Assessment and Formulation Case Presentation
advertisement

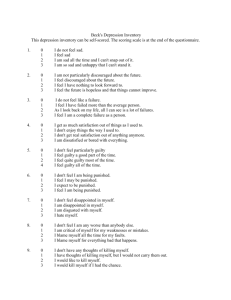
Assessment and Formulation Case Presentation Natalie Davies Alice Referral information •23 year old female •History of depression and self harm whilst at university 3 years ago •Depression had returned in the last 3 months, along with thoughts of self harm •Living with father and step-mother, after being evicted from the family home along with her mother and sister •Prescribed 50mg Lustral (Sertraline) Presenting Issues • Depressive symptoms improved however... ...on further exploration, still occasionally experiencing: – Low motivation – Tiredness – Social withdrawal – Self-critical thoughts • DSM –IV criteria Assessment tools • IAPT Minimum Data Set – PHQ9: 11 (Moderate) – GAD7: 5 (Mild) – WSAS: 20 (Significant impairment) – Phobia 1: 2 – Phobia 2: 1 – Phobia 3: 0 • Disorder specific measures Other factors • Medication – Sertraline 100mg 6 weeks prior to assessment • Risk – No thoughts of self harm or suicide (score of 0 on PHQ9 question 9) – No risk of neglect – No risk of harm to/from others Hot cross bun (Padesky & Mooney, 1990 ) Situation At home with step-mum Cognitive “what’s the point in getting up?” Physical Tired, insomnia, sleeping in the day Mood Sad Numb Behaviour Stay in bed, on laptop or watch TV Hot cross bun (Padesky & Mooney, 1990) Situation Meeting someone new Cognitive “I want to be someone different” “I’m not normal” Physical Butterflies in stomach, faster hear rate Mood Anxious Behaviour Tell lots of jokes, say “I sound weird” out loud Predisposing factors • Father left at age 9 • Mother “stopped caring” at age 11 – Home felt “unstable and unsafe” • Mother harsh and critical towards Alice Precipitating Events • Evicted from home, went to live with father and step-mother – Step-mother critical • First serious relationship ended Goals Westbrook, Kennerley, & Kirk, 2007 “To feel better about myself and have more self belief “ (Long Term) Refined in session 2: •To accept compliments (Short Term) •To do a stand-up comedy gig in London (Medium Term) •To stick up for myself more when my step-mum shouts at me (Medium Term) •To be myself and be more relaxed on dates e.g. telling less jokes (Medium Term) Longitudinal Formulation (Beck et al, 1979) Early experiences Dad left when 9 years Mum became neglectful at 11 years Core Beliefs I’m unlovable I’m abnormal Assumptions/Rules I can protect myself from the pain of rejection if I don’t let people get close People only accept you if you’re normal In order to be accepted I must not show the real me Compensatory strategies Don’t let anyone get close Tell someone everything about me that’s “abnormal” straight away Use of humour to detract from the “real me” Critical Incident Broke up from first serious girlfriend Moved in with Dad and Step-Mum Trigger Date doesn’t go well, reminder of ex NATs “It’s because there’s something wrong with me” “I’ll be alone forever” Emotion Depressed, Lonely Physical Tired, tearful, low motivation Behaviour Stop going on dates, use humour more in interactions, withdraw from friends Which model? • Beck et al’s (1979) cognitive model of depression – identified assumptions and core beliefs – developed as a result of early experiences – rigid assumptions, resistant to change – NATs triggered, which lead to depressed mood and social withdrawal Low Self Esteem? – Schemas in cognitive model of depression (Beck et al, 1979) similar to self esteem i.e. “they are a product of learning and, once in place, they in turn shape how a person perceives and makes sense of subsequent experiences” (Fennell, 1997, p. 2) – Low self-esteem may i) represent an aspect of a presenting issue ii)be a consequence of a presenting issue or iii) represent a longstanding vulnerability factor, preceding the onset of presenting issues Cognitive Model of Low Self Esteem (Fennell, 1997) Activation of Bottom Line A first date Depression Predictions “I’m abnormal, I won’t be accepted if I am myself” Self critical thoughts “there’s something wrong with me, I’ll be alone forever Anxiety Confirmation of Bottom Line Maladaptive Behaviour Use of humour Proposed Treatment Plan Aim Method Socialising Alice to the CBT model Completion of hot cross buns and cross-sectional formulation Challenging Alice’s self critical thoughts Completion of thought diaries Testing Alice’s assumption that she has to behave how she thinks others want her to in order to be accepted or loved Exploring consequence of belief, advantages and disadvantages, identify alternative rule, behavioural experiments Test Alice’s belief that she is abnormal Continuum work Engagement and Therapeutic Alliance • Engaged Well – Socialised to CBT model – Contributes to session • Alliance very good from the start – Open, honest, friendly • However, too many jokes? – Eliciting emotion- avoidant? Experience & Observe (Kolb 1984 and Lewin 1946) Situation Aware of client making many jokes in therapy session Cognitive “If I raise this it will be really awkward” “I’ll come across as really formal” Physical Butterflies, heart rate increased Mood Anxious Behaviour Avoided bringing this up in conversation Reflection –Assumptions related to valuing humour in sessions –I didn’t fully consider the potential impact on the emotional expression in the session –There is a need to validate my clients experiences, even if she isn’t? Plan Use of humour is advantageous to the therapeutic alliance where appropriate, but can become a barrier to eliciting emotions Summary • Presenting issue of mild-moderate depression, with a previous episode of depression 3 years ago • Assumptions/rules led to compensatory behaviours which became self-perpetuating • Treatment plan aimed at increasing confidence through reducing compensatory behaviours and testing assumptions Questions?