years in particular WHICH MODELS? Maudsley model • Inspired by the work of Salvador Minuchin (1975, 1978), Palazzoli et al (1978), in Downs and Blow (2013) Primarily focused on Anorexia Nervosa • Three tasks: – Gaining and maintaining family co-operation by intensifying the need to treat the disorder. (removing blame and shame) – Assess the organisation of the family, what alliances, boundary and control techniques are used – Establish interventions to help the family in the creation of change • Three Phases – Getting parents to work together, empowering to gain control over weight gain and weight restoration – Focus on helping adolescent to begin to eat on own – Family work to help young person to gain back control of thier eating (life) Multi-family groups • No quantitative studies but a number of case study write ups. • Multiple family groups, four families in one study Colahan and Robinson (2002) • Multiple interventions with all four families, using roles in family, treatment modalities and shared mealtimes. • Adaptation of Maudsley model looking at parent to parent support as adjunct. • Downs and Blow (2013) suggest this as an area for further study. Family Based Treatment • Girz et al (2013) Adolescent day treatment (Canada) – Parents check in with FT after weekend – FT holds conversation with parents after weekly team rounds – Re-entry meeting if extra support needed – Parents and children weekly FT sessions – Parents and children attend MFT evening – Parents involved in setting family transition plans (food and non-food related) Conjoint or Separated Family Therapy • Discussion in the literature about family based interventions and their delivery. Eisler et al (2000) (not published in FT literature) • Links to some of the earlier work with a psychoanalytic/systemic theory base. • 40 adolescent “patients” assigned to either: • Conjoint: Family and young person • Separated: Parent (and siblings?), young person separate. • Outcomes: – High levels of maternal criticism- Separated Family Therapy, better outcomes – Symptomatic change was more evident in the Separated Family Therapy whereas emotional change was more highly reported in the Conjoint Family Therapy. – Also significant changes in family measure of expressed emotion and critical comments between parents and young people were significantly reduced as was so between parents. Warmth between parents increased. Family members voices • Weak or quiet with some exceptions • Located in questionnaires and outcome measures • What is their narrative? • Downs and Blow (2013) , lack of literature about the role or support of siblings Exercise • This may be quite a challenging and emotional exercise, please look after yourself and one another and only share what you feel you would like to share. • There will be people in the room who have experienced eating problems, please be mindful. • Purpose of exercise is to: • Allow room to hear a family perspective • To consider any incoherence • To consider the best next steps from a family based intervention perspective. Vignette • Family: White British, Young woman aged 14, Mother aged 41, Father aged 45 , younger brother aged 12 • Primary care group: Practice nurse, GP , Health Visitor, School • Camhs team: Care co-ordinator, family therapist, Psychiatrist, MAT practitioner, 3rd sector support organisation. Instructions • Form in to groups as identified. Do not confer until all of boxes completed. • Using paper with six boxes follow instructions read out and make a mark or representation in each box which represents the instruction. • Now share your thoughts and experiences of the exercise in the group paying particular attention to feelings and then next steps (boxes 4 and 6). • Agree how you will feedback to the larger group. Feedback • What was it like doing the exercise, is everyone ok? • What next steps emerged, talk from each group to the other groups in turn? • What dilemmas, concerns, exciting ways forward emerge? Six instructions • • • • • • Family -mark the paper to represent relationship with your daughter/Sister. Drawing lines, dots and squiggles. Goal: mark the paper to represent your goal with this person. Where do you see yourself headed? Obstacle: marks the paper to represent what is getting in the way of achieving the goal. Counter –transference- mark the paper to represent her feeling about young person. Theories- mark the paper to represent what you know theoretically about this situation. What are the possible causes and context of your struggle? Next steps- mark the paper to represent what their next steps will be with this work. What do they envisage in the future? Early family intervention • Focus on preventing further weight loss/destructive behaviours. • Support parents; work with parental authority and responsibility. • Strike a balance between making it clear that the eating problem is unwelcome and acknowledging that it is functional • Use family and individual strengths • Keep young person linked to their world Family Therapy, what we are discovering Approach • Consider who is the client Dare (1997) • In involving parents and other family members what “approach” do you have • Contract ( bearing in mind safety and motivation for change) • Family culture respected • Current goals • Life cycle issues • Privacy and transparency • What is the impact on siblings, what is the forum for them to share • Both directive and collaborative? (outcome from narrative in studies about different experiences of treatment) • Clear and well co-ordinated , regular care plan reviews • Collaborative adaptable engagement with current system • Score- measuring progress across a number of domains Methods How we intervene • Structured family therapy- reflecting team • Family input in home-purpose? • Consultation • Educational and practical input • Explore needs of all family members • Use of a reflecting team approach • Individual work in the “presence of” • Joint team approach to care planning- are we stronger than the eating problem Techniques • • • • • • • • • • • Collaboration and transparency re goals/contract- write Engagement- key area and linked to approach/careful attention to contract Voices to be heard Explore resilience and strengths Teach, role play, enact, play, toys and tech CBT Develop rituals for talking, building on family strengths Develop a genogram as a tool Outcome measures Timing- when and how to intervene Within sessions– Sculpting – Externalising – directives/coaching – enactment – intensification Some ideas about ways forward • Remember that Anorexia is very powerful and can organise us all to do things we might otherwise not consider e.g. feelings, actions • Use people close to the person experiencing the problem as a resource. “System of Concern” • Consider the risk and the dilemmas associated with “consent”- but be open to possibilities References • • • • • • • Journal articles: Colahan, M. Robinson, P.H., (2002) Multi-family groups in the treatment of young adults with eating disorders. Journal of Family Therapy, Vol 24, pp. 17-30 Downs, K.J. and Blow, A.J., (2013) A substantive and Methodological review of the family-based treatment for eating disorders: the last 25 years of research. Journal of Family Therapy. Vol.35:51:p3-28 Eisler, I., Dare C., (2000) Family Therapy for Adolescent Anorexia Nervosa: The results of a Controlled Comparison of Two Family Interventions. Journal of Child Psychiatry, Vol.41, pp. 727736 Griz, L., Robinson, A.L., Foroughe, M., Jaspewr, K., Boachie, A., (2013) Adapting family-based therapy to a day hospital programme for adolescents with eating disorders: preliminary outcomes and trajectories of change. Journal of Family Therapy, Vol.35:51 pp.102-120 Minuchin, S., Baker, B.L., Rosman, B.L., Milman, L., Todd, T.C., (1975) A conceptual model of psychosomatic illness in children:family organisation and family therapy. Archives of General Psychiatry, Vol.32, pp. 1031-1038 Minuchin, S., Rosman, B.L, Baker, B.L, (1978) Psychosomatic Families: Anorexia Nervosa in Context. Cambridge, M.A.: Harvard University Press. Palazzoli. S.M. (1978), Self-Starvation: from individual to Family Therapy in the Treatment of Anorexia Nervosa. Trans. Pomerans, A. New York: Jason Aronson. References Grey literature • • Junior MARSIPAN: Management of Really Sick Patients under 18 with Anorexia Nervosa. Royal College of Psychiatrists, College report, January 2012 http://www.rcpsych.ac.uk/files/pdfversion/CR168.pdf accessed 28.8.13 National Institute for Clinical Excellence: Eating disorders Core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders Clinical Guideline http://www.nice.org.uk/nicemedia/live/10932/29218/29218.pdf accessed 29.7.13 • Burnham, J. (1992). Approach, Method, Technique: Making Distinctions and Creating Connections. Human Systems: The Journal of Systemic Consultation and Management. Vol 3, p3-26 • See hand out for references over last 20 years