decisions1
advertisement
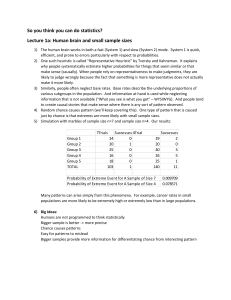
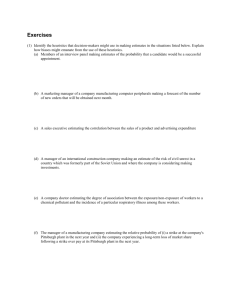
Clinical decision making Carl Thompson UK, Centre for Evidence Based Nursing Editor, Evidence Based Nursing www.ebn.bmj.com This session Integrating research evidence with preferences and contextual information When should intuition and more structured approaches be used? The ways people think and make choices What’s right and wrong with clinical experience? Tools and techniques: decision analysis, cognitive approaches How do nurses (and doctors) think they think? 1. Make sense of multiple cues 2. Diagnose or assess 3. Treat or intervene 4. Evaluate progress 5. Treat some more if needed Errr… start again… How do they actually think? The theory – cognitive continuum Hamm,R (1988) in Dowie & Elstein, Clinical Judgement and decision making, Cambridge University Press Heuristics and Bias Daniel Kahneman and Amos Tversky (d. 1996) Tversky and Kahneman, Judgment Under Uncertainty: Heuristics and Biases, Science (1974), Vol. 185, pp 1124-1131 The Need to Assess Probabilities People need to make decisions constantly: diagnosis and therapy Thus, people need to assess probabilities to classify objects or predict various values, such as p (DISEASE|SYMPTOMS) People employ heuristics to assess probabilities heuristics lead to significant biases, CONSISTENTLY This observation leads to a descriptive, rather than a normative, theory of human probability assessment “Getting” healthcare is not easy Pattern recognition is easier if you have experience Experience: A problem of perception Slide from Slawson, Shaughnessy, Becker, 1999. Do you see the Dalmation in the picture? Moral: Clinical experience sometimes helps see, sometimes prevents seeing the right picture Now that you see it, can you try to not see it? Moral: Experience can result in ideas that are difficult to change One learns the basic patterns One sees them in new situations. Then one can see the pattern where before it had been confusing. Time and nursing decisions Once every 30 seconds in critical care (Bucknall, 2000) Circa 50 decisions every 8 hour shift in Medical Admissions (Thompson et al. 2001 – 2005) 5 judgement or decision challenges per consult for health visitors. Remember uncertainty? How do we normally respond? Experiential/internal knowledge Very limited textual information use and for certain kinds of decisions (British National Formulary and local protocols) 90 hours of primary care = 1 telephone call 180 hours of acute care (1080 decisions) = local protocols x4 times, BNF x50 times). ‘sophistication’ and technology doesn’t matter (Randell et al. 2007). Demography and biography poor predictors of use The five classic decision pitfalls Representativeness rate neglect Availability Overconfidence Confirmation Illusory correlations and base What can we do? Think about decision structure, time & visibility Be aware of base rates Consider whether information is truly relevant and not just salient Seek reasons why you may be wrong and entertain alternatives Ask questions that may disprove, rather than confirm, your current hº You are wrong more often than you think