Treatment for Depression
advertisement

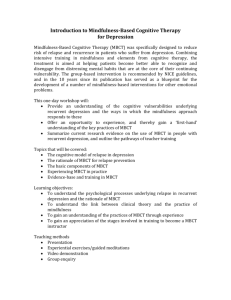
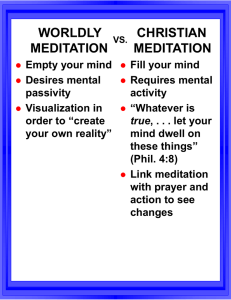
Treatment for Depression ~ Mindfulness Meditation ~ Meditation Meditation is an old eastern practice dating back to 2500 years ago, but in the last 40 years, has attracted considerable professional and popular interest and, with the growth of holistic medicine and wider concerns with fitness, health, and emotional well-being, it continues to be attractive as a means of natural and healthy development. About the Intervention Mindfulness is a particular way of paying attention, in the present moment and nonjudgmentally (Kabat-Zinn, 1994). The goal of MM practice is simply to experience what is present from moment to moment and one eventually learns to face and work with the full range of human emotions and mind states. Duration: Eight-week training program that requires an immediate and significant lifestyle change most readily seen in the need to devote a minimum of 45 minutes per day, six days per week to practicing the various forms of meditation and yoga assigned for ‘homework’ About the Intervention MBCT is based on an integration of aspects of CBT for depression (Beck et al., 1979) with components of the mindfulness-based stress reduction program developed by Kabat-Zinn and colleagues. The Cognitive view of Depression builds on the basic observation that how people think can have a profound influence on how they feel and behave. Unlike CBT, there is little emphasis in MBCT on changing the content of thoughts; rather, the emphasis is on changing awareness of and relationship to thoughts Movie ~Healing From Within~ Based on Jon Kabat-Zinns approach/procedure to Mindfulness Meditation Research Article Prevention of Relapse/Recurrence in Major Depression by Mindfulness-Based Cognitive Therapy (Teasdale et al., 2000) Study evaluated mindfulness-based cognitive therapy (group intervention) designed to train recovered recurrently depressed patients to disengage from depressogenic thinking that may mediate relapse/recurrence. Why is prevention of relapse important? Patients who recovered from a first depressive episode have about a 50% chance of developing a new episode, whereas the risk of recurrence is 7080% for those who have a history of two or more depressive episodes. Also, for about 6- 13%, depression becomes chronic and every new episode just becomes more and more lethal. Study Information Participants: n= 145 random recovered recurrently major depressed patients Recruited from community health care facilities and by media announcements at three different sites: predominantly rural, Welsh speaking area of north Wales, city of Cambridge, England, and metropolitan area of Toronto, Ontario Inclusion criteria: -18-65 years of age -met DSM III-R criteria for a history of recurrent major depression -a history of treatment by a recognized antidepressant medication , but off antidepressant medication for at least 12 weeks Study Information Patients who currently practiced yoga more than twice a week were excluded Relapse/recurrence to major depression was assessed over a 60 week study period: 8 week treatment phase followed by a 52 week follow up phase Two baseline variables: -recency of recovery from last episode of depression (within 0-12 months prior to randomization vs. within 13-24 months prior to randomization) and number of previous episodes of MDD ( two vs. more than two) - both these variables have been found to be related to the risk of relapse/recurrence in previous studies (Evans et al., 1992) Study Information Treatment: Treatment as usual patients were instructed to seek help from their family doctor, or other sources, should they encounter symptomatic deterioration . MBCT patients were taught skills that allow individuals to disengage from ‘habitual’ dysfunctional cognitive routines, in particular depression-related ruminative thought patterns , as a way to reduce future risk of relapse and recurrence of depression. Study Information MBCT program delivered by instructor in eight weekly 2hour group training sessions, which included daily homework exercises Homework: some form of guided (taped) or unguided awareness exercises, directed at increasing moment by moment nonjudgmental awareness of bodily sensations, thoughts, and feelings with exercises designed to integrate application of awareness skills into daily life Findings: For patients with 3 or more previous episodes of depression (77% of the sample) MBCT significantly reduced (almost halved) risk of relapse recurrence rates compared with TAU For patients with only 2 previous episodes, MBCT did not significantly reduce relapse/recurrence History= age at admission to study minus age of first onset yielded a mean for those with three or more episodes approximately four times as great as that for patients with two episodes Limitations: The key outcome of interest in this study was the prevention of a future event rather than reduction of symptoms present at baseline assessment No evidence to show if similar effects would be obtained with different ethnic or educational backgrounds Study used only individuals with Major Depressive Disorder, thus not taking into account those with Bipolar Disorder, who are generally more likely to try or to commit suicide Group therapy and not individual Background In comparison with drop-outs, those who maintain meditation practice show significantly greater decreases in depression over 1 year (Fehr, 1977). A group of long term meditators (with 43 months of TM experience) showed a significantly lower level of depression than the short-term (6 weeks) meditators. However, in this study, the subjects were not randomly assigned to meditation and control groups, and so the longterm meditators may already have had relativiely low levels of depression before learning TM (Ferguson and Gowan, 1976). Neurobiology of Disorder Several brain neurotransmitter systems have been implicated in depression and mania: glutamate, serotonin, norepinephrine, and dopamine With the use of neuroimaging studies depressed patients have shown several abnormalities of regional cerebral blood flow and glucose metabolism in various brain regions, including the limbic cortex, the prefrontal cortex, the hippocampus, the amygdala, and the anterior cingulate cortex Neurobiology of Disorder hippocampus/cingulate gyrus- involved in learning and memory amygdala- only part of limbic system responsible for emotional responses -other areas involved with learning and memory of emotions prefrontal cortex- formulation of plans and strategies Neurobiology of Disorder The approach of CBT developed by A.T Beck initially grew out of clinical observations of depressed patients. Consists of 3 components: 1. 1.Negative automatic thoughts 2. 2. Systematic logical errors 3. 3. Depressogenic schema 4. Combination of negative expectations about oneself and one’s future and the rigid thinking that lies behind cognitive errors causes depressed people to misinterpret events in their lives, which make it more likely that a sad mood will follow Neurobiology of Disorder These reactivated patterns of thinking can act to maintain and intensify the dysphoric state through escalating and self-perpetuating cycles of ruminative cognitive-affective processing( Teasdale, 1988, 1997). Studies have compared patterns of thinking activated by mild dysphoria in those with and without a history of major depression and can explain difference through episode sensitization and kindling. Mindfulness: Its focus is to teach individuals to become more aware of thoughts and feelings and relate to them in a wider decentered perspective as ‘mental events’ rather than as aspects of the self or as necessarily accurate reflections of reality. Evaluation Advantages: -Does not pose serious side effects (ex. Lithium) -Many antidepressant medications have significant side-effects -MBCT offers a promising cost-efficient psychological approach to preventing relapse/recurrence in recovered recurrently depressed patients -M-based stress reduction approach is generic and thus can appeal to and be of significant relevance and benefit for a wide range of people (patients dealing with heart disease, HIV, anxiety, depression) Evaluation Disadvantages: -Most episodes of depression will improve within a few months even if untreated, thus effective treatment must show results sooner, therefore great reliance on many pharmacological treatments -Since meditation is a self-directed and active process, it may not be readily dispensed , like medication, to depressed patients if they show little motivation to practice -Therefore, the value of meditation is greater for those people who want to be directly involved in their development than those who want to be ‘cured’ Conclusion MBCT appropriate because reviewing studies of lifetime course of depression, a recent commentary concluded that ‘it has been established that unipolar major depressive disorder is a chronic, lifelong illness, the risk for repeated episodes exceeds 80%, patients will experience an average of 4 lifetime major depressive episodes of 20 weeks duration each (Judd, 1997) For patients with 3 or more previous episodes of depression (77% of the sample) MBCT significantly reduced (almost halved) risk of relapse recurrence rates compared with TAU Conclusion Does CBT need to be combined with antidepressants in order to be effective with severely depressed outpatients? -16 weeks of CBT produced a 1 year follow up success rate that equaled or slightly exceeded that achieved by a full year of antidepressant treatment , and CBT’s maintenance effects were clearly superior to short term(16 weeks) Conclusion About one third of MDD patients will not respond favorably to the first psychosocial treatment We know through crossover studies that many individuals who fail on one antidepressant will experience treatment gains when switched to a different medication No present empirical data to guide clinicians providing psychotherapy for patients who have failed to improve following an initial psychosocial intervention Conclusion MM based clinical interventions may hold considerable therapeutic promise, either alone or in combination with other forms of intervention